Overcoming Cancer Health Disparities Through Diversity in Cancer Training and Workforce
In this section, you will learn:
- Racial and ethnic minorities are considerably underrepresented in the cancer research and care workforce.
- It is imperative to prioritize investment in early-career researchers to enhance diversity and improve equity in the workforce.
- Diversity-focused training has improved inclusion within the cancer research and care workforce; however gaps remain throughout the cancer research training path.
- Improved support from medical research mentors and peer groups is needed to support diverse researchers and address cancer health disparities.
Complex, interrelated factors contribute to cancer health disparities (see Factors That Drive Cancer Health Disparities). Although the overall health care workforce has become more diverse (796)Salsberg E, Richwine C, Westergaard S, Portela Martinez M, Oyeyemi T, Vichare A, et al. Estimation and Comparison of Current and Future Racial/Ethnic Representation in the US Health Care Workforce. JAMA Netw Open 2021;4:e213789. [LINK NOT AVAILABLE], diversity in the cancer research (797)Westring AF, Sammel MD, Speck RM, Tuton LW, Grisso JA, Abbuhl SB. Career Trajectories of Women from Underrepresented Minority Groups at an Academic Medical Center. JAMA Netw Open 2021;4:e212723-e. [LINK NOT AVAILABLE] and care workforce (798)Lang JJ, Issa R, Lombardi C, Garcia E, Oke OC, Ekwenna O. Trends in Race and Ethnicity among Matriculants to US Oncology Training Programs, 2015-2020. JAMA Netw Open 2021;4:e2128530-e. [LINK NOT AVAILABLE] still lags behind trends in the general U.S. population. A proposed strategy to overcome cancer health disparities and achieve health equity is to diversify and support the cancer research and care workforce (799)Wilbur K, Snyder C, Essary AC, Reddy S, Will KK, Mary S. Developing Workforce Diversity in the Health Professions: A Social Justice Perspective. Health Professions Education 2020;6:222-9. [LINK NOT AVAILABLE]. Diversity is generally defined as the full range of human similarities and differences in group affiliation including gender, race and ethnicity, social class, role within an organization, age, religion, sexual orientation, physical ability, and other group identities (CDPR). In June 2021, Executive Order 14035 “Diversity, Equity, Inclusion, and Accessibility (DEIA) in the Federal Workforce” established a working DEIA framework for the federal government(800)The White House. Government-Wide Strategic Plan to Advance Diversity, Equity, Inclusion, and Accessibility in the Federal Workforce. [updated November 2021, cited 2022 April 22].. The identified DEIA priorities and guidance seek to increase representation and promote fair treatment of people regardless of race, ethnicity, sexual orientation, gender identity, physical ability, religious beliefs, or community background. This federal initiative can be applied to the Science, Technology, Engineering, Mathematics, and Medicine (STEMM) career pathway that prepares current and future students and health care trainees for successful careers in cancer research and care. This chapter details the changing landscape of training and workforce diversity; describes efforts to sustain the cancer research training pool; and discusses approaches to develop a supportive health care workforce that reflects community diversity.
Science, Technology, Engineering, Mathematics, and Medicine Educational Landscape
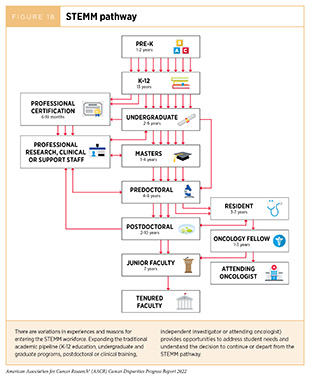
The traditional academic pipeline—starting with K-12 education, through undergraduate and graduate programs, followed by postdoctoral or clinical training, and leading to an independent investigator (including physician-scientist) position—is not linear. For many, there are different pathways that lead them to join the cancer research and care workforce (Figure 18).
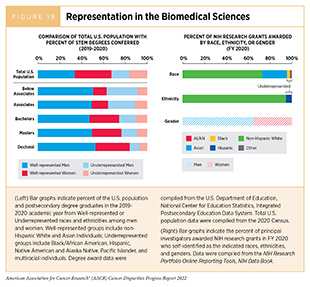
A diverse cancer research and care workforce provides many benefits, including: increased quality of care and patient satisfaction for medically underserved groups (801)Gomez LE, Bernet P. Diversity Improves Performance and Outcomes. Journal of the National Medical Association 2019;111:383-92. [LINK NOT AVAILABLE]; enhanced communication between patients and providers (802)Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, Gender, and Partnership in the Patient-Physician Relationship. JAMA 1999;282:583-9. [LINK NOT AVAILABLE](803)Capers Q, Johnson A, Berlacher K, Douglas P. The Urgent and Ongoing Need for Diversity, Inclusion, and Equity in the Cardiology Workforce in the United States. Journal of the American Heart Association 2021;10. [LINK NOT AVAILABLE]; greater trust and enrollment in clinical trials (522)Niranjan SJ, Martin MY, Fouad MN, Vickers SM, Wenzel JA, Cook ED, et al. Bias and Stereotyping among Research and Clinical Professionals: Perspectives on Minority Recruitment for Oncology Clinical Trials. Cancer 2020;126:1958-68. [LINK NOT AVAILABLE](804)Nazha B, Mishra M, Pentz R, Owonikoko TK. Enrollment of Racial Minorities in Clinical Trials: Old Problem Assumes New Urgency in the Age of Immunotherapy. American Society of Clinical Oncology Educational Book 2019:3-10. [LINK NOT AVAILABLE]; and high-quality jobs for a larger proportion of the population. For example, Black and Hispanic women working with patient navigators who spoke the same language and were from similar racial and ethnic backgrounds received official cancer diagnoses sooner following an abnormal breast or cervical cancer screening (805)Charlot M, Santana MC, Chen CA, Bak S, Heeren TC, Battaglia TA, et al. Impact of Patient and Navigator Race and Language Concordance on Care after Cancer Screening Abnormalities. Cancer 2015;121:1477-83. [LINK NOT AVAILABLE]. However, achieving diversity and promoting fair treatment regardless of identity are persistent challenges across the cancer research and care workforce, especially at senior leadership levels (Figure 19) (806)Valantine HA, Lund PK, Gammie AE. From the NIH: A Systems Approach to Increasing the Diversity of the Biomedical Research Workforce. CBE Life Sci Educ 2016;15:fe4. [LINK NOT AVAILABLE](807)Kamran SC, Winkfield KM, Reede JY, Vapiwala N. Intersectional Analysis of U.S. Medical Faculty Diversity over Four Decades. New England Journal of Medicine 2022;386:1363-71. [LINK NOT AVAILABLE].
Exploring underlying causes for the loss of a significant number of underrepresented minorities (URM: Black, Hispanic, Native American and Alaska Native, Pacific Islander, and multiracial individuals) from the STEMM career pathway and identifying effective strategies to mitigate these factors are essential for creating a more inclusive cancer research workforce (Figure 18). Every step along the STEMM career pathway poses different structural challenges that disproportionately impact trainees. For example, some of the greatest predictors of scientific achievement disparities for Black and Hispanic children in grades three through eight in the United States are (808)Morgan PL, Farkas G, Hillemeier MM, Maczuga S. Science Achievement Gaps Begin Very Early, Persist, and Are Largely Explained by Modifiable Factors. Educational Researcher 2016;45:18-35. [LINK NOT AVAILABLE](809)Betancur L, Votruba-Drzal E, Schunn C. Socioeconomic Gaps in Science Achievement. International Journal of STEM Education 2018;5:38. [LINK NOT AVAILABLE]: gaps in general knowledge in kindergarten and first grade; low socioeconomic status; and attending schools with limited resources. Native Hawaiian or other Pacific Islander children face unique challenges with the STEMM career pathway due to geographical isolation, scarcity of STEMM educators, and a cultural focus on fulfilling the immediate needs of their families and communities (810)Kerr JQ, Hess DJ, Smith CM, Hadfield MG. Recognizing and Reducing Barriers to Science and Math Education and Stem Careers for Native Hawaiians and Pacific Islanders. CBE—Life Sciences Education 2018;17:mr1. [LINK NOT AVAILABLE]. Decades of underinvestment in K-12 education within predominantly racial and ethnic minority communities have contributed to lower graduation rates, lower availability of college-level classes in high school, and lower standardized test scores (811)U.S. Commision on Civil Rights. Public Education Funding Inequity in an Era of Increasing Concentration of Poverty and Resegregation. [updated January 2018, cited 2022 April 22].(812)American University School of Education. Inequality in Public School Funding: Key Issues & Solutions for Closing the Gap. [updated September 10, 2020, cited 2022 April 22].(813)Lafortune J, Rothstein J, Schanzenbach DW. School Finance Reform and the Distribution of Student Achievement. American Economic Journal: Applied Economics 2018;10:1-26. [LINK NOT AVAILABLE]. These factors contribute to fewer URM students enrolling in undergraduate STEMM programs.
Recognizing these challenges and cultivating early childhood interests in STEMM establish a strong educational foundation. This supports the feasibility of becoming a productive and impactful cancer researcher or health care provider in the future. Tailored approaches to increase diversity and promote fair treatment are needed as structural challenges associated with early childhood STEMM education differ between specific groups and settings. These examples highlight the importance of introducing STEMM concepts and training in early childhood and supporting the professional development of K-12 teachers in low-resource areas (814)Institute of Education Sciences – Regional Educational Laboratory Program. Improving High School Graduation Rates for All Evidence Blast. [updated November 14, 2018, cited 2022 April 22]..
A robust ecosystem of flexible, inclusive, and individualized support is needed to foster diversity in STEMM pathways beyond high school. There are disproportionately fewer STEMM bachelor’s degrees earned by racial and ethnic minorities (Figure 19), which can be attributed to educational inequality, reported/perceived discrimination, disenchantment with the original career plan, or changing career plans but remaining in biomedical science (815)Rosenzweig EQ, Hecht CA, Priniski SJ, Canning EA, Asher MW, Tibbetts Y, et al. Inside the Stem Pipeline: Changes in Students’ Biomedical Career Plans across the College Years. Science Advances 2021;7:eabe0985. [LINK NOT AVAILABLE].
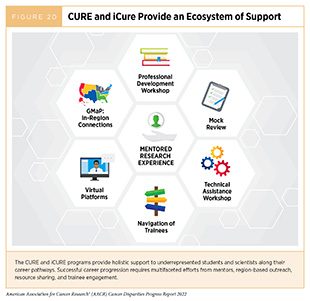
The NCI CRCHD supports URMs from middle school through the junior tenure-track faculty positions with the Continuing Umbrella of Research Experiences (CURE) program (see sidebar on NIH and NCI Initiatives to Promote Workforce Diversity). CURE invests in trainees and scientists from groups typically underrepresented in biomedical research by employing a holistic approach that promotes mentoring, professional support, and career skills building, all surrounding the centerpiece of individually mentored research experience. In addition, the Intramural Continuing Umbrella of Research Experiences (iCURE) brings undergraduate students, postbaccalaureate and post-masters degree individuals, graduate students, and postdoctoral fellows into the NCI research community and supports mentored research experiences. iCURE particularly encourages the participation of individuals from underrepresented populations and aims to further NCI’s interest in diversity (Figure 20).
Additional programs, such as the Science, Education, Partnership Awards (SEPA) Program from NIH’s National Institute of General Medical Sciences, facilitate collaborations between K-12 teachers and medical researchers to provide early opportunities to engage with medical research (816)National Institutes of Health. Science Education Partnership Award. [updated April 22, 2022, cited 2022 April 22].. A SEPA program at the University of Arizona, Q-Cubed, included 787 high school students from a historically underserved community and 98 percent of the participants went on to attend college between 1987-2021. In comparison, approximately half of high school graduates in Arizona went on to attend college in 2018 (817)The National Center for Higher Education Management Systems. College-Going Rates of High School. [updated cited 2022 April 22].. Expanding upon these excellent initiatives carries the potential to improve equity in early-life educational opportunities. However, additional large structural changes are necessary to fully develop the potential of children from historically marginalized communities.
Diversity in the Basic and Translational Cancer Research Workforce
Building a diverse workforce requires understanding and addressing the underlying structural challenges that continue to perpetuate inequity in STEMM training and career progression. PhD students and postdoctoral fellows are the foundation of the cancer research workforce, as they conduct the vast majority of basic and translational experiments. Recruiting diverse graduate school applicants from Minority-Serving Institutions has the potential to promote a diverse graduate student body (818)The Graduate School at Duke University. Director of Uncf/Mellon Program Shares Insights on Recruiting from Hbcus. [updated November 27, 2018, cited 2022 April 22].. Retaining URM scientists is also critical. Studies show that URM graduate students and scientists receive less mentoring support than well-represented peers (819)Carpten JD, Fashoyin-Aje L, Garraway LA, Winn R. Making Cancer Research More Inclusive. Nature Reviews Cancer 2021;21:613-8. [LINK NOT AVAILABLE](820)National Academies of Sciences EM, Affairs PG, Workforce BHE, STEMM CEM, Dahlberg ML, Byars-Winston A. The Science of Effective Mentorship in STEMM. National Academies Press; 2020. [LINK NOT AVAILABLE]. While academia primarily incentivizes scientists who propose innovative grants and succeed in publishing scientific articles, many successful senior scientists may benefit from additional training in mentorship which would subsequently help support the professional development of their trainees. In fact, incentives and compensation for excellence in mentorship as well as formal training programs have been shown to increase retention of URM scientists (820)National Academies of Sciences EM, Affairs PG, Workforce BHE, STEMM CEM, Dahlberg ML, Byars-Winston A. The Science of Effective Mentorship in STEMM. National Academies Press; 2020. [LINK NOT AVAILABLE]. Providing additional institutional supports, such as mental health and childcare services, can also improve retention of graduate students and postdoctoral fellows in academia (821)National Academies of Sciences E, and Medicine. Mental Health, Substance Use, and Wellbeing in Higher Education: Supporting the Whole Student. Washington, DC: The National Academies Press; 2021. [LINK NOT AVAILABLE](822)Turning Chutes into Ladders for Women Faculty: A Review and Roadmap for Equity in Academia. Journal of Women’s Health 2020;29:721-33. [LINK NOT AVAILABLE]. Less than 15 percent of life science PhD graduates receive a tenure-track research position within five years of graduation (821)National Academies of Sciences E, and Medicine. Mental Health, Substance Use, and Wellbeing in Higher Education: Supporting the Whole Student. Washington, DC: The National Academies Press; 2021. [LINK NOT AVAILABLE], which emphasizes the need to reform graduate education to support and prepare students for a variety of fulfilling career options. The challenge of finding a tenure-track position has been made even more difficult by the COVID-19 pandemic forcing many universities to freeze hiring new faculty members (7)American Association for Cancer Research. Aacr Report on the Impact of COVID-19 on Cancer Research and Patient Care. [updated February 10, 2022, cited 2022 April 22].. While these general issues affect all scientists, URM scientists navigate structural racism (see Collaborative Resources to Build Health Equity Partnerships), have a greater likelihood of being first-generation college students, and infrequently receive financial support from family members during tenuous career transitions. These hurdles exacerbate difficulties inherent within the academic job market.
A key milestone that establishes a scientist as an independent investigator is attaining an NIH Research Project (R01) grant. It is concerning that the challenges described in this chapter hinder DEIA efforts and independence across STEMM pathways (see Science, Technology, Engineering, Mathematics, and Medicine Educational Landscape). Early-stage women and/or URM researchers received a disproportionately low number of R01 grants in fiscal year (FY) 2020 when compared to male scientists from well-represented groups (823)National Institutes of Health – NIH Data Book. NIH Data Book – Data by Gender. [updated February 2022, cited 2022 April 22].. A key contributing factor is that start-up packages—money and resources provided by institutes to new faculty for starting their own laboratories—offered to women scientists are on average 60 percent less than those offered to men (824)Sege R, Nykiel-Bub L, Selk S. Sex Differences in Institutional Support for Junior Biomedical Researchers. JAMA 2015;314:1175-7. [LINK NOT AVAILABLE]. Furthermore, disproportionate dependent-care responsibilities, greater time spent mentoring trainees, and lower pay contribute to female scientists leaving academic research positions more frequently than men (825)Northeastern University. Do Women Publish Less Than Men in Scientific Fields? Turns out, Scientists Have Been Asking the Wrong Question. [updated March 5, 2020, cited 2022 April 22].826). These issues highlight the need for focused efforts and funding mechanisms to support women and URM scientists in order to increase diversity in the workforce (826a)Odedina FT, Stern MC. Role of funders in addressing the continued lack of diversity in science and medicine. Nat Med. 2021;27:1859-1861. [LINK NOT AVAILABLE].
NIH and NCI have recently created several initiatives to support URM scientists in the research workforce (see sidebar on NIH and NCI Initiatives to Promote Workforce Diversity). As one example, the UNITE initiative was established with the goal of ending structural racism across NIH and the NIH-supported scientific community. To improve equity, there needs to be continued focus on retaining every promising scientist, addressing bias in the grant review process, offering flexibility in career status and grant timelines, fostering innovation in recruitment strategies, and using formalized mentor training programs to improve mentorship skills and interaction with mentees (806)Valantine HA, Lund PK, Gammie AE. From the NIH: A Systems Approach to Increasing the Diversity of the Biomedical Research Workforce. CBE Life Sci Educ 2016;15:fe4. [LINK NOT AVAILABLE](827).
NCI and NIH have created several funding mechanisms to directly support URM ESIs. For example, the K01, K99/R00, and R21 grant mechanisms support postdoctoral early-career scientists in gaining their independence. Some K01 and R21 grants in particular are focused on supporting URM scientists (828)National Cancer Institute. NCI Mentored Research Scientist Development Award to Promote Diversity (K01). [updated April 22, 2022, cited 2022 April 22].(829)National Cancer Institute. Exploratory Grant Award to Promote Workforce Diversity in Basic Cancer Research (R21). [updated June 14, 2021, cited 2022 April 22].. This year, NIH also announced new administrative supplements for mentors committed to training URM scientists (830)National Institutes of Health – Office of Extramural Research. New Nih Administrative Supplements Available to Support Diversity Mentorship. [updated February 9, 2022, cited 2022 April 22].. Starting in 2022, scientists with current NIH-funded grants supporting mentorship and training activities can apply for up to $250,000 in direct cost support to fund research projects and career development for trainees. In addition, NIH institutes and centers issued 171 student loan repayment awards in FY 2020 totaling almost $13 million for investigators involved in health disparities research (831)National Institutes of Health – Office of Extramural Research. What’s New with the NIH Loan Repayment Programs: FY 2022 Applications, Anniversaries, and a New Program. [updated April 22, 2022, cited 2022 April 22].. Focused approaches to fund ESIs and women researchers from underrepresented groups should be a priority, as this could improve recruitment and retention within the cancer research workforce (see sidebar on NIH and NCI Initiatives to Promote Workforce Diversity). Robust, sustained, and predictable funding increases for NIH and NCI are critical to ensure that these programs continue.
Diversity in the Cancer Care Workforce
Physicians
Similar to the cancer research workforce, diversity in the cancer care workforce does not reflect the patient population, especially at higher career stages (Figure 21). Failure to retain diverse physicians in the training pathway contributes to staffing shortages. It is estimated that the United States will have 2,250 fewer oncologist physicians in 2025 than needed to maintain the same ratio of providers to patients as there was during 2014 (832)Yang W, Williams JH, Hogan PF, Bruinooge SS, Rodriguez GI, Kosty MP, et al. Projected Supply of and Demand for Oncologists and Radiation Oncologists through 2025: An Aging, Better-Insured Population Will Result in Shortage. Journal of Oncology Practice 2014;10:39-45. [LINK NOT AVAILABLE]. Approximately 21 percent of 13,146 U.S. oncologists were over the age of 64 years in 2021 (833)ASCO. 2021 Snapshot: State of the Oncology Workforce in America. JCO Oncology Practice 2021;17:249. [LINK NOT AVAILABLE], suggesting a significant proportion may soon retire. It is concerning that only 577 new oncologists graduated U.S. oncology fellowship programs in 2021 (833)ASCO. 2021 Snapshot: State of the Oncology Workforce in America. JCO Oncology Practice 2021;17:249. [LINK NOT AVAILABLE]. This shortage of oncologists has an immediate impact on the ability to access and deliver cancer care in underserved communities, particularly in rural areas; 32 million Americans live in rural counties that do not have any oncologists, which is an important missing aspect of geographical diversity in the workforce (834)2020 Snapshot: State of the Oncology Workforce in America. JCO Oncology Practice 2021;17:30. [LINK NOT AVAILABLE]. These shortages lead to long working hours and high burnout rates (835)Shanafelt TD, Gradishar WJ, Kosty M, Satele D, Chew H, Horn L, et al. Burnout and Career Satisfaction among US Oncologists. J Clin Oncol 2014;32:678-86. [LINK NOT AVAILABLE], which impact access to care as well as quality of care. One of the most significant predictors of where physicians will start their careers is where they train; almost half of physicians continue to practice in the state where they conducted a residency, and more than two thirds of physicians continue to practice in the state if they attended medical school and conducted a residency in that state (836)Association of American Medical Colleges. 2021 – State Physician Worforce Data Report. [updated January 2022, cited 2022 April 22].. Therefore, providing increased residency and fellowship positions in rural areas is critical to grow the rural workforce, as well as establishing new medical schools in historically underserved areas. It is notable that Alaska, Montana, and Wyoming do not have medical schools to train physicians. Enhancing federal student loan repayment programs or other financial incentives for physicians to work in rural areas or urban communities that are medically underserved could also improve access to health care by building the local workforce (837)Bärnighausen T, Bloom DE. Financial Incentives for Return of Service in Underserved Areas: A Systematic Review. BMC Health Services Research 2009;9:86. [LINK NOT AVAILABLE].
It is encouraging that the matriculating class of medical students in 2021 was the largest and most diverse ever (839)Association of American Medical Colleges. 2021 Fall Applicant, Matriculant, and Enrollment Data Tables. [updated December 2021, cited 2022 April 22]., with Black first-year medical students comprising 11.3 percent, Hispanic students comprising 12.7 percent, and Asian students comprising 26.5 percent of the matriculating class. Additionally, women comprised 55.5 percent of the matriculating class. The increase of first year medical students from diverse populations aligns with the lifelong efforts of LaSalle D. Leffall, Jr., MD. Mentoring and training future physicians from diverse backgrounds is key to addressing cancer health inequities. However, a critical bottleneck in training more physicians is the congressionally mandated limit on the number of Medicare-funded medical residency positions following medical school (840)Congressional Research Service. Federal Support for Graduate Medical Education: An Overview. [updated April 22, 2022, cited 2022 April 22].(841)Association of American Medical Colleges. State-by-State Graduate Medical Education Data. [updated April 22, 2022, cited 2022 April 22].. While some states and universities fund a few medical residencies, Medicare funds the vast majority. This means that thousands of highly capable medical school graduates may not be able to ultimately practice medicine and must find nonclinical jobs (842)HCP Live. Options for Physicians Who Don’t Get Accepted to Residency Programs. [updated December 7, 2016, cited 2022 April 22].(843)The New York Times. ‘I Am Worth It’: Why Thousands of Doctors in America Can’t Get a Job. [updated July 20, 2021, cited 2022 April 22].. As part of the FY 2021 federal appropriations package, Congress provided funds for 200 additional residency spots per year for five years, with a focus on areas with physician shortages (844)Centers for Medicare & Medicaid Services. CMS Funding 1,000 New Residency Slots for Hospitals Serving Rural & Underserved Communities. [updated December 17, 2021, cited 2022 April 22].; this was the largest increase to Medicare-funded residency spots in 25 years. Further lifting the cap on Medicare-funded residencies would enable the training of additional oncologists and other physicians, including URM physicians. In addition, continued efforts from all stakeholders are needed to ensure a diverse and representative oncology residency workforce, considering recent evidence of continued disparities in URM representation within oncology training programs (798)Lang JJ, Issa R, Lombardi C, Garcia E, Oke OC, Ekwenna O. Trends in Race and Ethnicity among Matriculants to US Oncology Training Programs, 2015-2020. JAMA Netw Open 2021;4:e2128530-e. [LINK NOT AVAILABLE].
Efforts from professional societies are also important for diversifying the health care workforce. The National Medical Association provides scholarships for African American students to attend medical school (845)National Medical Association. About Us – National Medical Association. [updated April 22, 2022, cited 2022 April 22].. In 2021, the American Medical Association (AMA) unveiled a new strategic plan to build equity and reconcile the organization’s own history with policies that exacerbated structural racism throughout health care (846)American Medical Association. Ama Adopts New Policy to Increase Diversity in Physician Workforce. [updated June 17, 2021, cited 2022 April 22].. AMA’s plan includes working with medical schools to develop more inclusive recruitment policies and advocating for funds to create new medical schools at Historically Black Colleges and Universities (HBCUs), Hispanic-Serving Institutions, and Tribal Colleges and Universities.
Physician-Scientists
Physician-scientists fill a unique niche in cancer research and care due to their dual training in both science and medicine. However, this valuable skill set means that physician-scientists have great demands on their time and may not have adequate room in their schedules to conduct research to develop successful grant proposals. Due to similar issues facing women in basic cancer research described earlier, women physician-scientists are 30 percent less likely than male physician-scientists to receive an R01-equivalent grant within eight years of joining a postdoctoral program. Furthermore, URM physician-scientists are 17 percent less likely than NHW or Asian physician-scientists to receive an R01-equivalent grant (848)National Institutes of Health – Office of Extramural Research. Further Demographic Analyses of NIH R01 Grant Outcomes of T32 Postdoctoral Participants – NIH Extramural Nexus. [updated July 27, 2021, cited 2022 April 22].. Receiving an NIH K award, such as a K08 or K23, to protect research time in the clinical postdoctoral setting was associated with a 10-fold greater likelihood of receiving an R01-equivalent grant. Therefore, K awards or other support to protect research time focused on female and other underrepresented physician-scientists could greatly help improve the diversity of physician-scientists. More recently, AACR collaborated with the Bristol Myers Squibb Foundation and National Medical Fellowships on an initiative to train 250 community-oriented clinical trial investigators who are underrepresented in medicine or have demonstrated a commitment to increasing diversity in clinical trials; named Robert A. Winn Diversity in Clinical Trials Award Program, this new initiative is a testament to our commitment to eliminating cancer health disparities by propelling tangible improvements in cancer workforce diversity (849)American Association for Cancer Research. AACR to Partner with the Bristol Myers Squibb Foundation on Its Diversity in Clinical Trials Career Development Program. [updated May 19, 2021, cited 2022 April 22].(850)Bristol Myers Squibb. Bristol Myers Squibb Foundation Honors Diversity and Health Equity Leader by Naming Diversity in Clinical Trials Training Program after Him; Welcomes Gilead Sciences as Program Supporter. [updated April 11, 2022, cited 2022 April 22]. Increasing the diversity of physician-scientists is crucial to build trust in medical research and stimulate innovation.
Other Health Care Professionals
Comprehensive cancer care teams are consist of additional professionals, such as physician assistants, nurse practitioners, registered nurses, dieticians, community health workers, patient navigators, and other care partners, who play an important role in cancer care; yet many of these professions do not reflect the patient populations they serve. For example, in 2020, 7.2 percent of U.S. registered nurses identified as Asian, 6.7 percent identified as Black, 5.6 percent as Hispanic, and 0.5 percent as AI/AN (851)Smiley RA, Ruttinger C, Oliveira CM, Hudson LR, Allgeyer R, Reneau KA, et al. The 2020 National Nursing Workforce Survey. Journal of Nursing Regulation 2021;12:S1-S96. [LINK NOT AVAILABLE]. A 2018 analysis estimated that the United States would have a shortage of 154,018 registered nurses by 2020 and 510,394 by 2030 (852)Zhang X, Tai D, Pforsich H, Lin VW. United States Registered Nurse Workforce Report Card and Shortage Forecast: A Revisit. Am J Med Qual 2018;33:229-36. [LINK NOT AVAILABLE]. The COVID-19 pandemic has made this shortage dramatically apparent and has further exacerbated it (853)Yang Y, Mason D. COVID-19’s Impact on Nursing Shortages, the Rise of Travel Nurses, and Price Gouging. [updated January 28, 2022, cited 2022 April 22].(854)Yong E. Why Health-Care Workers Are Quitting in Droves. [updated November 16, 2021, cited 2022 April 22].. A key bottleneck in training additional registered nurses is the lack of nurse instructors and the related capacity of undergraduate programs (855)American Association of Colleges of Nurses. Nursing Shortage. [updated September 2020, cited 2022 April 22].. Supporting larger nursing programs, especially at Minority-Serving Institutions, could significantly increase the diversity of registered nurses. As discussed in the following chapter (see Policies to Address Disparities in Clinical Research and Care), community health workers and patient navigators help connect racial and ethnic minority patients with the health care system and other resources that build health equity and reduce health care costs by promoting disease prevention (856)Mailloux CG, Halesey E. Patient Navigators as Essential Members of the Healthcare Team: A Review of the Literature. 2018. [LINK NOT AVAILABLE](857)Charlot M, Stein JN, Damone E, Wood I, Forster M, Baker S, et al. Effect of an Antiracism Intervention on Racial Disparities in Time to Lung Cancer Surgery. J Clin Oncol. 2022; 40:1755-1762. [LINK NOT AVAILABLE](858)Shreya Kangovi NM, David Grande, Judith A. Long, and David A. Asch. Evidence-Based Community Health Worker Program Addresses Unmet Social Needs and Generates Positive Return on Investment. Health Affairs 2020;39:207-13. [LINK NOT AVAILABLE](859)Corbett CM, Somers TJ, Nuñez CM, Majestic CM, Shelby RA, Worthy VC, et al. Evolution of a Longitudinal, Multidisciplinary, and Scalable Patient Navigation Matrix Model. Cancer Medicine 2020;9:3202-10. [LINK NOT AVAILABLE]. Community health workers are more likely than other types of health workers to reflect the demographic makeup of the patients they serve (860)Zippia. Community Health Worker Demographics and Statistics in the US. [updated April 18, 2022, cited 2022 April 22]., partly due to less expensive education requirements that lower barriers to entering the profession. Community health workers also provide net health care cost savings by reducing the amount of emergency care their patients require (858)Shreya Kangovi NM, David Grande, Judith A. Long, and David A. Asch. Evidence-Based Community Health Worker Program Addresses Unmet Social Needs and Generates Positive Return on Investment. Health Affairs 2020;39:207-13. [LINK NOT AVAILABLE]. However, funding sources for community health workers and patient navigators are often not sustainable. Facilitating and incentivizing the training of more health care providers from medically underserved communities would not only benefit patients in those communities, but also provide stable, high-quality jobs for local economies that are historically disadvantaged.