- Research: Driving Progress Against Cancer
- Cancer: An Ongoing Public Health Challenge
- Inequities in the Burden of Cancer in the United States
- Variable Progress Against Different Types of Cancer and Stages of Diagnosis
- The Growing Population Burden of Cancer
- The Global Burden of Cancer
- Funding Cancer Research: A Vital Investment
Cancer in 2023
In this section, you will learn:
- In the United States, the overall cancer death rate has been steadily declining since the 1990s, with the reductions between 1991 and 2020 translating into more than 3.8 million cancer deaths avoided.
- The decline in overall U.S. cancer death rates is driven by steady declines in mortality from cancers of the breast, colon and rectum, lung, and prostate.
- More than 18 million cancer survivors were living in the United States as of January 1, 2022.
- Progress has not been uniform against all cancer types or all subtypes and stages of a given cancer type.
- There are stark inequities in the cancer burden among many sociodemographic groups within the United States; these inequities occur across the cancer continuum and are driven largely by social factors.
- The economic burden of cancer both on individuals and the U.S. health care system is expected to rise in the coming decades, highlighting the urgent need for more research to accelerate the pace of progress against cancer.
Research: Driving Progress Against Cancer
Research is the backbone of progress against cancer because it is the driving force behind every breakthrough that enhances survival and quality of life and every new policy or program designed to improve public health. Discoveries across the major areas of cancer research, including basic, clinical, translational, and population sciences, provide the foundation for advances in cancer prevention, detection, diagnosis, treatment, and survivorship.
Every clinical advance as well as every policy that spurs progress against cancer is the culmination of a complex process that requires collaboration over the course of many years among numerous different stakeholders committed to fundamentally changing the face of this devastating disease (see Sidebar 1).
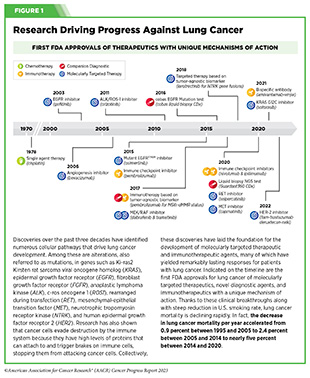
The remarkable advances being made against cancer—in particular, improvements in prevention, early detection, and treatment—are resulting in a steady decline in U.S. cancer death rates year after year. In fact, the age-adjusted overall cancer death rate has fallen by 33 percent between 1991 and 2020, a reduction that translates into averting an estimated 3.8 million deaths from cancer (2)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 17. [LINK NOT AVAILABLE]. The reduction in overall U.S. cancer mortality rate is driven largely by the decline in lung cancer death rate, the pace of which has accelerated in recent years because of reduction in smoking and advances in early detection and treatment (see Figure 1). Reduction in death rates for melanoma, colorectal cancer, prostate cancer, and female breast cancer has also contributed to overall progress against U.S. cancer mortality (2)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 17. [LINK NOT AVAILABLE].
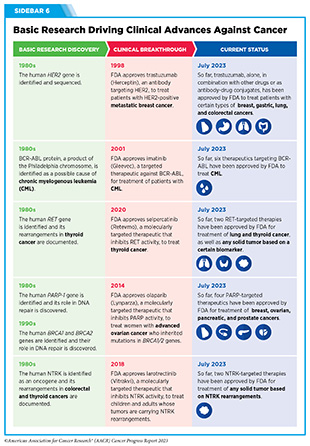
Research-driven advances in treatment are reflected in the steady declines in death rates for melanoma, leukemia, and kidney cancer (2)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 17. [LINK NOT AVAILABLE]. The death rate for chronic myeloid leukemia (CML), a cancer of the blood and bone marrow, for instance, has declined by 70 percent between 1975 and 2020 (5)Surveillance, Epidemiology, and End Results (SEER) Program. Accessed: July 5, 2023. . This progress can be attributed to groundbreaking basic research discoveries from the 1960s through 1980s that identified the mechanistic underpinnings of the disease and propelled the development of a cascade of new treatments for CML (see Sidebar 6) (6)Howlader N, et al. (2023) Cancer Epidemiol Biomarkers Prev, 32: 744. [LINK NOT AVAILABLE].
Among children (14 years or younger) and adolescents (15 to 19 years), overall cancer death rates have declined by 70 percent and 64 percent, respectively, between 1970 and 2020, driven largely by improvements in treatment (2)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 17. [LINK NOT AVAILABLE].
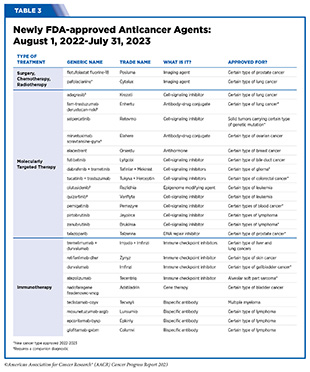
Among the major advances made across the clinical cancer care continuum from August 1, 2022, to July 31, 2023, are 14 new anticancer therapeutics approved for use by FDA (see Table 3). During this period, FDA also approved new uses for 12 previously approved anticancer therapeutics (see Table 3, p. 77), two agents to improve quality of life for patients with cancer undergoing active treatment, two new imaging agents to help visualize cancerous cells during surgery (see Visualizing Lung Cancers More Precisely During Surgery and Imaging Prostate Cancer More Clearly) and several artificial intelligence-based tools to improve detection and diagnosis of cancers (see Sidebar 24). Collectively, advances such as these are helping increase the number of children and adults who live longer and fuller lives after a cancer diagnosis. As of January 1, 2022, the most recent date for which such estimate is available, more than 18 million individuals with a history of cancer were alive in the United States (7)Miller KD, et al. (2022) CA Cancer J Clin, 0: 1. [LINK NOT AVAILABLE]. Recent studies indicate that the number of U.S. individuals living despite being diagnosed with metastatic disease has increased since the 1990s and this number is estimated to grow considerably in the coming years (8)Gallicchio L, et al. (2022) J Natl Cancer Inst, 114: 1476. [LINK NOT AVAILABLE]. This increase is attributable to the advances in treatments that are available for patients with metastatic cancers.
Cancer: An Ongoing Public Health Challenge
Although incredible progress has been made against cancer, it continues to be an enormous public health challenge in the United States and around the world (see Sidebar 4). In the United States alone, an estimated 1,958,310 new cases of cancer will be diagnosed in 2023 and 609,820 people will die from the disease (see Table 1). Men have a higher incidence of many cancer types, including bladder, colon, and brain cancer compared to women and ongoing research is evaluating the role of a range of biological factors including genetics, epigenetics, metabolism, and immunity in mediating these differences.
Unfortunately, many population groups in the United States experience a disproportionately high rate of cancer incidence and death attributable largely to socioeconomic disadvantages. It should also be noted that current estimates of cancer burden do not reflect the adverse impact of COVID-19, which caused serious declines in screening, early detection, and new cancer diagnoses, and which continues to take a toll on cancer care especially among the medically underserved populations (9)American Association for Cancer Research. AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care. Accessed: June 30, 2022. (10)Berrian J, et al. (2023) Cancer Med, 12: 7381. [LINK NOT AVAILABLE](11)Zhao J, et al. (2023) JCO Oncol Pract: OP2200522. [LINK NOT AVAILABLE]. Ongoing monitoring of cancer-related population-based data is warranted to assess the long-term consequences of COVID-19 on cancer burden in the United States.
Inequities in the Burden of Cancer in the United States
While we are making unprecedented advances against cancer, the grim reality is that these advances have not benefited everyone equally. Because of a long history of structural inequities and systemic injustices in the United States, certain segments of the population continue to shoulder a disproportionate burden of adverse health conditions, including cancer.
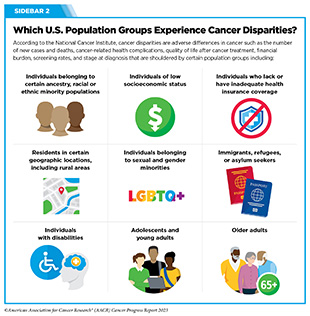
Cancer disparities are one of the most pressing public health challenges in the United States. The National Cancer Institute (NCI) defines cancer disparities as adverse differences in cancer, such as number of new cases, number of deaths, cancer-related health complications, survivorship and quality of life after cancer treatment, screening rates, and stage at diagnosis that exist among certain population groups (see Sidebar 2).
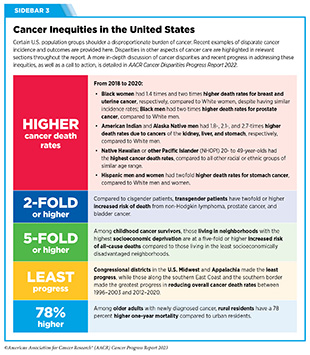
As outlined in the AACR Cancer Disparities Progress Report 2022 (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2023. , racial and ethnic minorities and other medically underserved U.S. populations shoulder a disproportionately higher burden of cancer (see Sidebar 3).
Individuals who are Black have the highest death rates and lowest survival rates of any racial or ethnic group in the U.S. for most cancers, largely driven by structural and systemic inequities (14)American Cancer Society. Cancer Facts and Figures for African Americans 2019-2021. Accessed: July 28, 2023. . While the disparity in the overall cancer death rate between Black and White populations has narrowed by half over the last two decades, Black individuals still had a 12 percent higher overall cancer death rate compared to White individuals, and the highest death rate from cancer among all U.S. racial or ethnic groups in 2020 (5)Surveillance, Epidemiology, and End Results (SEER) Program. Accessed: July 5, 2023. . American Indian and Alaska Native (AIAN) individuals are a culturally and geographically diverse U.S. population group who experience a disproportionally high prevalence of several chronic illnesses, including many cancers, largely because of barriers to quality health care (15)Kratzer TB, et al. (2023) CA Cancer J Clin, 73: 120. [LINK NOT AVAILABLE]. Cancer is the leading cause of death in the U.S. Hispanic population, the second largest racial or ethnic group in the continental United States and Hawaii, whereas heart disease is the leading cause of death in the non- Hispanic White population (16)Miller KD, et al. (2021) CA Cancer J Clin, 71: 466. [LINK NOT AVAILABLE].
Researchers are increasingly recognizing the heterogeneity in cancer burden among individuals within each of the major racial or ethnic minority groups (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2023. . As one example, the U.S. Asian population has ancestry in numerous countries of origin and the Native Hawaiian or other Pacific Islander (NHOPI) population comprises more than 25 diverse subgroups with distinct variations in historical backgrounds, languages, and cultural traditions. Striking disparities in cancer death rates between NHOPI and Asian individuals have been identified since national death certificates included a new racial classification system which separated NHOPI individuals from Asian individuals, two populations that are frequently aggregated in cancer epidemiological data (17)Haque AT, et al. (2023) J Natl Cancer Inst. [LINK NOT AVAILABLE]. These findings highlight the vital importance of disaggregated cancer data to fully understand cancer disparities and develop effective strategies for achieving health equity.
In addition to racial or ethnic minorities, many other segments of the U.S. population shoulder a disproportionate burden of cancer (see Sidebar 2). These include residents in rural areas that lack access to cutting-edge cancer treatments and/or state-of-the-art health care facilities, sexual and gender minorities who experience bias and discrimination in health care settings, and low-income households where there is persistent poverty, and limited access to healthy food or the needed health care. It should be noted that patients with intersectional identities often experience multilevel barriers to cancer care that adversely impact screening, diagnosis, treatment, and survivorship. As one example, recent data have shown that Black and AIAN populations living in rural areas experience greater poverty and lack of access to quality care, which expose them to greater risk of experiencing poor cancer outcomes (22)Zahnd WE, et al. (2021) Int J Environ Res Public Health, 18. [LINK NOT AVAILABLE].
Root causes of cancer disparities are multidimensional and multifactorial. Researchers have developed many models to understand and address health inequities. A key component of these models is the framework of social determinants of health (SDOH). According to NCI, SDOH are the social, economic, and physical conditions in the places where people are born and where they live, learn, work, play, and grow older that can affect their health, well-being, and quality of life (see Figure 2). It is increasingly evident that structural racism and systemic injustices are key adverse social factors, creating conditions that perpetuate health inequities, including cancer disparities, for racial or ethnic minorities and other medically underserved populations (23)Alnajar A, et al. (2023) JAMA Netw Open, 6: e234261. [LINK NOT AVAILABLE](24)Hoskins KF, et al. (2023) JAMA Oncol, 9: 536. [LINK NOT AVAILABLE](25)Zhang L, et al. (2023) JAMA Oncol, 9: 122. [LINK NOT AVAILABLE](26)Vince RA, Jr., et al. (2023) JAMA Netw Open, 6: e2250416. [LINK NOT AVAILABLE].
Considering that a significant proportion of the U.S. population is affected by cancer disparities, it is important that public health experts intensify efforts designed to improve the understanding and mitigation of these inequities. Only with new insights obtained through innovative and inclusive research, such as basic research using biospecimens from diverse populations, clinical studies involving participants from all sociodemographic backgrounds, and health care delivery research that is representative of everyone in the communities, will we be able to develop and implement interventions that eventually eliminate cancers for all populations.
Variable Progress Against Different Types of Cancer and Stages of Diagnosis
Among the current challenges in cancer science and medicine is the uneven progress against different cancer types and different stages of a given cancer type.
These challenges are illustrated by the fact that the 5-year relative survival rates for U.S. patients vary widely depending on both the type of cancer diagnosed and the stage at diagnosis (5)Surveillance, Epidemiology, and End Results (SEER) Program. Accessed: July 5, 2023. . For example, the overall 5-year relative survival rates of 94 percent for patients with melanoma and 97 percent for patients with prostate cancer stand in stark contrast to the overall 5-year relative survival rates of 23 percent for those with liver cancer and 13 percent for those with pancreatic cancer. In addition, among women with breast cancer and men with prostate cancer, those whose cancer is confined to the breast, or to the prostate, have 5-year relative survival rates of 99 percent and 100 percent, respectively, while those whose cancer has metastasized have 5-year relative survival rates of 31 percent and 34 percent, respectively (5)Surveillance, Epidemiology, and End Results (SEER) Program. Accessed: July 5, 2023. .
Variable progress among different cancer types can be partly attributed to the availability of novel cutting-edge therapeutic options, or lack thereof, that have moved rapidly from the laboratory to the clinic and are now available to patients. As one example, between January 1, 2011, and July 31, 2023, the U.S. Food and Drug Administration (FDA) approved five immunotherapeutics and six molecularly targeted therapeutics for use alone or in combination for the treatment of patients with metastatic melanoma, a previously intractable cancer. Thanks to these innovative new therapeutics, melanoma mortality rates have declined rapidly between 2011 and 2020 by about five percent per year in adults younger than age 50 and three percent per year in those 50 and older (28)American Cancer Society. Cancer Facts and Figures. Accessed: July 5, 2023. . In contrast, progress has been slow for patients with glioblastoma multiforme (GBM), an aggressive form of brain tumor (see Tackling Difficult-to-Treat Cancers). Since the approval of the chemotherapeutic temozolomide nearly 25 years ago, no new anticancer agents have shown promise in improving overall survival. Consequently, the 5-year relative survival rate for patients with GBM remains at a dismal seven percent (29)Ostrom QT, et al. (2022) Neuro Oncol, 24: v1. [LINK NOT AVAILABLE].
Developing new and effective methods for early detection of more cancer types could help address the challenge of variable progress between types of cancer because the likelihood of cure is much higher when cancer is diagnosed at an early stage while it is confined to its original location than when it has spread to distant sites. Additionally, intensive research into the molecular underpinnings of cancer initiation and progression is vital in order to improve future therapeutic options for currently hard-to-treat diseases (see Tackling Difficult-to-Treat Cancers).
The Growing Population Burden of Cancer
The public health challenges posed by cancer are predicted to grow considerably in the coming decades unless we develop and implement more effective strategies for cancer prevention, early detection, and treatment (30)International Agency for Research on Cancer. Global Cancer Observatory. Accessed: July 31, 2023. . In the United States alone, the number of new cancer cases diagnosed each year is expected to reach nearly 2.3 million by 2040 (30)International Agency for Research on Cancer. Global Cancer Observatory. Accessed: July 31, 2023. . This is because cancer is primarily a disease of aging; 57 percent of diagnoses occur among those 65 and older (28)American Cancer Society. Cancer Facts and Figures. Accessed: July 5, 2023. , and this segment of the U.S. population is expected to grow from 54.1 million in 2019 to nearly 81 million in 2040 (31)U.S. Department of Health and Human Services. Administration for Community Living. 2020 Profile of Older Americans. Accessed: Jul 6, 2023. .
Also contributing to the projected increase in the number of U.S. cancer cases are the high rates of obesity and physical inactivity and the continued use of cigarettes by 11.5 percent of adults (32)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. [LINK NOT AVAILABLE]. However, it should be noted that a significant proportion of lung cancers (16 percent in women and 10 percent in men) are diagnosed in individuals without a history of smoking (33)Siegel DA, et al. (2021) JAMA Oncol, 7: 302. [LINK NOT AVAILABLE] and there is a need for more research to determine whether the incidence rate of lung cancer among those without a history of smoking is increasing (34)Pelosof L, et al. (2017) J Natl Cancer Inst, 109. [LINK NOT AVAILABLE]. Identification of risk factors, characterization of disease, and development of evidence-based early detection and treatments are critical needs to lower the burden of lung cancer in the population of patients who do not have a history of smoking.
While overall cancer incidence in the United States has stabilized in recent years, the incidence of certain cancer types such as pancreatic cancer and uterine cancer (5)Surveillance, Epidemiology, and End Results (SEER) Program. Accessed: July 5, 2023. is steadily increasing. Additionally, many recent studies have reported an increase in the incidence of colorectal cancer among individuals younger than 50 years, a phenomenon referred to as early-onset cancer (35)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 233. [LINK NOT AVAILABLE](36)Giannakis M, et al. (2023) Science, 379: 1088. [LINK NOT AVAILABLE]. According to a recent report, between 2011 and 2019, the colorectal cancer incidence rate increased by 1.9 percent per year in people younger than 50 years (35)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 233. [LINK NOT AVAILABLE]. Many of the early-onset colorectal cancer cases are diagnosed at an advanced stage. Between 2010 and 2019, among 20- to 49-year- old individuals, incidence of advanced-stage colorectal cancer increased by about three percent per year (35)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 233. [LINK NOT AVAILABLE].
Understanding the reasons behind rising cases of early-onset colorectal cancer is an area of intensive research. To reduce the burden of early-onset colorectal cancer, the United States Preventive Services Taskforce (USPSTF) and many professional societies have modified their screening guidelines to recommend starting colorectal cancer screening at an earlier age (see Guidelines for Cancer Screening). Researchers are also evaluating new and improved strategies including genetic testing and other approaches for prevention and early detection of colorectal cancer in the younger population (37)Sinicrope FA (2022) N Engl J Med, 386: 1547. [LINK NOT AVAILABLE].
Another cancer for which U.S. incidence rate has been rising is cervical cancer (39)Francoeur AA, et al. (2022) Int J Gynecol Cancer. [LINK NOT AVAILABLE](40)Shahmoradi Z, et al. (2022) JAMA, 328: 2267. [LINK NOT AVAILABLE]. According to a recent analysis, the rate of advanced cervical cancer (that has spread to the bladder or rectum at diagnosis) increased by 1.3 percent per year from 2001 to 2018 (39)Francoeur AA, et al. (2022) Int J Gynecol Cancer. [LINK NOT AVAILABLE]. A second report showed that, among U.S. women ages 30 to 34 years, overall cervical cancer incidence increased by 2.5 percent per year between 2012 and 2019 (40)Shahmoradi Z, et al. (2022) JAMA, 328: 2267. [LINK NOT AVAILABLE]. Considering that nearly all cervical cancers are caused by infection with human papillomavirus (HPV) and that HPV vaccination (see Prevent and Eliminate Infection from Cancer-causing Pathogens) and cervical cancer screening are extremely effective in reducing the burden of the disease, these data emphasize the importance of public health measures to boost cervical cancer prevention and early detection in the United States (see Screening for Early Detection).
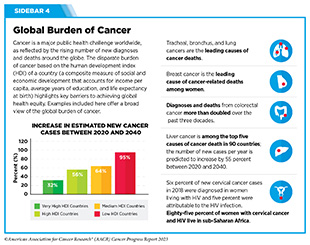
The Global Burden of Cancer
Beyond the United States, cancer is an ongoing global challenge (see Sidebar 4). According to a recent analysis, there were an estimated 17.2 million new cancer cases (excluding nonmelanoma skin cancer) and 10 million cancer deaths globally, in 2019 (41)Global Burden of Disease Cancer C, et al. (2022) JAMA Oncol, 8: 420. [LINK NOT AVAILABLE]. The study evaluated cancer burden in terms of cancer-related deaths, as well as disability-adjusted life years (DALYs) and years of life lost (YLLs), which are two measures of cancer morbidity. Researchers found that among the 22 groups of diseases and injuries analyzed, cancer was second only to cardiovascular disease in the number of deaths, DALYs, and YLLs (41)Global Burden of Disease Cancer C, et al. (2022) JAMA Oncol, 8: 420. [LINK NOT AVAILABLE]. The five leading causes of cancer-related morbidity among men and women combined were cancers of the lung, colon and rectum, stomach, breast, and liver.
There is a stark disparity in the cancer burden among countries with different levels of socioeconomic development. Researchers use various metrics such as human development index (HDI) or sociodemographic index (SDI), which are composite measures of social and economic development, to identify where countries or geographic areas fall on the spectrum of development. SDI quantification considers income per capita, average years of education, and total fertility rate for citizens younger than 25 (42)Institute for Health Metrics and Evaluation. Socio-demographic Index (SDI). Accessed: July 5, 2023. ; HDI measurement considers income per capita, average years of education, and life expectancy at birth (43)United Nations. Human Development Index. Accessed: July 5, 2023. . While age-adjusted cancer incidence and mortality rates are declining in countries with high SDI, both rates are still trending upward in lower SDI countries (41)Global Burden of Disease Cancer C, et al. (2022) JAMA Oncol, 8: 420. [LINK NOT AVAILABLE]. Based on a recent estimate, between 2010 and 2019, countries with the lowest SDI experienced the largest percent increase in the numbers of cancer cases and deaths (41)Global Burden of Disease Cancer C, et al. (2022) JAMA Oncol, 8: 420. [LINK NOT AVAILABLE].
Considering the growth and aging of the global population and the negative impact of recent global crises such as the COVID-19 pandemic on cancer research and patient care (45)United Nations. Ageing. Accessed: July 6, 2023. , researchers caution that the burden of cancer worldwide may rise significantly in the coming decades. One area in which progress is urgently needed is the establishment of population-based cancer registries in all countries because the collection of high-quality cancer surveillance data is essential for developing effective national cancer control plans. Notably, only one in five low- and middle-income countries has the necessary data to drive policy and reduce the burden and suffering due to cancer, according to the International Agency for Research on Cancer (46)Editorial (2014) Lancet, 383: 1946. [LINK NOT AVAILABLE].
Another emerging concern among public health experts is the dramatic rise since the 1990s in the incidence of early-onset cancers, including cancers of the breast, colon, esophagus, kidney, liver, and pancreas, among others, around the world (47)Ugai T, et al. (2022) Nat Rev Clin Oncol, 19: 656. [LINK NOT AVAILABLE]. While improvements in early detection may be attributable, in part, to this rising cancer incidence, researchers hypothesize that early life exposures to certain cancer risk factors (see Reducing the Risk of Cancer Development), including diets rich in highly processed foods, alcohol, sedentary lifestyle, obesity, environmental carcinogens, and an unfavorable microbiome, many of which have become more prevalent in recent decades, are playing a role in the increased incidence of early-onset cancers (47)Ugai T, et al. (2022) Nat Rev Clin Oncol, 19: 656. [LINK NOT AVAILABLE]. Notably, 44 percent of cancer deaths worldwide are caused by modifiable risk factors, such as smoking and drinking alcohol (48)GBD 2019 Cancer Risk Factors Collaborators. (2022) Lancet, 400:563 [LINK NOT AVAILABLE].
To ensure equitable progress against cancer worldwide, it is imperative that the global medical research community work together and shares best practices to implement newer and more effective strategies that incorporate local needs and knowledge into tailored national cancer control plans. Public health experts have identified several priorities based on present and future needs of low resource countries, including reducing the burden of advanced cancers; improving access, affordability, and outcomes of treatment; utilizing value-based care; fostering implementation research; and leveraging technology to improve cancer control (49)Pramesh CS, et al. (2022) Nat Med, 28: 649. [LINK NOT AVAILABLE]. The urgent need for robust worldwide investments in medical research is emphasized by recent findings that estimated the cumulative global economic burden of cancer to be at an enormous $25.2 trillion over the next 30 years (50)Chen S, et al. (2023) JAMA Oncol, 9: 465. [LINK NOT AVAILABLE].
Funding Cancer Research: A Vital Investment
Cancer exerts an immense toll, both because of the number of lives it affects each year and its significant economic impact. The direct medical costs of cancer care are one measure of the financial impact of cancer, and in the United States alone, these costs were estimated to be nearly $209 billion in 2020, the last year for which these data are currently available (28)American Cancer Society. Cancer Facts and Figures. Accessed: July 5, 2023. . Unfortunately, these numbers stand in stark contrast to the NCI budget of $6 billion for the same year. Notably, the direct medical costs do not include the indirect costs of lost productivity due to cancer-related morbidity and mortality, which are also extremely high. As one example, the costs of lost productivity for U.S. adolescent and young adult patients with cancer (age 15 to 39) diagnosed in 2019 were an estimated $18 billion over their lifetime (54)Parsons SK, et al. (2023) J Clin Oncol, 41: 3260. [LINK NOT AVAILABLE].
Patients with cancer shoulder a large amount of economic burden associated with cancer care. In 2019, in the United States, patients with cancer lost nearly $5 billion due to time costs— value of time that patients spend traveling to and from health care, waiting for care, and receiving care—and paid an estimated $16.2 billion in out-of-pocket costs for cancer care (55)Kuehn BM (2021) JAMA, 326: 2251. [LINK NOT AVAILABLE].
With the number of cancer cases projected to increase in the coming decades, it is likely that both the direct and indirect costs will also escalate. According to a recent report the economic burden of cancer in the United States will reach $5.3 trillion over the next three decades (50)Chen S, et al. (2023) JAMA Oncol, 9: 465. [LINK NOT AVAILABLE]. The rising personal and economic burden of cancer underscores the urgent need for more research so that we can accelerate the pace of progress and curb the increasing burden of this disease.
Recent advances in cancer prevention, detection, and treatment, many of which are highlighted in this report, were made as a direct result of the cumulative efforts of researchers across the spectrum of cancer science and medicine. Much of their work, as well as that of FDA and CDC, is supported by funds from the federal government. Public sector funding from NIH and NCI contributes significantly to the development of novel anticancer drugs including molecularly targeted therapeutics and immunotherapeutics (see Advances in Treatment with Molecularly Targeted Therapy) and Immunotherapy: Pushing the Frontier of Cancer Medicine) (56)Nayak RK, et al. (2021) JAMA Intern Med, 181: 1522. [LINK NOT AVAILABLE](57)Galkina Cleary E, et al. (2023) JAMA Health Forum, 4: e230511. [LINK NOT AVAILABLE]. The rapid pace of approval of these cutting-edge treatments, many of which were evaluated in NCI-funded clinical trials, has transformed the treatment landscape and dramatically improved patient outcomes. A recent study that evaluated the population-level impact of NCI-funded clinical research concluded that over the past 40 years, patients with cancer in the United States gained 14 million years of additional life because of these trials (60)Shiels MS, et al. (2023) Cancer Discov, 13: 1084. [LINK NOT AVAILABLE]. Collectively, these findings highlight the importance of federal investments in medical research in saving and extending lives and driving progress against cancer.
The consecutive increases for the NIH budget in the last seven fiscal years have helped maintain the momentum of progress against cancer and other diseases (see Investments in Research Fuel a Healthier Future). Additionally, NIH research grants help sustain the U.S. economy. In Fiscal Year (FY) 2022, the $36.68 billion awarded to researchers in the 50 U.S. states and the District of Columbia supported more than 568,000 jobs and nearly $97 billion in economic activity (59)United for Medical Research. NIH’s Role in Sustaining the U.S. Economy. Accessed: August 1, 2023. .
NCI’s current success rate of 14.1 percent in FY 2021 has created a grant funding crisis and has left potentially lifesaving cancer science and medicine unfunded. There are also serious concerns that early-stage scientists and those from underrepresented racial or ethnic backgrounds might choose other career paths instead of academic research, which will impede progress against cancer.
If Congress lowers the NCI budget, it will force the Institute to reduce pay lines to even lower levels. Such actions will result in highly meritorious grants being unfunded and make it harder for the next generation of scientists to build promising careers in cancer research.
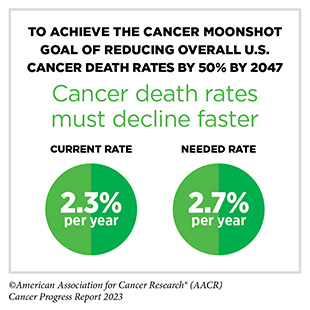
Therefore, it is imperative that in the years ahead, Congress continues to provide sustained, robust, and predictable increases in investments in the federal agencies that are vital for fueling progress against cancer, in particular, NIH, NCI, FDA, and CDC (see AACR Call to Action). Such investments will help the medical research community sustain the momentum of scientific and technological innovation and accelerate the pace of progress against cancer to achieve the President’s Cancer Moonshot goal of reducing U.S. cancer death rate by 50 percent by the year 2047.
Next Section: Understanding the Path to Cancer Development Previous Section: A Snapshot of a Year in Progress