Disparities in Cancer Screening for Early Detection
In this section, you will learn:
- Cancer screening aims to find precancerous lesions and cancers at their earliest stage when it is easier to treat them.
- Population-based screenings are performed based on age and sex for those at an average risk of developing cancer, and based on behavioral factors or family history for those at a higher risk of developing cancer.
- Professional organizations and government-affiliated agencies carefully evaluate the benefits and harms of cancer screening to make evidence-based recommendations for its use in the clinic.
- Adherence to routine cancer screening reduces mortality from the cancer for which individuals are screened.
- Socioeconomic and structural barriers are primary contributors to cancer screening disparities for racial and ethnic minorities and other medically underserved populations.
- Stakeholders across the cancer control continuum are developing and implementing multipronged strategies that are culturally and linguistically tailored to raise cancer screening awareness, access, and adherence among the underscreened populations.
- Research regarding genetics of ancestry and its impact on cancer risk may improve the precision of personalized screening for patients in the future.
Cancer screening is defined as looking for precancerous lesions, or early cancers before a person develops any signs or symptoms. While modifying certain behaviors can reduce the risk of developing cancer, routine screening for cancer can help find an aberration at the earliest possible time during cancer development. Health care providers use the information gleaned from a cancer screening test to make an informed decision on whether to monitor or treat, or surgically remove precancerous lesions or early-stage cancer before either progresses to a more advanced stage (Figure 12).
Ways to Screen for Cancer
There are different kinds of cancer screening tests and exams that include visual examination to check for unusual features such as lumps or discolored skin; medical and family history analyses to review an individual’s genetic, behavioral, and environmental risks; laboratory tests to determine the changes in cancer biomarkers in samples of tissues or fluids in the body; and imaging procedures to look for abnormalities inside the body (see sidebar on Tests for Cancer Screening).
Cancer screening has the potential to save lives by detecting cancer early when it is easier to treat and when chances of
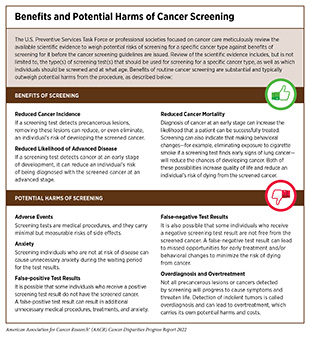
survival are the highest. For example, researchers evaluating the benefits of lung cancer screening recently reported a 25 percent decline in lung cancer deaths at a 10-year follow-up of more than 6,000 participants who underwent lung cancer screening from December 2003 to July 2006 (444)de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced Lung-Cancer Mortality with Volume Ct Screening in a Randomized Trial. New England Journal of Medicine 2020;382:503-13. [LINK NOT AVAILABLE]. Another recent study found that the routine screening for breast cancer in eligible women reduced the risk of dying from breast cancer within 10 years after the initial diagnosis by 41 percent and decreased the risk of developing advanced breast cancer by 25 percent (445)Duffy SW, Tabár L, Yen AM-F, Dean PB, Smith RA, Jonsson H, et al. Mammography Screening Reduces Rates of Advanced and Fatal Breast Cancers: Results in 549,091 Women. Cancer 2020;126:2971-9. [LINK NOT AVAILABLE]. However, it is important to note that some screening tests are invasive medical procedures that can potentially cause harm (see sidebar on Benefits and Potential Harms of Cancer Screening). Because of the potential harms, the risks and benefits of cancer screening are carefully considered for everyone.
Cancer Screening Guidelines
Guidelines for cancer screening are meticulously developed by professional societies focused on public health. The key objective is to help individuals decide whether they should be screened for cancer, at what age they should start screening, how frequently they should get screened, and by which method. In the United States, an independent group of experts convened by the Agency for Healthcare Research and Quality of U.S. HHS carefully evaluates data regarding the benefits and potential harms of different approaches to disease prevention, including cancer screening tests, genetic testing, and preventive therapeutics, to make evidence-based recommendations about the use of these in the clinic. These volunteer experts form USPSTF (Figure 13).
USPSTF recommendations for cancer screening tests fall into four categories, including recommendations for screening certain individuals at certain intervals (see sidebar on Characteristics that Determine Eligibility for Cancer Screening), recommendations against screening, and deciding that there is insufficient evidence to make a recommendation.
In addition to considering evidence regarding potential new screening programs, USPSTF reevaluates existing
recommendations as new research becomes available and can revise the recommendations if necessary (Figure 13). Occasionally, other professional societies focused on cancer care also issue screening guidelines.
Disparities in Cancer Screening
Early detection of cancer through routine screening saves lives by catching the disease early; minimizing risk of cancer progressing to an advanced, harder-to-treat stage; and thus improving both the survival and quality of life. According to one recent estimate, increasing the use of screening for breast, cervical, and colorectal cancers to 100 percent from its levels in 2016 would prevent an additional 2,821, 6,834, and 35,530 deaths, respectively (446)Sharma KP, Grosse SD, Maciosek MV, Joseph D, Roy K, Richardson LC, et al. Preventing Breast, Cervical, and Colorectal Cancer Deaths: Assessing the Impact of Increased Screening. Prev Chronic Dis 2020;17:E123. [LINK NOT AVAILABLE]. Unfortunately, not all segments of the U.S. population equitably benefit from routine cancer screening (see sidebar on Guidelines for and Disparities in Screening for Five Cancer Types).
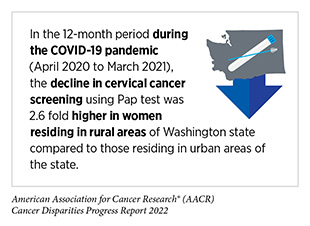
Research shows that cancer screening rates are substantially lower among those from racial/ethnic minorities compared to White individuals (447)Liu D, Schuchard H, Burston B, Yamashita T, Albert S. Interventions to Reduce Healthcare Disparities in Cancer Screening among Minority Adults: A Systematic Review. J Racial Ethn Health Disparities 2021;8:107-26. [LINK NOT AVAILABLE]. Furthermore, screening patterns vary for different types of cancer and/or screening tests among racial and ethnic minorities and other medically underserved populations (4)Kaiser Family Foundation. Racial Disparities in Cancer Outcomes, Screening, and Treatment. [updated February 3, 2022, cited 2022 April 22].. Barriers such as access to health insurance, low health literacy, and miscommunication between patients and providers contribute to low screening rates among minority adults (447)Liu D, Schuchard H, Burston B, Yamashita T, Albert S. Interventions to Reduce Healthcare Disparities in Cancer Screening among Minority Adults: A Systematic Review. J Racial Ethn Health Disparities 2021;8:107-26. [LINK NOT AVAILABLE]. As detailed in the AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care released in February 2022, severe interruptions in routine cancer screening, especially during the initial months of the pandemic, may have exacerbated the existing disparities (7)American Association for Cancer Research. Aacr Report on the Impact of COVID-19 on Cancer Research and Patient Care. [updated February 10, 2022, cited 2022 April 22].. Here, we focus our discussion on the disparities in screening for five cancer types for which USPSTF currently has population-based screening guidelines and discuss some of the interventions that have helped close the disparity gap in cancer screening.
Breast Cancer
The overall screening rates for breast cancer are mostly similar between White women and women from racial and ethnic minorities (451)Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in Meeting USPSTF Breast, Cervical, and Colorectal Cancer Screening Guidelines among Women in the United States. Prev Chronic Dis 2021;18:E37. [LINK NOT AVAILABLE]. However, there are substantial variations in different aspects within the cancer screening process—such as provider–patient communication on the benefits and potential harms of screening; referral for a screening exam; follow-up if the results of a screening exam are positive, among others—that lead to persistent disparities. For example, even though the overall screening rates among Black women are similar to those for White women, researchers have found that Black women receive suboptimal methods of screening for breast cancer. One study evaluated imaging data from nearly 400,000 women who received breast cancer screening between 2015 and 2019 and found that, compared to 60.5 percent of White women, only 44 percent of Black women were screened by digital breast tomosynthesis, considered to be technologically superior in identifying invasive breast cancer (452)Alsheik N, Blount L, Qiong Q, Talley M, Pohlman S, Troeger K, et al. Outcomes by Race in Breast Cancer Screening with Digital Breast Tomosynthesis Versus Digital Mammography. J Am Coll Radiol 2021;18:906-18. [LINK NOT AVAILABLE]. Studies have also found that, compared to NHW women, Black women are 31 percent more likely to have extremely dense breasts (453)Moore JX, Han Y, Appleton C, Colditz G, Toriola AT. Determinants of Mammographic Breast Density by Race among a Large Screening Population. JNCI Cancer Spectrum 2020;4. [LINK NOT AVAILABLE]—a known risk factor for breast cancer. Yet, Black women with dense breasts are less likely to receive supplemental breast imaging to confirm the results of the initial screening test compared to NHW women (15 percent versus 45 percent, respectively) (454)Ezratty C, Vang S, Brown J, Margolies LR, Jandorf L, Lin JJ. Racial/Ethnic Differences in Supplemental Imaging for Breast Cancer Screening in Women with Dense Breasts. Breast Cancer Res Treat 2020;182:181-5. [LINK NOT AVAILABLE]. Since Black women face higher risks of breast cancer at younger ages compared to White women, and higher risk of biologically aggressive breast tumors at all ages (see Black or African American Population), many disparities researchers advocate in favor of screening mammography beginning at age 40 years as a strategy to mitigate breast cancer disparities.
Similar variations in aspects of breast cancer screening are also prevalent among women from other ethnic and racial minorities. One study found that Hispanic women were 12 times less likely to be screened for breast cancer more than once in a 5-year period compared to White women (452)Alsheik N, Blount L, Qiong Q, Talley M, Pohlman S, Troeger K, et al. Outcomes by Race in Breast Cancer Screening with Digital Breast Tomosynthesis Versus Digital Mammography. J Am Coll Radiol 2021;18:906-18. [LINK NOT AVAILABLE]. There are also significant differences in breast cancer screening rates within minority populations who represent a diverse group of individuals with unique cultural identities and behavioral habits. For instance, within the Asian American population, women who immigrated from Korea had the lowest screening rates (55 percent), while those from China had the highest rate (72 percent) (455)Li Y, Xie H, Theodoropoulos N, Wang Q. Mammography Screening Disparities in Asian American Women: Findings from the California Health Interview Survey 2015-2016. J Clin Oncol 2021;39:e18568. [LINK NOT AVAILABLE].
Research has shown that the largest disparities in receiving the recommended screening for breast cancer are determined by socioeconomic status (SES), level of education, and access to health care, all of which also intersect with racial and ethnic identities to exacerbate breast cancer screening disparities (see Factors That Drive Cancer Health Disparities. For example, the rate of breast cancer screening was 10 percentage points less among women with a high school diploma compared to those with a college degree (451)Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in Meeting USPSTF Breast, Cervical, and Colorectal Cancer Screening Guidelines among Women in the United States. Prev Chronic Dis 2021;18:E37. [LINK NOT AVAILABLE]. Access to health insurance was the biggest determinant of disparity in meeting the USPSTF guidelines for breast cancer screening. In 2018, there was a difference of 26 percentage points in breast cancer screening between women who had some form of health insurance (80.5 percent) versus those without any health insurance (54.5 percent) (451)Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in Meeting USPSTF Breast, Cervical, and Colorectal Cancer Screening Guidelines among Women in the United States. Prev Chronic Dis 2021;18:E37. [LINK NOT AVAILABLE].
Successful breast cancer screening relies on timely follow up if the exam shows any abnormalities. Delaying or failing to follow up on a screening exam undermines the potential benefits of screening and is associated with poorer outcomes. Researchers are finding that women from racial and ethnic minorities and other medically underserved populations often do not receive follow up care (456)Reece JC, Neal EFG, Nguyen P, McIntosh JG, Emery JD. Delayed or Failure to Follow-up Abnormal Breast Cancer Screening Mammograms in Primary Care: A Systematic Review. BMC Cancer 2021;21:373. [LINK NOT AVAILABLE]. The reasons for failure to follow-up include lack of access to health insurance, fear of cost, lack of health literacy, and/or miscommunications between patient and provider.
Disparities in routine breast cancer screening are also apparent for transgender individuals, who are at an increased risk of developing breast cancer. A recent study showed that, compared to individuals whose gender identity aligns with the one associated with the sex assigned to them at birth (cisgender), only 32 percent of individuals transitioning from female to male and just two percent of those transitioning from male to female had undergone breast cancer screening (457)Oladeru OT, Ma SJ, Miccio JA, Wang K, Attwood K, Singh AK, et al. Breast and Cervical Cancer Screening Disparities in Transgender People. Am J Clin Oncol 2022;45:116-21. [LINK NOT AVAILABLE]. In addition to better quality data to develop cancer screening guidelines that are specific to the needs of SGM populations, culturally sensitive interventions are urgently needed to close gaps in provider and patient knowledge about cancer screening and improve health care experiences of gender minorities in the United States (458)Sterling J, Garcia MM. Cancer Screening in the Transgender Population: A Review of Current Guidelines, Best Practices, and a Proposed Care Model. Transl Androl Urol 2020;9:2771-85. [LINK NOT AVAILABLE](459)Nelson B. A Cancer Screening Crisis for Transgender Patients: Discrimination, Patient Unease, Provider Ignorance, and a Highly Gendered Health Care System Are Impeding Cancer Screening and Risk Assessment in the Transgender Population. In This Article, the First of a 2-Part Series, We Explore How Clinicians Can Begin to Address Those Barriers. Cancer Cytopathol 2019;127:421-2. [LINK NOT AVAILABLE].
Cervical Cancer
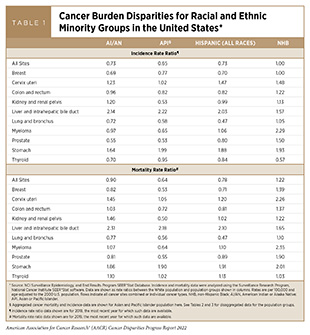
According to the most recent estimates available, the overall cervical cancer screening rate was more than 80 percent in the U.S. in 2018(460)Patterns of Mammography, Pap Smear, and Colorectal Cancer Screening Services among Women Aged 45 and Over. In: National Center for Health S, editor. National Health Statistics Reports, National health statistics reports; no. 157. Hyattsville, MD.. However, there are disparities in screening rates based on sociodemographics. Compared to the White population, incidence of cervical cancer is higher among all racial and ethnic minorities (see Table 1). The disparate rates of cervical cancer incidence are particularly alarming because medically underserved and underscreened populations account for more than 60 percent of cervical cancer diagnoses (461)Scarinci IC, Garcia FAR, Kobetz E, Partridge EE, Brandt HM, Bell MC, et al. Cervical Cancer Prevention. Cancer 2010;116:2531-42. [LINK NOT AVAILABLE].
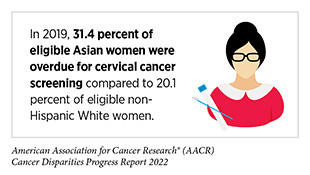
In recent years, the percentage of women in the U.S. who are overdue for cervical cancer screening has been growing (462)Suk R, Hong Y-R, Rajan SS, Xie Z, Zhu Y, Spencer JC. Assessment of US Preventive Services Task Force Guideline–Concordant Cervical Cancer Screening Rates and Reasons for Underscreening by Age, Race and Ethnicity, Sexual Orientation, Rurality, and Insurance, 2005 to 2019. JAMA Netw Open 2022;5:e2143582-e. [LINK NOT AVAILABLE]. It is important to note that this increase predates the COVID-19 pandemic and is independent of the severe interruptions in overall cancer screening during the first half of 2020 (7)American Association for Cancer Research. Aacr Report on the Impact of COVID-19 on Cancer Research and Patient Care. [updated February 10, 2022, cited 2022 April 22]., which may further worsen these trends. Researchers found that the number of women overdue for cervical cancer screening increased overall between 2005 and 2019. For example, the proportion of women ages 21 to 29 years without up-to-date screening doubled from 14.2 percent in 2005 to 29.1 percent by 2019 (462)Suk R, Hong Y-R, Rajan SS, Xie Z, Zhu Y, Spencer JC. Assessment of US Preventive Services Task Force Guideline–Concordant Cervical Cancer Screening Rates and Reasons for Underscreening by Age, Race and Ethnicity, Sexual Orientation, Rurality, and Insurance, 2005 to 2019. JAMA Netw Open 2022;5:e2143582-e. [LINK NOT AVAILABLE]. A significant proportion of Hispanic women (64.4 percent), who have the highest incidence of cervical cancer among racial and ethnic minorities (see Table 1), were overdue for cervical cancer screening; it is alarming that the reason for this disparity was because they did not know they needed to be screened for cervical cancer. Conversely, access to health care was a major source of disparity among NHW women; 10.4 percent indicated lack of access as the reason for not receiving cervical cancer screening compared to only 3.2 percent of Asian women— the population group with the highest proportion of overdue cervical cancer screening (462)Suk R, Hong Y-R, Rajan SS, Xie Z, Zhu Y, Spencer JC. Assessment of US Preventive Services Task Force Guideline–Concordant Cervical Cancer Screening Rates and Reasons for Underscreening by Age, Race and Ethnicity, Sexual Orientation, Rurality, and Insurance, 2005 to 2019. JAMA Netw Open 2022;5:e2143582-e. [LINK NOT AVAILABLE].
Disparities in cervical cancer screening are also persistent in other medically underserved populations. According to a recent study, women who identified as lesbian were 22 percent less likely to be up to date with their cervical cancer screening in 2018 (448)Sabatino SA, Thompson TD, White MC, Shapiro JA, de Moor J, Doria-Rose VP, et al. Cancer Screening Test Receipt – United States, 2018. MMWR Morb Mortal Wkly Rep 2021;70:29-35. [LINK NOT AVAILABLE]. Findings from another recent study highlight the disparities in routine cancer screening for transgender individuals despite their increased risk for cervical cancer. Compared to cisgender individuals, individuals transitioning from female to male were 58 percent less likely to adhere to cervical cancer screening (457)Oladeru OT, Ma SJ, Miccio JA, Wang K, Attwood K, Singh AK, et al. Breast and Cervical Cancer Screening Disparities in Transgender People. Am J Clin Oncol 2022;45:116-21. [LINK NOT AVAILABLE].
Place of residence also plays an important role in staying up to date with cervical cancer screening. In 2018, women living in rural areas were 34 percent less likely to be up to date with cervical cancer screening compared to those living in urban areas. Researchers identified the lack of access to health care as a significant contributor to this disparity (463)Locklar LRB, Do DP. Rural-Urban Differences in HPV Testing for Cervical Cancer Screening. J Rural Health 2022;38:409-15. [LINK NOT AVAILABLE]. Another study found that women without any health insurance in 2018 were 17 percent less likely to have received cervical cancer screening compared to those who had some form of health insurance (451)Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in Meeting USPSTF Breast, Cervical, and Colorectal Cancer Screening Guidelines among Women in the United States. Prev Chronic Dis 2021;18:E37. [LINK NOT AVAILABLE].
Colorectal Cancer
In recent years, the rate of colorectal cancer (CRC) diagnoses in individuals who are younger than 50 years of age—a diagnosis that is considered an early-onset colorectal cancer (EOCRC)— has increased by 2.2 percent every year (465)American Cancer Society. Colorectal Cancer Facts & Figures 2020-2022. [LINK NOT AVAILABLE], prompting USPSTF in 2021 to lower the recommended age for initiating CRC screening from 50 to 45 years (466)Force UPST. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 2021;325:1965-77. [LINK NOT AVAILABLE]. According to a recent report, the alarming increase in EOCRC is disproportionately high in Black and Hispanic individuals compared to White individuals (12.7 percent versus 16.5 percent versus 8.7 percent) (467)Acuna-Villaorduna AR, Lin J, Kim M, Goel S. Racial/Ethnic Disparities in Early-Onset Colorectal Cancer: Implications for a Racial/Ethnic-Specific Screening Strategy. Cancer Medicine 2021;10:2080-7. [LINK NOT AVAILABLE]. The reasons for EOCRC are not clear.
There has been some progress toward reducing disparities in colorectal screening in recent years. Researchers have observed that the proportion of individuals who were not up to date with CRC screening decreased for most racial and ethnic minorities between 2012 and 2020; compared to White individuals, the decrease was the largest for NHOPI (from 46 percent in 2012 to 28 percent in 2020), followed by Hispanic people (from 47 percent in 2012 to 37 percent in 2020) (4)Kaiser Family Foundation. Racial Disparities in Cancer Outcomes, Screening, and Treatment. [updated February 3, 2022, cited 2022 April 22].. Despite the narrowing disparity in staying up to date with the CRC screening, Hispanic, Asian, and AI/AN people were still more likely than White people not to be up to date with CRC screening tests in 2020(4)Kaiser Family Foundation. Racial Disparities in Cancer Outcomes, Screening, and Treatment. [updated February 3, 2022, cited 2022 April 22]..
Disparities in CRC screening are complex and multidimensional. For example, a similar proportion of Black and White individuals were up to date with CRC screening in 2018 (65.3 percent versus 67.9 percent, respectively) (448)Sabatino SA, Thompson TD, White MC, Shapiro JA, de Moor J, Doria-Rose VP, et al. Cancer Screening Test Receipt – United States, 2018. MMWR Morb Mortal Wkly Rep 2021;70:29-35. [LINK NOT AVAILABLE]. However, evidence is accruing that population-specific guidelines may be necessary to ensure that individuals at a disproportionately higher risk of developing certain types of cancer receive screening starting at the age and using tests that will increase the chances of diagnosing cancer early when it is easier to treat. As one example, one study found that Black individuals, especially Black females, were more likely to be diagnosed with advanced stage EOCRC, and that the cancer was likely to be present in areas of the colon that are harder to image by sigmoidoscopy (467)Acuna-Villaorduna AR, Lin J, Kim M, Goel S. Racial/Ethnic Disparities in Early-Onset Colorectal Cancer: Implications for a Racial/Ethnic-Specific Screening Strategy. Cancer Medicine 2021;10:2080-7. [LINK NOT AVAILABLE], indicating that specific CRC screening guidelines may be needed for younger Black women.
For Hispanic individuals, there are significant disparities in being up to date with the recommended CRC screening, and these disparities vary by population subgroup. In 2018, for instance, Puerto Rican individuals were more likely to be up to date with the recommended CRC screening compared to non-Hispanic individuals (76.6 percent versus 68.2 percent, respectively). In comparison, Mexican American individuals were significantly less likely to be up to date with CRC screening (52.3 percent) (468)Viramontes O, Bastani R, Yang L, Glenn BA, Herrmann AK, May FP. Colorectal Cancer Screening among Hispanics in the United States: Disparities, Modalities, Predictors, and Regional Variation. Prev Med 2020;138:106146. [LINK NOT AVAILABLE]. Other studies have shown CRC screening disparities among Hispanic populations also vary by state and are primarily determined by the lack of adequate health insurance and lack of access to care (468)Viramontes O, Bastani R, Yang L, Glenn BA, Herrmann AK, May FP. Colorectal Cancer Screening among Hispanics in the United States: Disparities, Modalities, Predictors, and Regional Variation. Prev Med 2020;138:106146. [LINK NOT AVAILABLE].
Researchers have found that rural residence adversely affects adherence to the recommended CRC screening. Findings from a recent study of nearly 3,000 women across 11 U.S. states revealed that those living in rural areas were 19 percent less likely to be up to date with CRC screening compared to women living in urban areas (449)Shete S, Deng Y, Shannon J, Faseru B, Middleton D, Iachan R, et al. Differences in Breast and Colorectal Cancer Screening Adherence among Women Residing in Urban and Rural Communities in the United States. JAMA Netw Open 2021;4:e2128000. [LINK NOT AVAILABLE]. In 2018, the recommended CRC screening was also significantly lagging among individuals with less than a high school education (54.2 percent compared to 73.5 percent among college graduates); among uninsured individuals (30.2 percent compared to 69 percent among those with private insurance); and among immigrants who had been in the U.S. fewer than ten years (32.8 percent compared to 69.2 percent among those born in U.S.) (448)Sabatino SA, Thompson TD, White MC, Shapiro JA, de Moor J, Doria-Rose VP, et al. Cancer Screening Test Receipt – United States, 2018. MMWR Morb Mortal Wkly Rep 2021;70:29-35. [LINK NOT AVAILABLE]. The prevalence of CRC screening also varies substantially among U.S. states and territories.
There are many barriers to the CRC screening adherence among ethnic and racial minorities and other medically underserved populations. Low SES, lack of access to health care, lack of knowledge about CRC screening, and mistrust in the health care system all contribute to low adherence to CRC screening (469)White PM, Itzkowitz SH. Barriers Driving Racial Disparities in Colorectal Cancer Screening in African Americans. Curr Gastroenterol Rep 2020;22:41. [LINK NOT AVAILABLE]. Researchers have found that sociocultural attitudes such as perceptions of masculinity among Black men are additional barriers to meeting CRC screening recommendations (470)Earl V, Beasley D, Ye C, Halpin SN, Gauthreaux N, Escoffery C, et al. Barriers and Facilitators to Colorectal Cancer Screening in African-American Men. Dig Dis Sci 2022;67:463-72. [LINK NOT AVAILABLE].
Lung Cancer
Less than five percent of all eligible individuals were up to date with low-dose computed tomography (LDCT) in 2016-2017 (471)Okereke IC, Nishi S, Zhou J, Goodwin JS. Trends in Lung Cancer Screening in the United States, 2016-2017. J Thorac Dis 2019;11:873-81. [LINK NOT AVAILABLE], even though adhering to screening guidelines reduces lung cancer-related deaths by more than 20 percent, according to the findings of two landmark studies (444)de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced Lung-Cancer Mortality with Volume Ct Screening in a Randomized Trial. New England Journal of Medicine 2020;382:503-13. [LINK NOT AVAILABLE](472)Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med 2011;365:395-409. [LINK NOT AVAILABLE]. In addition to the overall low adherence rates for LDCT, significant disparities exist between White individuals and those belonging to racial and ethnic minorities.
One key example of the disparity is the LDCT eligibility for Black individuals. Research shows that Black people are at a higher risk of lung cancer at a younger age even if they smoke less over time (473)Aldrich MC, Mercaldo SF, Sandler KL, Blot WJ, Grogan EL, Blume JD. Evaluation of USPSTF Lung Cancer Screening Guidelines among African American Adult Smokers. JAMA Oncol 2019;5:1318-24. [LINK NOT AVAILABLE], and yet they were 36 percent less likely to be eligible for LDCT under the previous USPSTF guidelines (474)Narayan AK, Chowdhry DN, Fintelmann FJ, Little BP, Shepard J-AO, Flores EJ. Racial and Ethnic Disparities in Lung Cancer Screening Eligibility. Radiology 2021;301:712-20. [LINK NOT AVAILABLE]. USPSTF lowered the age to begin screening for lung cancer from 55 to 50 years of age in 2021, in part to mitigate disparities in eligibility criteria for LDCT, and greatly expanded the proportion of individuals eligible for LDCT. However, initial findings suggest that additional changes to the guidelines may be necessary to further decrease the gap in LDCT eligibility of Black individuals. One study examined the LDCT eligibility of the participants of the Black Women’s Health Study, which includes nearly 60,000 Black women from across the U.S. Researchers found that the LDCT eligibility of at-risk Black women in the study increased from 22.7 percent under the previous guidelines to 33.9 percent under the revised guidelines, amounting to a 50 percent increase. However, the study also found that removing the restriction from the revised guidelines that former smokers must have stopped smoking within the past 15 years to be eligible for LDCT could have further increased the proportion of eligible Black women from 33.9 percent to 48.2 percent (475)Potter AL, Yang CJ, Woolpert KM, Puttaraju T, Suzuki K, Palmer JR. Evaluating Eligibility of US Black Women under USPSTF Lung Cancer Screening Guidelines. JAMA Oncol 2022;8:163-4. [LINK NOT AVAILABLE]. Additional studies will further help inform evidence-based adaptations to the guidelines ensuring that everyone benefits equally from lifesaving cancer screening recommendations. Racial and ethnic minorities and other medically underserved populations also experience disparities in the follow up visits if the screening results are positive for abnormalities. An analysis of nine studies comprising thousands of individuals who underwent LDCT found that only 67 percent of Black individuals followed up after the initial screening regardless of the stage at which lung cancer was diagnosed (476)Kunitomo Y, Bade B, Gunderson CG, Akgün KM, Brackett A, Cain H, et al. Racial Differences in Adherence to Lung Cancer Screening Follow-Up: A Systematic Review and Meta-Analysis. Chest 2022;161:266-75. [LINK NOT AVAILABLE]. Lack of access to quality health care is also a major contributor to the low LDCT adherence rates (477)Zgodic A, Zahnd WE, Miller DP, Jr., Studts JL, Eberth JM. Predictors of Lung Cancer Screening Utilization in a Population-Based Survey. J Am Coll Radiol 2020;17:1591-601. [LINK NOT AVAILABLE]. One study found that individuals on a fee-for-service Medicare plan—a type of Medicare plan offered by a private insurance company where the plan determines how much the insurer must pay for care—were more than 50 percent less likely to undergo LDCT compared to those with private health insurance (478)Hirsch EA, Barón AE, Risendal B, Studts JL, New ML, Malkoski SP. Determinants Associated with Longitudinal Adherence to Annual Lung Cancer Screening: A Retrospective Analysis of Claims Data. Journal of the American College of Radiology 2021;18:1084-94. [LINK NOT AVAILABLE]. Similarly, place of residence can dictate access to state-of-the-art health care facilities. For example, individuals residing in urban areas were more than twice as likely to undergo LDCT compared to those living in rural areas (478)Hirsch EA, Barón AE, Risendal B, Studts JL, New ML, Malkoski SP. Determinants Associated with Longitudinal Adherence to Annual Lung Cancer Screening: A Retrospective Analysis of Claims Data. Journal of the American College of Radiology 2021;18:1084-94. [LINK NOT AVAILABLE].
Researchers have found that many additional reasons contribute to disparities in LDCT. For patients, reasons include unawareness of screening programs; fear of cancer diagnosis and perceived stigma; and cost concerns. For health care providers, reasons include unfamiliarity with eligibility criteria and insurance coverage; difficulty identifying eligible patients; insufficient time or knowledge to conduct shared decision-making; need for guidance with management of lung cancer screening results; and skepticism about the benefits of screening (479)Wang GX, Baggett TP, Pandharipande PV, Park ER, Percac-Lima S, Shepard J-AO, et al. Barriers to Lung Cancer Screening Engagement from the Patient and Provider Perspective. Radiology 2019;290:278-87. [LINK NOT AVAILABLE].
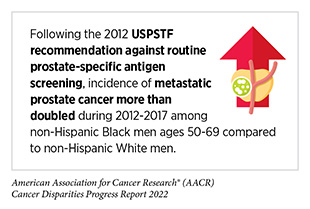
Prostate Cancer
Current USPSTF screening guidelines for prostate cancer recommend that men at an average risk of developing prostate cancer should start discussing potential benefits and harms of prostate cancer screening with their health care providers at the age of 55 (75)U.S. Preventive Services Task Force. Screening for Prostate Cancer: U.S. Preventive Services Task Force Recommendation Statement. JAMA 2018;319:1901-13. [LINK NOT AVAILABLE]. Black men share a disproportionate burden of prostate cancer compared to any other racial or ethnic group in the U.S. (see Cancer Health Disparities Among Racial and Ethnic Minority Populations. There is also a consensus that Black men were poorly represented in the screening studies that informed most current guidelines for prostate cancer (480)Oren O, Beach DF. Representation of African-American Patients in Clinical Studies of Prostate Cancer. J Clin Oncol 2016;34:e18057. [LINK NOT AVAILABLE]. Notably, recent findings indicate that screening Black men for prostate cancer at a younger age can decrease the likelihood of diagnosis with metastatic disease by 39 percent, and reduce the probability of dying from prostate cancer by 25 percent (481)Qiao E, Kotha NV, Nalawade V, Qian A, Voora RS, Nelson TJ, et al. Association of Increased Intensity of Prostate-Specific Antigen Screening in Younger African American Men with Improved Prostate Cancer Outcomes. J Clin Oncol 2021;39:5004. [LINK NOT AVAILABLE]. Some cancer-focused organizations now recommend that Black individuals start a dialogue with their physicians at the age of 45 to make an informed and shared decision about screening for prostate cancer(482)American Cancer Society. American Cancer Society Recommendations for Prostate Cancer Early Detection. [updated April 23, 2021, cited 2022 April 22].. Similar disparities in PSA-based prostate cancer screening exist among men who belong to other racial or ethnic populations (483)Abashidze N, Stecher C, Rosenkrantz AB, Duszak R, Jr, Hughes DR. Racial and Ethnic Disparities in the Use of Prostate Magnetic Resonance Imaging Following an Elevated Prostate-Specific Antigen Test. JAMA Netw Open 2021;4:e2132388. [LINK NOT AVAILABLE].
One persistent disparity in prostate cancer screening is the adherence to follow-up if elevated blood levels of PSA are detected, an indication that the individual may have prostate cancer and should undergo additional imaging-based tests for confirmation (see sidebar on Tests for Cancer Screening). A recent study found that, compared to White patients, Black patients with elevated PSA blood levels were 24-35 percent less likely to undergo subsequent prostate imaging. Researchers also noted that the likelihood of Black patients to undergo follow-up exams was less among those with higher levels of PSA and those between ages 65 and 74 years (483)Abashidze N, Stecher C, Rosenkrantz AB, Duszak R, Jr, Hughes DR. Racial and Ethnic Disparities in the Use of Prostate Magnetic Resonance Imaging Following an Elevated Prostate-Specific Antigen Test. JAMA Netw Open 2021;4:e2132388. [LINK NOT AVAILABLE]. Cost of medical care is another significant contributor to disparities. One study found that 11 percent of those who decided not to get screened for prostate cancer with a PSA test did so because of the concern for the cost of the test (485)Soror N, Keruakous A. Socio-Economic Disparities and Accessibility to Age-Appropriate Screening Tools. J Clin Oncol 2021;39:1529. [LINK NOT AVAILABLE].
Researchers have also identified the need for effective communication between patients and physicians to alleviate disparities in prostate cancer screening. For example, 38.6 percent of those who responded to a survey about the PSA test indicated that their doctor had discussed the advantages of a PSA test. The study also found that Asian men, or those without any form of health insurance, were less likely to be told about the benefits and potential harms of a PSA test (486)Bumanlag IM, Nieves-Jimenez HR, Jaoude JA, Ludmir EB, Taniguchi CM. Abstract Po-249: Prostate Screening &Amp; Patient Knowledge on Psa Testing among Males: Analysis of the 2019 Nhis. Cancer Epidemiology, Biomarkers & Prevention 2022;31:PO-249. [LINK NOT AVAILABLE].
Eliminating Disparities in Cancer Screening
Disparities in early detection of cancer lead to increased cancer diagnoses at an advanced stage when cancer is harder to treat and thus substantially contributes to the disproportionate burden of cancer-related deaths in racial and ethnic minorities and other medically underserved populations (see The State of Cancer Health Disparities in 2022. During the early months of the COVID-19 surge in 2020, elective clinical care (including cancer screening) was shut down in order to divert medical resources to COVID care and to comply with shelter-in-place mandates. After lifting of the hiatus, ongoing social distancing policies placed limits on availability of cancer screening appointments. The pandemic-related recession has been disproportionately severe among Black and Hispanic population groups, resulting in these groups experiencing even greater barriers to cancer screening. Lastly, the costs of COVID care disproportionately devastated many safety-net hospitals, leaving these facilities even more financially constrained when attempting to resume cancer screening programs for socioeconomically disadvantaged individuals. For all of these reasons, disparities experts fear that the pandemic may not only cause an increase in advanced-stage cancer diagnoses in all population groups, but it may also exacerbate the existing disparities in cancer screening.
Eliminating inequities in cancer screening requires more than increasing adherence among eligible individuals. All sectors must work in concert to develop and implement multipronged approaches that include dismantling structural racism, discrimination, and other societal inequities that pose significant barriers in access to cancer screening; raising the awareness of cancer screening among eligible individuals, especially those belonging to racial and ethnic minorities and other medically underserved populations; communicating its benefits and potential harms; developing culturally tailored interventions that address the lack of health literacy and cancer screening knowledge among certain populations; making cancer screening accessible to all—both in availability and cost; and conveying the importance of follow-up visits if the initial screening exam indicates the possibility of cancer. Stakeholders across the cancer care continuum—cancer researchers, physicians, federal regulatory and funding agencies; cancer-focused professional organizations; patient advocates and navigators—are working together to achieve this goal, and many established as well as innovative interventions are being tested across the nation.
In February 2022, the President’s Cancer Panel released the Closing Gaps in Cancer Screening: Connecting People, Communities, and Systems to Improve Equity and Access Report. The report was presented to President Biden and outlined barriers and provided recommendations to improve cancer screening and follow-up care in the United States. In this section, we are highlighting some of the approaches that have proven to be effective not only in increasing the cancer screening awareness, adherence and followup in racial and ethnic minorities, but also reducing or, in some cases, eliminating disparities in cancer mortality (488a).
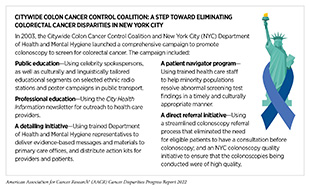
By Implementing Comprehensive Public Health Campaigns
In 2003, the New York City (NYC) Department of Health and Mental Hygiene launched a comprehensive campaign to increase colonoscopy uptake among NHB and Latino individuals as the primary test to screen for colorectal cancer. As a result of the campaign, disparities in colonoscopy were eliminated for these population groups in NYC by 2014.
The proportion of NHB individuals who had received colonoscopy within the last 10 years prior to the launch of the campaign in 2003 was 35 percent compared to White individuals, for whom the proportion was 48 percent. As one example of the effectiveness of the campaign, by 2016, proportions of eligible NHB and White individuals receiving timely colonoscopy were 72 percent and 67 percent, respectively (488)Brown JJ, Asumeng CK, Greenwald D, Weissman M, Zauber A, Striplin J, et al. Decreased Colorectal Cancer Incidence and Mortality in a Diverse Urban Population with Increased Colonoscopy Screening. BMC Public Health 2021;21:1280. [LINK NOT AVAILABLE]. Importantly, the overall CRC incidence and mortality rates were significantly decreased for White, NHB, and Latino populations in New York City between 2003 and 2016 (488)Brown JJ, Asumeng CK, Greenwald D, Weissman M, Zauber A, Striplin J, et al. Decreased Colorectal Cancer Incidence and Mortality in a Diverse Urban Population with Increased Colonoscopy Screening. BMC Public Health 2021;21:1280. [LINK NOT AVAILABLE].
By Increasing Access to Health Insurance
The United States is the only industrialized economy without a universal health care model, making access to quality health care one of the most significant barriers in adherence to recommended cancer screening. In 2018, uninsured women were 26 percent less likely to undergo breast cancer screening compared to those with some form of health insurance, and 15 percent of women avoided medical care because of cost (451)Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in Meeting USPSTF Breast, Cervical, and Colorectal Cancer Screening Guidelines among Women in the United States. Prev Chronic Dis 2021;18:E37. [LINK NOT AVAILABLE]. Another study found that NHB, AI/AN, or Hispanic women were more likely to be diagnosed with locally advanced breast cancer compared to White women and that nearly half of the differences were associated with lack of health insurance among women from minority populations (4)Kaiser Family Foundation. Racial Disparities in Cancer Outcomes, Screening, and Treatment. [updated February 3, 2022, cited 2022 April 22]..
Research has shown that equitable access to health care eliminates disparities. According to recent findings, between 2012—the last data year before expansion of the Affordable Care Act coverage was implemented—and 2020, the share of Hispanic women who were eligible but did not receive a recent mammogram fell by 11 percentage points from 32 percent to 21 percent, reversing a disparity between them and White women, 24 percent and 22 percent of whom were without a recent mammogram in 2012 and 2020, respectively(4)Kaiser Family Foundation. Racial Disparities in Cancer Outcomes, Screening, and Treatment. [updated February 3, 2022, cited 2022 April 22]..
By Developing Culturally Tailored Interventions through Community Engagement
Lack of information about screening recommendations, cultural beliefs, and patient attitudes and behaviors regarding health care visits and cancer screening measures can be significant contributors to lack of or hesitation in getting screened for cancer. Multiple studies have found that culturally and linguistically tailored interventions to enhance uptake of cancer screening among racial and ethnic groups have a high degree of success. In one study, researchers developed a multicomponent intervention to increase cervical cancer screening among Hispanic women along the U.S.-Mexico border. The approach—De Casa en Casa—combined previously successful screening strategies (comprised of reminders, incentives, one-on-one education, and out-of-pocket cost reduction) with a bilingual, culturally tailored educational component (which included community member engagement, culturally tailored material, and culturally tailored method of delivery) and a navigation component (which facilitated screening and diagnostic testing through dedicated patient navigators who helped with making appointments for screening tests, placed reminder calls, and provided transportation if needed). According to the study’s findings, individuals who received intervention were 14 times more likely to be screened compared with those who did not receive the intervention (489)Shokar NK, Calderon-Mora J, Molokwu J, Byrd T, Alomari A, Mallawaarachchi I, et al. Outcomes of a Multicomponent Culturally Tailored Cervical Cancer Screening Intervention among Underserved Hispanic Women (De Casa En Casa). Health Promot Pract 2021;22:112-21. [LINK NOT AVAILABLE]. Researchers have also found other innovative approaches, such as using narrative short films to convey the importance of cervical cancer screening to Spanish-speaking women, to be effective in increasing the uptake of cervical cancer screening in the study populations (128)Murphy ST, Frank LB, Chatterjee JS, Moran MB, Zhao N, Herrera PAd, et al. Comparing the Relative Efficacy of Narrative Vs Nonnarrative Health Messages in Reducing Health Disparities Using a Randomized Trial. American Journal of Public Health 2015;105:2117-23. [LINK NOT AVAILABLE](129)Ochoa CY, Murphy ST, Frank LB, Baezconde-Garbanati LA. Using a Culturally Tailored Narrative to Increase Cervical Cancer Detection among Spanish-Speaking Mexican-American Women. Journal of Cancer Education 2020;35:736-42. [LINK NOT AVAILABLE].
Research also shows that interventions which actively engage community members are often more effective. For example, the Pitt County Breast Wellness Initiative-Education provided culturally tailored breast cancer education and navigation for uninsured and underinsured Black and Latina women in two rural counties in North Carolina (490)Richman AR, Torres E, Wu Q, Kampschroeder AP. Evaluating a Community-Based Breast Cancer Prevention Program for Rural Underserved Latina and Black Women. J Community Health 2020;45:1205-10. [LINK NOT AVAILABLE]. This program trained community members and undergraduate students majoring in public health to educate participating women about breast health and the importance of screening using informational material developed for lay audiences. Sixty-eight percent of women who were eligible but never received a mammogram before received one through the program (490)Richman AR, Torres E, Wu Q, Kampschroeder AP. Evaluating a Community-Based Breast Cancer Prevention Program for Rural Underserved Latina and Black Women. J Community Health 2020;45:1205-10. [LINK NOT AVAILABLE].
By Reducing Structural Barriers
Collecting biospecimens (for example, blood) and/or images for most screening tests require specialized instruments and/or trained health care staff and a visit to a health care facility (see sidebar on Tests for Cancer Screening) and thus present potential structural barriers to adhering to cancer screenings. Researchers are testing strategies to minimize structural barriers to cancer screening. As one example, Kaiser Permanente Northern California—an integrated managed care consortium of eight states and the District of Columbia—initiated an organized, population-based colorectal cancer screening program from 2006 through 2008. The program, which is still in effect, proactively mailed fecal immunochemical tests (FIT) to use at home annually and allowed eligible individuals to request a colonoscopy. Recent findings from the program show that the proportion of individuals who were up to date with screening increased from 42 percent in 2000 to 79-80 percent during the period from 2015 through 2019 among Black persons and from 40 percent in 2000 to 82-83 percent during the period from 2015 through 2019 among White persons. Importantly, the disparity in colorectal cancer–specific mortality between the two groups was nearly eliminated from a difference of 21.6 cases per 100,000 people during 2007-2009 to 1.6 cases per 100,000 people during 2017-2019 (491)Doubeni CA, Corley DA, Zhao W, Lau Y, Jensen CD, Levin TR. Association between Improved Colorectal Screening and Racial Disparities. New England Journal of Medicine 2022;386:796-8. [LINK NOT AVAILABLE].
Another study found that combining text messaging with mailing free, at-home test kits can help boost the number of people who get screened for colorectal cancer. A nearly 10-fold increase in screening completion was observed among those who received a series of reminder texts and a free FIT to use at home compared to those who only received a single text message reminding them that they were overdue for colorectal cancer screening (492)Huf SW, Asch DA, Volpp KG, Reitz C, Mehta SJ. Text Messaging and Opt-out Mailed Outreach in Colorectal Cancer Screening: A Randomized Clinical Trial. J Gen Intern Med 2021;36:1958-64. [LINK NOT AVAILABLE].
Expanding clinic hours and/or offering weekend appointments for cancer screening is another potential strategy for facilitating screening among socioeconomically disadvantaged populations. Individuals belonging to these population groups may seek health maintenance appointments that allow them to avoid taking unpaid time off from work or at times when they have additional childcare options. Patient navigators, such as Sandra Morales, are also drawing on their personal experiences with health care system and playing a pivotal role in helping cancer patients from racial and ethnic minorities with overcoming structural barriers that can otherwise pose serious obstacles to navigating and accessing quality health care.
Improving Communication between Patients and Physicians
Effective communication about health-related information and advice between patients and their providers is pivotal for making informed and shared decisions as well as for receiving quality health care (493)Drossman DA, Chang L, Deutsch JK, Ford AC, Halpert A, Kroenke K, et al. A Review of the Evidence and Recommendations on Communication Skills and the Patient-Provider Relationship: A rome Foundation Working Team Report. Gastroenterology 2021;161:1670-88.e7. [LINK NOT AVAILABLE]. Research has shown that the patient-provider communication regarding cancer screening is influenced by several factors, such as whether the provider is current with knowledge of screening guidelines; whether the patient trusts the provider and the health care system in general; and whether the patient and provider speak the same language. A recent study found that Asian Americans with limited English proficiency were more than 50 percent less likely to be up to date with breast, cervical, or colorectal cancer screening compared to those proficient in English (494)Xie Z, Chen G, Suk R, Dixon B, Jo A, Hong YR. Limited English Proficiency and Screening for Cervical, Breast, and Colorectal Cancers among Asian American Adults. J Racial Ethn Health Disparities 2022. [LINK NOT AVAILABLE].
Harnessing data from electronic health records is one way to promote quality, safety, and efficiency; reduce health disparities; engage patients and families; improve care coordination; and maintain patient health information privacy and security. However, it is equally important to ensure that medically underserved populations have equitable access to the digital services and tools, and computers with high-speed Internet connections, to effectively benefit from new and emerging technologies.