Reducing the Risk of Cancer Development
In this section, you will learn:
- In the United States, 40 percent of all cancers are associated with modifiable risk factors.
- The significant decline in cancer mortality over the past three decades is largely attributable to reductions in smoking and increased cancer screening following the implementation of public health campaigns and policy initiatives.
- Nearly 20 percent of U.S. cancer diagnoses are related to excess body weight, unhealthy dietary patterns, alcohol intake, and physical inactivity.
- Many cases of skin cancer can be prevented by protecting the skin from ultraviolet radiation from the sun and indoor tanning devices.
- Nearly all cases of cervical cancer, as well as many cases of head and neck and anal cancers, can be prevented by HPV vaccination; many cases of liver cancer can be prevented by HBV vaccination.
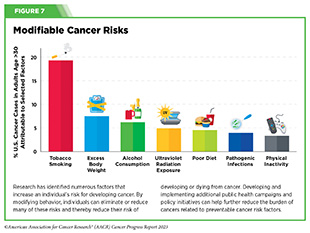
Research in basic, translational, and population sciences has broadened our understanding of the factors that increase an individual’s risk of developing cancer (see Figure 7). Modifiable risk factors, including tobacco use, unhealthy diet, physical inactivity, UV exposure, alcohol consumption, pathogenic infections, and obesity contribute to the development of 40 percent of all cancers. Given that several of these risks can be avoided, many cases of cancer can potentially be prevented. The increased recognition of these risk factors, which also contribute to many other chronic diseases such as those of the cardiovascular system, will help local and national public health organizations increase prevention efforts, lessening the negative health and economic impact of these diseases, including cancer.
Between 1991 and 2020, the United States experienced a 33 percent decline in overall cancer mortality largely due to the implementation of public health campaigns and policy initiatives designed to reduce smoking and increase early detection of cancers (2)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 17. [LINK NOT AVAILABLE]. However, while smoking rates have declined, the increasing prevalence of other risk factors, including obesity among U.S. children and adults, is cause for concern. Additionally, there is a lack of widespread uptake in the United States of preventive interventions such as vaccination against cancer-causing viruses including human papillomavirus (HPV), which is the primary cause of cervical cancer. Addressing and reducing all modifiable risk factors, especially those on the rise such as obesity, are required to continue the downward trend in cancer-related deaths.
Prevalence of modifiable risk factors is higher in segments of the U.S. population that experience cancer disparities, such as racial or ethnic, and sexual and gender minorities, as well as other medically underserved populations. These inequities stem from decades of structural, social, and institutional injustices that have placed disadvantaged populations in unfavorable living environments and contributed to behaviors that increase cancer risk (see Figure 2). For example, racial or ethnic minorities are more likely to live in areas that may have high levels of air pollution, no green spaces for physical activity, and/or little to no availability of healthy food options such as fresh fruits and vegetables. It is important that all stakeholders in public health work together to increase education and access to cancer prevention resources and eliminate the disproportionate burden of cancer risk factors in these populations.
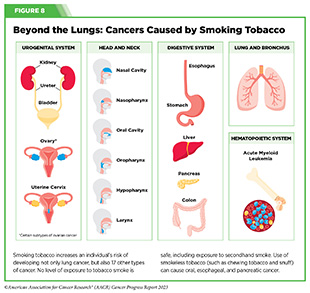
Eliminate Tobacco Use
The use of tobacco products is the leading preventable cause of cancer and is associated with the development of 17 different types of cancer in addition to lung cancer. Nearly 20 percent of all cancer cases and 30 percent of all cancer-related deaths are caused by tobacco products (see Figure 8). On average, people who smoke die ten years earlier than those who have never smoked (122)Jha P, et al. (2013) N Engl J Med, 368: 341. [LINK NOT AVAILABLE](123)The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA)2014. [LINK NOT AVAILABLE]. Research over the past 50 years has consistently demonstrated that byproducts released from smoking tobacco products, such as cigarettes, cause permanent cellular and molecular alterations which lead to cancer (124)Alexandrov LB, et al. (2016) Science, 354: 618. [LINK NOT AVAILABLE]. Furthermore, smoking causes many other chronic conditions including chronic obstructive pulmonary disease (COPD), asthma, chronic bronchitis, emphysema, and many types of cardiovascular diseases. Secondhand smoke is estimated to cause 41,000 deaths each year among adults in the United States, with 7,300 of these due to lung cancer (123)The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA)2014. [LINK NOT AVAILABLE].
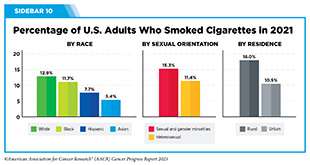
Thanks to nationwide tobacco control initiatives, cigarette smoking among U.S. adults has been on the decline. As of 2021, the most recent year for which such data are available, an estimated 46 million U.S. adults reported using any tobacco product (32)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. [LINK NOT AVAILABLE]. Of those, about 35.6 million reported using a combustible tobacco product (e.g., cigarettes, cigars, pipes) (32)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. [LINK NOT AVAILABLE] (see Sidebar 10). Rates of tobacco use among middle and high school students are also declining, with 16.5 percent of high school students (representing 2.51 million) and 4.5 percent of middle school students (representing 530,000) reporting having ever used tobacco products in 2022, which is down from 5.2 million high school students and 1.3 million middle school students in 2021, representing a 51 and 53 percent reduction, respectively (125)Park-Lee E, et al. (2022) MMWR Morb Mortal Wkly Rep, 71: 1429. [LINK NOT AVAILABLE](126)Gentzke AS, et al. (2022) MMWR Surveill Summ, 71: 1. [LINK NOT AVAILABLE]. Despite the downward trends, these numbers are still of concern, as research shows that nine out of 10 adults who smoke cigarettes daily first try smoking by age 18, necessitating appropriate interventions among younger population to reduce the risk of continued tobacco usage as adults (127)Hu T, et al. (2020) J Am Heart Assoc, 9: e014381. [LINK NOT AVAILABLE].
There is strong evidence that smoking cessation has both immediate and long-term health benefits (129)Ahmed AA, et al. (2015) Circ Heart Fail, 8: 694. [LINK NOT AVAILABLE](130)Duncan MS, et al. (2019) JAMA, 322: 642. [LINK NOT AVAILABLE](131)Centers for Disease Control and Prevention. Benefits of Quitting. Accessed: July 31, 2023. . For instance, those who stop smoking reduce their risk of developing cancers of the larynx, oral cavity, and pharynx by half after 10 years of cessation. After 20 years, the risk of developing these cancers is lowered to the same level as someone who never smokes (132)Centers for Disease Control and Prevention. Smoking and Cancer. Accessed: July 5, 2023. [LINK NOT AVAILABLE].
Evidence-based interventions at local, state, and federal levels, including tobacco price increases, public health campaigns, marketing restrictions, cessation counseling, FDA-approved medications, and smoke-free laws, must be utilized to continue the downward trend of tobacco use (134)Herbst RS, et al. (2022) Clin Cancer Res, 28: 4861. [LINK NOT AVAILABLE].
Other combustible tobacco products (e.g., cigars), smokeless tobacco products (e.g., chewing tobacco and snuff), and water pipes (e.g., hookahs) are also associated with adverse health outcomes, including cancer (135)Gupta S, et al. (2018) Indian J Med Res, 148: 56. [LINK NOT AVAILABLE](136)Patil S, et al. (2022) J Oral Biol Craniofac Res, 12: 439. [LINK NOT AVAILABLE](137)National Cancer Institute. Cigars: Health Effects and Trends. Accessed: July 5, 2023. .
Electronic cigarettes (e-cigarettes) were first introduced into the U.S. market in 2006 and have gained popularity among those who smoke and those who have never smoked, especially among middle and high school students and young adults ages 18 to 24.
The landscape of e-cigarette devices has evolved over the years to include different types of products, such as prefilled pods (e.g., JUUL) or cartridge-based devices, and disposable devices (e.g., Puff Bar), among others. E-cigarettes can deliver nicotine, an extremely addictive substance that is harmful to the developing brain, at similar levels as traditional cigarettes (138)Prochaska JJ, et al. (2022) Tob Control, 31: e88. [LINK NOT AVAILABLE](139)Goriounova NA, et al. (2012) Cold Spring Harb Perspect Med, 2: a012120. [LINK NOT AVAILABLE]. While e-cigarettes emit fewer carcinogens than combustible tobacco, they still expose individuals to toxic chemicals that can damage DNA and trigger inflammation (140)Goniewicz ML, et al. (2018) JAMA Netw Open, 1: e185937. [LINK NOT AVAILABLE](141)Yu V, et al. (2016) Oral Oncol, 52: 58. [LINK NOT AVAILABLE](142)Muthumalage T, et al. (2019) Sci Rep, 9: 19035. [LINK NOT AVAILABLE](143)Tehrani MW, et al. (2021) Chem Res Toxicol, 34: 2216. [LINK NOT AVAILABLE]. Unlike combustible cigarettes, e-cigarettes come in flavors, such as cotton candy and bubblegum, that appeal to youth and are key drivers of e-cigarette use among youth and young adults (144)National Academy of Sciences. Public health consequences of e-cigarettes. Accessed: July 6, 2023. .
After years of increase, the use of e-cigarettes has started to decline among U.S. middle and high school students. Nearly 28 percent of high school students and 11 percent of middle school students reported using e-cigarettes in 2019. While these numbers have declined to 14.1 percent of high school students and 3.3 percent of middle school students in 2022, they are slightly higher than what was reported in 2021 (145)Cooper M, et al. (2022) MMWR Morb Mortal Wkly Rep, 71: 1283. [LINK NOT AVAILABLE](146)Wang TW, et al. (2020) MMWR Morb Mortal Wkly Rep, 69: 1310. [LINK NOT AVAILABLE]. Clearly, more work needs to be done to effectively curb the use of these products in young populations.
The FDA has implemented several restrictions on e-cigarettes in the past year (see Leveraging Policy to Reduce Tobacco-related Illness). It is imperative that all stakeholders continue to work together and implement policies that reduce e-cigarette use among youth and young adults.
Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active
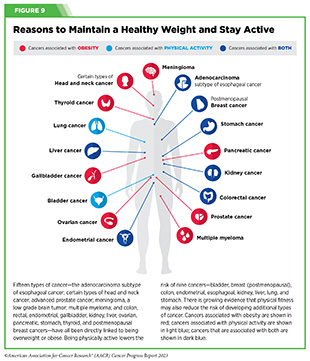
Nearly 20 percent of new cancer cases and 16 percent of cancer deaths in U.S. adults are attributable to a combination of excess body weight, poor diet, physical inactivity, and alcohol consumption (147)Islami F, et al. (2018) CA Cancer J Clin, 68: 31. [LINK NOT AVAILABLE]. Being overweight or obese as an adult increases a person’s risk for 15 types of cancer; being physically active reduces risk for nine types of cancer (see Figure 9). Increased body mass index (BMI), which is a measure of body thickness based on height and weight, is often associated with an individual’s likelihood of developing certain cancers (148)Reeves GK, et al. (2007) BMJ, 335: 1134. [LINK NOT AVAILABLE](149)Pati S, et al. (2023) Cancers (Basel), 15. [LINK NOT AVAILABLE](150)Bhaskaran K, et al. (2014) Lancet, 384: 755. [LINK NOT AVAILABLE]. In addition, specific types of fat, such as abdominal obesity or a higher waist-to-hip ratio, may be a stronger risk factor (151)Lei YY, et al. (2021) BMC Cancer, 21: 839. [LINK NOT AVAILABLE](152)Recalde M, et al. (2023) Nat Commun, 14: 3816. [LINK NOT AVAILABLE]. Being overweight or obese leads to long-lasting inflammation, abnormal levels of insulin, and higher than normal levels of sex hormones, all of which increase the risk of developing certain types of cancer (149)Pati S, et al. (2023) Cancers (Basel), 15. [LINK NOT AVAILABLE].
Among U.S. adults, the rate of obesity from 2017 to 2020 was 41.9 percent (153)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: July 5, 2023. . This is a 37 percent increase from the year 2000, when the rate was 30.5 percent (153)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: July 5, 2023. . During this same time, severe obesity among U.S. adults nearly doubled, with an increase from 4.7 percent to 9.2 percent (153)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: July 5, 2023. . As with smoking adults who are obese have a high risk of many chronic diseases, including diabetes, cardiovascular disease, stroke, and cancer (1)American Association for Cancer Research. AACR Cancer Progress Report 2022. Accessed: July 5, 2023. .
Of increasing concern is the rise in obesity among children and teens (2 to 19 years of age), increasing 300 percent in the past five decades, from five percent in the 1970s to approximately 19.7 percent during the period from 2017 to 2020 (154)Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. Accessed: July 6, 2023. . Recent data show that being overweight or obese during childhood increases the likelihood of developing cancer as adults (155)Jensen BW, et al. (2023) J Natl Cancer Inst, 115: 43. [LINK NOT AVAILABLE].
One emerging area of concern among public health experts is the recent rise in early-onset colorectal cancer that has been partially attributed to the rise in obesity (see The Growing Population Burden of Cancer) (164)Li H, et al. (2022) Gastroenterology, 162: 1088. [LINK NOT AVAILABLE]. In a meta-analysis, which examined 30 studies on early-onset colorectal cancer risk factors, being overweight or obese increased the likelihood of developing early-onset colorectal cancer by 1.2 and 1.5 times, respectively, compared to maintaining a healthy weight (165)Hua H, et al. (2023) Front Oncol, 13: 1132306. [LINK NOT AVAILABLE]. Understanding how modifiable risk factors like obesity, unhealthy diet, and lack of exercise are contributing to the rise in early-onset colorectal cancer is vital for establishing effective prevention efforts.
Weight loss interventions have proven to be effective in reducing or eliminating the risk of cancers associated with obesity. As one example, bariatric surgery, a term used to describe a collection of procedures that are done to help people who are obese lose weight, has been shown to lower the risk of developing and/or dying from certain obesity-associated cancers (166)Adams TD, et al. (2023) Obesity (Silver Spring), 31: 574. [LINK NOT AVAILABLE](167)Clapp B, et al. (2022) Br J Surg, 110: 24. [LINK NOT AVAILABLE](168)Aminian A, et al. (2022) JAMA, 327: 2423. [LINK NOT AVAILABLE]. While further research is needed to elucidate whether bariatric surgery can effectively reduce the burden of all obesity-related cancers, identifying equitable strategies including lifestyle and therapeutic interventions to address obesity must certainly be a top priority for U.S. public health.
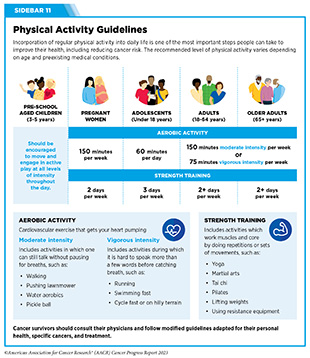
Another effective intervention to reduce weight is through increased physical activity. Unfortunately, many U.S. adults do not meet the minimum recommended physical activity guidelines (see Sidebar 11). According to recent data from CDC, only 25 percent of individuals met the minimum amount of aerobic and muscle-strengthening exercise in 2020 (170)Abildso CG, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 85. [LINK NOT AVAILABLE]. This is concerning because physical activity can reduce the risk of nine types of cancer, with research indicating that, annually, over 46,000 U.S. cancer cases could potentially be avoided if everyone met these guidelines (see Sidebar 11) (171)Minihan AK, et al. (2022) Med Sci Sports Exerc, 54: 417. [LINK NOT AVAILABLE].
Based on a recent study, people who engage in four to five minutes of vigorous physical activity daily can reduce their cancer risk by up to 32 percent (173)Stamatakis E, et al. (2023) JAMA Oncol. [LINK NOT AVAILABLE]. Another study among older adults who engaged in several types of exercise, including running, racquet sports, walking, golf, swimming, and cycling, found that all forms of exercise reduced all-cause, cardiovascular, and cancer mortality, compared to those who did not participate in these activities (see Sidebar 11) (174)Watts EL, et al. (2022) JAMA Netw Open, 5: e2228510. [LINK NOT AVAILABLE]. It is important to note that the type of exercise is not as important as getting the recommended amount of physical activity.
There are many barriers that may prevent individuals from being physically active, including cost and access to fitness facilities, lack of green spaces, and family obligations (176)Withall J, et al. (2011) BMC Public Health, 11: 507. [LINK NOT AVAILABLE]. These barriers are exacerbated in racial and ethnic minorities and other medically underserved populations. Based on recent data, physical inactivity is higher in Hispanics (31.7 percent) and non-Hispanic Blacks (30.3 percent), compared to non-Hispanic Whites (23.4 percent) (177)Centers for Disease Control and Prevention. Physical Inactivity is More Common among Racial and Ethnic Minorities in Most States. Accessed: July 5, 2023. . There are also geographic disparities, with only 16 percent of people in suburban and rural areas meeting the recommended physical activity guidelines, compared to 27.8 percent of those living in urban areas (170)Abildso CG, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 85. [LINK NOT AVAILABLE].
Developing widespread campaigns to increase physical activity in the U.S. population is vital if we are to change the current trends. As one example, The Active People, Healthy Nation initiative aims to help 27 million people become more physically active by 2027 by designing activity-friendly communities, encouraging physical activity at school, and engaging community leaders to implement relevant programs to encourage physical activity.
Poor diet, consisting of processed foods and lacking fresh fruits or vegetables, is responsible for the development of about five percent of all cancers, with several studies demonstrating a link between consumption of highly processed foods and cancer incidence (179)Chang K, et al. (2023) EClinicalMedicine, 56: 101840. [LINK NOT AVAILABLE]. It is therefore concerning that U.S. adults consumed about seven percent more highly processed foods in 2017-2018 than they did in 2001-2002 (180)Juul F, et al. (2022) Am J Clin Nutr, 115: 211. [LINK NOT AVAILABLE].
Highly processed foods lack fiber and include high amounts of added sugar, salt, fats, preservatives, and additives in their ingredients (see Sidebar 12). Research has shown that high consumption of ultra-processed foods is associated with an increased risk of colorectal cancer (181)Wang L, et al. (2022) BMJ, 378: e068921. [LINK NOT AVAILABLE]. On the other hand, a diet rich in fresh fruits and vegetables, nuts, whole grains, and fish can help lower the risk of developing certain cancers and many other chronic conditions. For instance, one study of nearly 80,000 men from diverse backgrounds showed that adherence to a healthy diet lowered risk for certain types of colorectal cancers (182)Hang D, et al. (2023) J Natl Cancer Inst, 115: 155. [LINK NOT AVAILABLE]. There is growing appreciation of following healthy and balanced dietary patterns rather than eating more of a specific nutrient. For instance, a Mediterranean Diet emphasizes consumption of plant-based foods and healthy fats, which allows individuals to customize their diet to fit their tastes and preferences.
The widespread availability and low cost of fast food—food that can be prepared quickly and easily and is sold in restaurants and snack bars as a quick meal or to be taken out—led to 37 percent of U.S. adults (ages 40 to 59) and 45 percent of U.S. young adults (ages 20 to 39) consuming these on any given day during 2013-2016 (184). Unfortunately, fast foods are highly processed, calorie dense, high in salt content, and low in fiber, making them of poor nutritional value. It is also concerning that fast food consumption is higher among racial or ethnic minorities with 43 percent of non-Hispanic Black adults versus 36 percent of non-Hispanic White adults consuming fast food between 2013 and 2016, the most recent timeframe for which these data are available (184)Centers for Disease Control and Prevention. Fast Food Consumption Among Adults in the United States, 2013–2016. Accessed: July 5, 2023. .
Disparities in diet quality among different segments of the U.S. population can be attributed to socioeconomic and geographic factors, which contribute to food insecurity. Food insecurity is defined by the United States Department of Agriculture (USDA) as the lack of access by all people in a household at all times to enough food for an active, healthy life. Studies show that food insecurity is higher among racial or ethnic minorities and those who live in poverty. These communities are often located in neighborhoods that are considered “food deserts,” which are areas that have low availability of healthy foods like fresh fruit and vegetables and an abundance of fast-food options. Community-driven initiatives administered through key partners, such as faith-based organizations, schools, and local food retailers, are one mechanism to promote healthy eating.
Sugar-sweetened beverages are a major contributor to caloric intake among U.S. youth and adults, and there are emerging data indicating that consumption of sugar-sweetened beverages may be associated with an increased risk of cancer (4)American Association for Cancer Research. AACR Cancer Progress Report 2021. Accessed: June 30, 2023. . In certain rural areas, for example the Appalachia region, local interventions have led to a reduction in consumption of sugar-sweetened beverages, and increased consumption of vegetables (185)Norman-Burgdolf H, et al. (2021) Prev Med Rep, 24: 101642. [LINK NOT AVAILABLE]. The Philadelphia Beverage Tax on sugar-sweetened beverages, implemented in 2017, increased the cost of sodas and juices that contain sugar by 1.5 cents per ounce. The tax led to demonstrated reductions in the consumption of sugar-sweetened beverages (186)Hua SV, et al. (2023) JAMA Netw Open, 6: e2323200. [LINK NOT AVAILABLE], with one study indicating as much as a 42 percent drop in the sale of these types of beverages after two years (187)Bleich SN, et al. (2021) JAMA Netw Open, 4: e2113527. [LINK NOT AVAILABLE]. The tax revenue generated is used to fund early-education programs (including free universal pre-K), healthy messaging, and upgrades to playground equipment (188)Edmondson EK, et al. (2022) J Nutr Sci, 11: e67. [LINK NOT AVAILABLE]. Pilot initiatives like these need to be closely examined to determine their long-term health effects and impact on diet, obesity, and cancer burden.
Reduce Risk of Diabetes
Diabetes affects 11.3 percent of the U.S. population, equating to 37.3 million people (189)Centers for Disease Control and Prevention. National Diabetes Statistics Report. Accessed: July 5, 2023. . Evidence shows that having type 1 or type 2 diabetes increases the risk of developing liver, pancreatic, endometrial, colorectal, breast, and bladder cancers. Type 2 diabetes, a condition in which the body cannot regulate sugar properly, can be attributed to genetic factors as well as modifiable risk factors, some of which are also risk factors for cancer, such as obesity, poor diet, physical inactivity, and smoking. Recent studies have shown that many health conditions that are common among those with diabetes, including high levels of insulin and inflammation, may also increase the risk of breast, colorectal, prostate, endometrial, liver, and ovarian cancers, regardless of an individual’s BMI (190)Zhang AMY, et al. (2021) Diabetes Metab J, 45: 285. [LINK NOT AVAILABLE]. Continuing to understand the mechanisms by which diabetes contributes to cancer risk may help identify opportunities for intervention.
Encouragingly, keeping blood sugars low through eating a healthful diet rich with vegetables, fruits, and whole grains; engaging in physical activity; reducing or eliminating alcohol consumption; and stopping smoking can significantly reduce the risk of cancer in people with diabetes. It is essential that patients with diabetes be aware of their increased cancer risk and undergo recommended age- and sex-appropriate cancer screenings.
Limit Alcohol Consumption
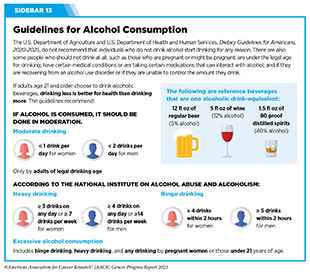
The consumption of alcohol is linked to more than 200 diseases and increases the risk of six different types of cancer including certain types of head and neck cancer, esophageal squamous cell carcinoma, and breast, colorectal, liver, and stomach cancers. Nearly four percent of cancers diagnosed worldwide in 2020 can be attributed to alcohol consumption (191)Rumgay H, et al. (2021) Lancet Oncol, 22:1071. [LINK NOT AVAILABLE]. In the U.S., it is estimated that from 2013 to 2016, 75,000 cancer cases and 19,000 cancer deaths were linked to alcohol (192)Goding Sauer A, et al. (2021) Cancer Epidemiol, 71: 101893. [LINK NOT AVAILABLE]. All alcoholic beverages pose a risk for cancer development because they contain ethanol, which can modulate hormones, and its byproducts can damage DNA, which increases the risk of developing cancers (193)National Cancer Institute. Alcohol and Cancer Risk Fact Sheet. Accessed: July 5, 2023. .
The greatest risks are associated with long-term alcohol consumption and binge-drinking, i.e., when large amounts of alcohol are consumed in a short period of time (194)White AJ, et al. (2017) Am J Epidemiol, 186: 541. [LINK NOT AVAILABLE]. Even light intake of alcohol can increase an individual’s risk for certain cancers, while moderate drinking can increase the risk of developing certain cancers of the head and neck, breast, and colon and rectum (195)Bagnardi V, et al. (2015) Br J Cancer, 112: 580. [LINK NOT AVAILABLE](196)Cao Y, et al. (2015) BMJ, 351: h4238. [LINK NOT AVAILABLE](197)Choi YJ, et al. (2018) Cancer Res Treat, 50: 474. [LINK NOT AVAILABLE](198)Yoo JE, et al. (2021) JAMA Netw Open, 4: e2120382. [LINK NOT AVAILABLE]. Following guidelines for alcohol consumption (see Sidebar 13) can help to lower the risk of developing alcohol-related cancers.
Research indicates that those who reduce or stop drinking alcohol can decrease their risk of developing alcohol-related cancers by eight percent and can reduce their risk of all cancer by four percent compared to those who sustain or increase their consumption of alcohol (200)Gapstur SM et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 5. [LINK NOT AVAILABLE](201)Yoo JE, et al. (2022) JAMA Netw Open, 5: e2228544. [LINK NOT AVAILABLE]. Public messaging campaigns (such as cancer-specific warning labels displayed on alcoholic beverages) must be considered along with effective clinical strategies to reduce the burden of alcohol-related cancers.
Future efforts focused on evidence-based policy interventions, such as regulating the number of alcohol stores in a given area, and increased taxes and prices need to be implemented to curb the consumption of alcohol.
Protect Skin from UV Exposure
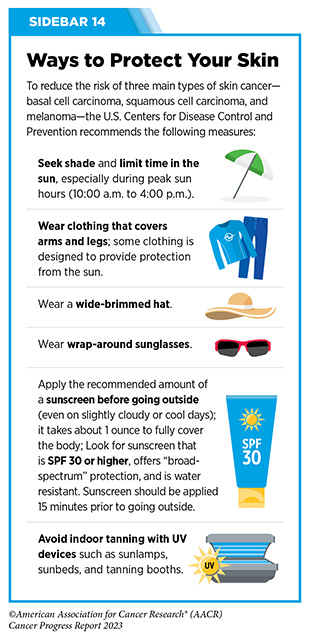
Ultraviolet (UV) radiation is a type of light emitted primarily from the sun but also from artificial sources, such as tanning beds. Exposure to UV radiation can lead to the development of skin cancers, including basal cell carcinoma, squamous cell carcinoma, and melanoma, which is the most aggressive form of skin cancer. In fact, UV radiation accounts for 95 percent of skin melanomas and six percent of all cancers (147)Islami F, et al. (2018) CA Cancer J Clin, 68: 31. [LINK NOT AVAILABLE]. This is because UV radiation can damage cellular DNA with continued exposure leading to cancer.
Anyone can develop skin cancer, but some people are at a higher risk, especially those who are light skinned and get easily sunburned.
It has been reported that there is a lack of understanding in the U.S. population regarding how skin cancer develops and when to use sun protection (203)Strome A, et al. (2021) JAMA Netw Open, 4: e2134550. [LINK NOT AVAILABLE]. According to data from the CDC, 29 percent of U.S. adults and 64 percent of adolescents experienced sunburn at least once in the past year in 2021 (204)Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS). Accessed: July 5, 2023. (205)Centers for Disease Control and Prevention. National Health Interview Survey. Accessed: July 5, 2023. . This is concerning, as severe sunburns increase the risk of developing all three types of skin cancer (up to two and a half times for melanoma), compared to no history of severe sunburn (206)Wu S, et al. (2016) Am J Epidemiol, 183: 824. [LINK NOT AVAILABLE]. One study reported that women who experienced at least five episodes of severe sunburns between the ages of 15 and 20 years were 80 percent more likely to develop melanoma later in life, compared to those who did not experience sunburns (207)Wu S, et al. (2014) Cancer Epidemiol Biomarkers Prev, 23: 1080. [LINK NOT AVAILABLE].
One common misconception is that people cannot get sunburned on cloudy days. However, up to 80 percent of the sun’s harmful UV rays can penetrate clouds. It is recommended that individuals practice sun-safe habits anytime they are outside to limit exposure to harmful UV radiation (see Sidebar 14).
It is encouraging that the use of tanning beds, particularly among U.S. youth, has dramatically decreased in the past decade. Implementing legislation that restricts the use of tanning beds among youth is important to prevent use of these devices, especially because youth who use tanning beds by 17 years of age are twice as likely to continue using these devices as adults (208)Solazzo AL, et al. (2020) J Adolesc Health, 67: 609. [LINK NOT AVAILABLE]. Currently, 44 states and the District of Columbia either ban or regulate the use of indoor tanning devices by minors (209)Skin Cancer Foundation. Indoor Tanning Legislation: Here’s Where We Stand. Accessed: July 5, 2023. . All states should enact legislation banning indoor tanning for minors, to continue the downward trend of tanning bed usage, especially among youth.
Prevent and Eliminate Infection from Cancer-causing Pathogens
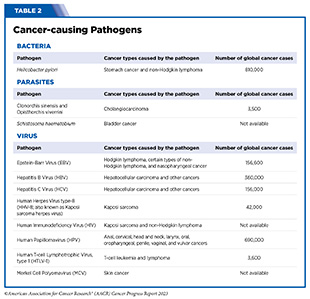
Cancer-causing pathogens (bacteria, viruses, and parasites) increase a person’s risk for several types of cancer (see Table 2). Infection with these agents can change the way a cell behaves, weaken the immune system, and cause chronic inflammation, all of which can lead to cancer. In the United States, about three percent of all cancer cases are attributable to infection with pathogens (147)Islami F, et al. (2018) CA Cancer J Clin, 68: 31. [LINK NOT AVAILABLE]. Globally, an estimated 13 percent (2.2 million) of all cancer cases in 2018 were attributable to pathogenic infections, with more than 90 percent of these cases attributable to four pathogens: human papillomavirus (HPV), hepatitis B (HBV), hepatitis C (HCV), and Helicobacter pylori (212)de Martel C, et al. (2020) Lancet Glob Health, 8: e180. [LINK NOT AVAILABLE].
Individuals can significantly lower their risks by protecting themselves from infection or by seeking treatment, if available, to eliminate an infection (see Sidebar 15).
Human papillomavirus is a group of more than 200 related viruses that are responsible for almost all cervical cancers, 90 percent of anal cancers, and 70 percent of oropharyngeal cancers, as well as most penile, vaginal, and vulvar cancers. While most HPV infections do not cause cancer, those that are persistent and with high-risk HPV virus types can lead to cancer. These high-risk HPVs cause three percent of all cancers in women and two percent in men in the United States (213)Centers for Disease Control and Prevention. Basic information about HPV and cancer. Accessed: July 28, 2022. . Globally, HPV-related cancers comprise about five percent of all cancers (214)National Cancer Institute. HPV and Cancer. Accessed: August 11, 2022. .
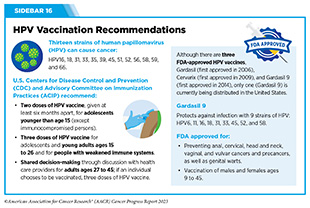
Fortunately, the most recently approved vaccine for HPV, Gardasil 9, protects against nine of the 13 different types of cancer-causing HPV strains. This vaccine has been extremely effective in reducing the incidence of cervical cancer among 20- to 24-year-old women, the first group to become eligible after the U.S. approval of the vaccine in 2006. The most recent data show that between 2012 and 2019, rates of cervical cancer declined by 65 percent among U.S. women in their early 20s, compared to only a 33 percent reduction in the previous decade (2005-2012) (28)American Cancer Society. Cancer Facts and Figures. Accessed: July 5, 2023. .
The HPV vaccine is approved for males and females ages nine to 45, with recommendations for the first doses beginning at age 11 to 12 (see Sidebar 16). Despite the positive impact of the vaccine on reducing cervical cancer incidence, the uptake of the HPV vaccine has been suboptimal in the United States. In 2021, only 76.9 percent of adolescents ages 13 to 17 had received one dose of the HPV vaccine and only 61.7 percent had received the recommended two doses (215)Pingali C, et al. (2022) MMWR Morb Mortal Wkly Rep, 71: 1101. [LINK NOT AVAILABLE]. This stands in sharp contrast to other countries, such as the United Kingdom, where high uptake of HPV vaccination among 12- to 13-year-old girls has led to an 87 percent reduction in cervical cancer among women in their 20s (216)Torjesen I (2021) BMJ, 375: n2689. [LINK NOT AVAILABLE].
Programs designed to increase rates of HPV vaccination in the U.S., such as The Healthy People Initiative, which aims to vaccinate 80 percent of the eligible population, using strategies, including the implementation of vaccination information systems, patient reminders, and vaccination programs in schools can have immense public health benefit (217)Healthy People 2030. Increase the proportion of adolescents who get recommended doses of the HPV vaccine — IID‑08. Accessed: July 5, 2023. .
Chronic infection with HBV and HCV, viruses that cause liver inflammation and damage, can lead to liver cancer and other malignancies including non-Hodgkin lymphoma (NHL), if left untreated (218)Alkrekshi A, et al. (2021) Clin Lymphoma Myeloma Leuk, 21: e832. [LINK NOT AVAILABLE](219)Lai YR, et al. (2022) Cancers (Basel), 14. [LINK NOT AVAILABLE]. After new reported cases of HBV remained stable through 2013 until 2019, there was an abrupt decrease of 32 percent reported cases in 2020, potentially attributable to the COVID-19 pandemic, which may have led to reduced testing but not necessarily reduced infections (220)Center for Disease Control and Prevention. 2020 Viral Hepatitis Surveillance Report. Accessed: July 5, 2023. . In contrast, cases of HCV have doubled since 2013, with an increase of 15 percent between 2019 and 2020 (220)Center for Disease Control and Prevention. 2020 Viral Hepatitis Surveillance Report. Accessed: July 5, 2023. . These numbers are concerning, as HBV is preventable with vaccination and HCV can be cured using antiviral medications.
To eliminate viral hepatitis as a public health threat, the U.S. Department of Health and Human Services released the Viral Hepatitis Strategic Plan for the United States: A Roadmap to Elimination (2021-2025). The primary goals listed in the report are to prevent new infections, improve hepatitis-related health outcomes for infected individuals, reduce disparities and health inequities related to hepatitis, improve surveillance of viral hepatitis, and bring together all relevant stakeholders in coordinating efforts to address the hepatitis epidemic.
Individuals infected with human immunodeficiency virus (HIV) have an elevated risk of Kaposi sarcoma, NHL, and cervical cancer; these are called AIDS-defining cancers because they are more likely to occur in people who are infected with HIV, which is the virus that causes AIDS (221)National Cancer Institute. HIV Infection and Cancer Risk – NCI. Accessed: July 31, 2023. . This higher risk is attributable to HIV infection, which weakens the immune system. Prior to highly active antiretroviral therapy (HAART) in 1996, people infected with HIV had a 2,800-fold higher risk of Kaposi sarcoma compared to the general population (222)Yarchoan R, et al. (2018) New England Journal of Medicine, 378: 1029. [LINK NOT AVAILABLE]. Since HAART, there has been a steady decline in incidence of Kaposi sarcoma; however, rates remain 800-fold higher than in the general population (223)Shiels MS, et al. (2017) Curr Opin HIV AIDS, 12: 6. [LINK NOT AVAILABLE]. As the population living with HIV continues to age, the burden of cancers, particularly non-AIDS-defining cancers (such as anal, liver, and lung cancers) will continue to rise (224)Hernandez-Ramirez RU, et al. (2017) Lancet HIV, 4: e495. [LINK NOT AVAILABLE]. One study reported that incidence of lung cancer in people with HIV age 60 years and older is higher than the two most common AIDS-defining cancers, NHL and Kaposi sarcoma (225)Haas CB, et al. (2022) Lancet HIV, 9: e700. [LINK NOT AVAILABLE].
Limit Exposure to Environmental Risk Factors
Environmental pollutants are encountered in the air, drinking water, and food making them nearly impossible to avoid. Federal agencies, including the Environmental Protection Agency and Department of Health and Human Services, set guidelines for the acceptable exposure limits allowed in the environment. However, some individuals experience higher levels of exposure to certain pollutants due to their occupation, living conditions, or daily activities. Exposure to higher than acceptable levels of certain pollutants, without appropriate protection, can increase the risk of certain diseases. Environmental carcinogens, which are substances that can lead to cancer and are present in the environment, include arsenic, asbestos, radon, lead, radiation, and other chemical pollutants. The International Agency for Research on Cancer (IARC) and the U.S. National Toxicology Program (NTP) are both responsible for evaluating substances and exposures and classifying them as carcinogens at the global and national level, respectively.
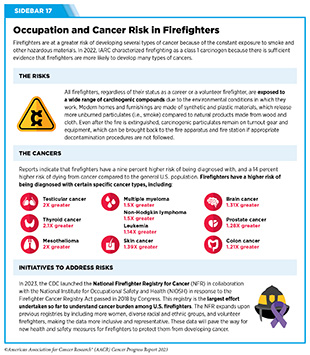
Higher than normal levels of exposure to carcinogens have led IARC to classify certain occupations, such as firefighting and painting, and work environments, such as iron and steel foundries or working around welding fumes, as class 1 carcinogens, meaning they are cancer-causing to humans (see Sidebar 17).
It can be difficult for some segments of the U.S. population to avoid or reduce their exposure to environmental carcinogens. For instance, racial or ethnic minorities and people living in poverty are often at increased risk of being exposed to high levels of air pollution, which the IARC has designated as a potential cause of cancer in humans. One type of air pollution termed particle pollution refers to a mix of tiny solid and liquid particles that are in the air we breathe. Nearly 36 percent of the U.S. population, representing 119.6 million people, live in places with unhealthy levels of particle pollution (236)American Lung Association. State of the Air 2023. Accessed: July 5, 2023. [tooltip text="237" url="https://ntp.niehs.nih.gov/sites/default/files/ntp/results/pubs/cancer_assessment/lanfinal20210400_508.pdf" newwindow="true"]National Toxicology Program. National Toxicology Program Cancer Hazard Assessment Report on Night Shift Work and Light at Night. Accessed: July 5, 2023. . New laws, regulations, and policies to reduce the release of pollutants into the atmosphere are necessary to minimize the long-term, adverse health effects of air pollution, including cancer.
Other exposures including chronic stress, lack of sleep, and night-shift work have also been shown to increase a person’s risk of developing certain types of cancer (237)National Toxicology Program. National Toxicology Program Cancer Hazard Assessment Report on Night Shift Work and Light at Night. Accessed: July 5, 2023. .
The CDC reports that about 11 million adults in the U.S. frequently work night shifts, with certain groups such as men, and Black and non-Hispanic individuals, more likely to do this type of work. In one recent study, researchers found that women age 50 or older who had both day and night shifts were twice as likely to develop breast cancer compared to those who only worked day shifts (238)International Agency for Research on Cancer. Night Shift. Accessed: July 5, 2023. . Although the underlying mechanisms are not clear, researchers believe that disruption of the body’s circadian rhythm (i.e., the internal clock) can alter biological processes that normally help prevent cancer development. Emerging research indicates that avoiding lighting that disrupts circadian rhythms, for example, lighting that is low in blue light may help reduce cancer risk (239)Figueiro MG, et al. (2020) J Safety Res, 74: 169. [LINK NOT AVAILABLE](240)Figueiro MG, et al. (2010) Int J Endocrinol, 2010: 829351. [LINK NOT AVAILABLE](241)Faraut B, et al. (2019) Front Neurosci, 13: 1366. [LINK NOT AVAILABLE]. Long-term research is needed to understand how exposure to certain light sources, particularly at night, may contribute to cancer risk.
As we learn more about environmental and occupational cancer risk factors and identify those segments of the U.S. population who are exposed to these factors, new and equitable policies need to be developed and implemented to reduce cancer risk and improve the health of all populations.
Be Cognizant of Hormonal Factors
Pregnancy and Breastfeeding
Historically, parous women – women who have given birth – were known to be less likely to develop breast cancer than nulliparous women – women who have never given birth. This protective effect of pregnancy reduces the risk of developing a type of breast cancer called estrogen receptor-positive tumor (242)Nichols HB, et al. (2019) Ann Intern Med, 170: 22. [LINK NOT AVAILABLE](243)Ambrosone CB, et al. (2020) Cancer Res, 80: 4871. [LINK NOT AVAILABLE](244)Jung AY, et al. (2022) J Natl Cancer Inst. [LINK NOT AVAILABLE]. Importantly, the risk reduction is only manifested after a decade or longer following a woman’s last pregnancy, with greater protection conferred with increasing time (242)Nichols HB, et al. (2019) Ann Intern Med, 170: 22. [LINK NOT AVAILABLE](243)Ambrosone CB, et al. (2020) Cancer Res, 80: 4871. [LINK NOT AVAILABLE](244)Jung AY, et al. (2022) J Natl Cancer Inst. [LINK NOT AVAILABLE]. Parous women are at reduced risk for developing breast cancer after menopause (when most breast cancers are diagnosed) compared to their nulliparous peers.
In contrast, between five to ten years after giving birth, known as the postpartum period, women face a short-term, elevated risk for a different type of breast cancer called estrogen receptor-negative tumors compared to women who have never given birth (245)Vohra SN, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 561. [LINK NOT AVAILABLE]. Finally, young women are at a higher risk of developing triple-negative breast cancer; the risk is elevated in the postpartum period but decreases over time (242)Nichols HB, et al. (2019) Ann Intern Med, 170: 22. [LINK NOT AVAILABLE](244)Jung AY, et al. (2022) J Natl Cancer Inst. [LINK NOT AVAILABLE](245)Vohra SN, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 561. [LINK NOT AVAILABLE]. Identifying interventions that may alleviate the tumor-promoting potential of recent childbirth, and determining the best therapeutic options to treat postpartum breast cancer, are areas of extensive investigation.
There is evidence that breastfeeding can be protective against the development of estrogen receptor-negative breast cancer in mothers that is associated with giving birth (246)Millikan RC, et al. (2008) Breast Cancer Res Treat, 109: 123. [LINK NOT AVAILABLE](247)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723. [LINK NOT AVAILABLE](248)Fortner RT, et al. (2019) Breast Cancer Res, 21: 40. [LINK NOT AVAILABLE], with increased duration of breastfeeding associated with further decrease in risk (160)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the risk of cancer. Accessed: July 6, 2023. (244)Jung AY, et al. (2022) J Natl Cancer Inst. [LINK NOT AVAILABLE](247)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723. [LINK NOT AVAILABLE](249)Anstey EH, et al. (2017) Am J Prev Med, 53: S40. [LINK NOT AVAILABLE](250)Palmer JR, et al. (2014) J Natl Cancer Inst, 106. [LINK NOT AVAILABLE](251)John EM, et al. (2018) Int J Cancer, 142: 2273. [LINK NOT AVAILABLE]. Emerging data suggest that breastfeeding may also be associated with a lower risk of ovarian cancer development (252)Li DP, et al. (2014) Asian Pac J Cancer Prev, 15: 4829. [LINK NOT AVAILABLE](253)Babic A, et al. (2020) JAMA Oncol, 6: e200421. [LINK NOT AVAILABLE]. The protective effects of breastfeeding are seen in both Black and White women (160)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the risk of cancer. Accessed: July 6, 2023. (247)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723. [LINK NOT AVAILABLE](249)Anstey EH, et al. (2017) Am J Prev Med, 53: S40. [LINK NOT AVAILABLE](250)Palmer JR, et al. (2014) J Natl Cancer Inst, 106. [LINK NOT AVAILABLE]. Notably, the increased risk of triple-negative breast cancer diagnosis associated with giving birth can be reduced by breastfeeding, with longer durations of breastfeeding further decreasing the risk (160)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the risk of cancer. Accessed: July 6, 2023. (249)Anstey EH, et al. (2017) Am J Prev Med, 53: S40. [LINK NOT AVAILABLE](250)Palmer JR, et al. (2014) J Natl Cancer Inst, 106. [LINK NOT AVAILABLE](254)Ma H, et al. (2017) Breast Cancer Res, 19: 6. [LINK NOT AVAILABLE]. Beyond protecting the mother, emerging data suggest that breastfeeding can also reduce the risk of children developing leukemia. The protective effect increased proportionally with duration of breastfeeding (255)Su Q, et al. (2021) BMC Med, 19: 90. [LINK NOT AVAILABLE](256)Amitay EL, et al. (2015) JAMA Pediatr, 169: e151025. [LINK NOT AVAILABLE].
While breastfeeding is not always an option, the awareness of the benefits of breastfeeding in reducing cancer risk is low among U.S. women (258)Hoyt-Austin A, et al. (2020) Obstet Gynecol, 136: 1154. [LINK NOT AVAILABLE]. Culturally tailored public education and implementation of health policies in support of lactation are needed, specifically for medically underserved populations, such as young Black women, who have a lower prevalence of breastfeeding and a higher incidence of aggressive breast cancers compared to all other U.S. racial and ethnic groups (259)Chiang KV, et al. (2021) MMWR Morb Mortal Wkly Rep, 70: 769. [LINK NOT AVAILABLE](260)Beauregard JL, et al. (2019) MMWR Morb Mortal Wkly Rep, 68: 745. [LINK NOT AVAILABLE].
Hormone Replacement Therapy
Hormone replacement therapy (HRT) refers to treatments that aim to relieve the common symptoms of menopause and the long-term biological changes, such as bone loss, that take place after menopause. These changes occur due to the decline in the levels of the hormones estrogen and progesterone. Hormone replacement therapy usually involves treatment with estrogen and progestin or estrogen alone in women who have undergone a hysterectomy. This is because when estrogen is given alone, but not in combination with progestin, it is associated with an increased risk of endometrial cancer, a type of cancer that forms in the tissue lining of the uterus.
Data show that women who use the estrogen and progestin combination have an increased risk of developing breast cancer (261)Chlebowski RT, et al. (2020) JAMA, 324: 369. [LINK NOT AVAILABLE](262)Chlebowski RT, et al. (2008) Arch Intern Med, 168: 370. [LINK NOT AVAILABLE]. The risk is greater with longer duration of use and is nearly two-fold higher among women who have used estrogen and progestin in combination for 10 years or longer compared to those who never used HRT (263)Chlebowski RT, et al. (2009) N Engl J Med, 360: 573. [LINK NOT AVAILABLE](264)Collaborative Group on Hormonal Factors in Breast C (2019) Lancet, 394: 1159. [LINK NOT AVAILABLE](265)Wang SM, et al. (2020) Breast Cancer Res, 22: 129. [LINK NOT AVAILABLE]. Women who are no longer using HRT have a lower risk than current users but remain at an elevated risk for more than a decade after they have stopped taking the drugs (264)Collaborative Group on Hormonal Factors in Breast C (2019) Lancet, 394: 1159. [LINK NOT AVAILABLE]. Individuals who seek HRT should discuss with their health care providers the advantages and possible risks, before deciding what is right for them.
One area of ongoing investigation in exogenous hormone use is the differential cancer risks among individuals undergoing gender-affirming hormonal therapy (266)Jackson SS, et al. (2022) Trends Cancer, 8: 273. [LINK NOT AVAILABLE]. While current data are very limited, there is emerging evidence indicating an increased risk of breast cancer but a lower risk of prostate cancer among trans women who received gender-affirming hormonal therapy compared to age-matched cisgender men. Trans men who received gender affirming hormonal therapy had a lower risk of breast cancer compared to age-matched cisgender women (267)de Blok CJM, et al. (2019) BMJ, 365: l1652. [LINK NOT AVAILABLE](268)de Nie I, et al. (2020) J Clin Endocrinol Metab, 105: e3293. [LINK NOT AVAILABLE]. New evidence indicates that this lower risk of breast cancer in trans men may be due to protective effects of receiving androgen therapy during their transition (269)Raths F, et al. (2023) Cell Genom, 3: 100272. [LINK NOT AVAILABLE]. Long-term, population-based studies are needed to comprehensively assess the risk of cancers in these understudied and medically underserved populations.
Next Section: Screening for Early Detection Previous Section: Understanding the Path to Cancer Development