- Eliminate Tobacco Use
- Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active
- Reduce Alcohol Consumption
- Protect Skin from UV Exposure
- Prevent and Eliminate Infection from Cancer-causing Pathogens
- Limit Exposure to Environmental Risk Factors
- Be Cognizant of Hormonal Factors
- Spotlight: Increasing Cancer Risk Among Children and AYAs
Reducing the Risk of Cancer Development
In this section, you will learn:
- In the United States, 40 percent of all cancers are associated with modifiable risk factors, which necessitates a robust emphasis on and support for public health–focused research.
- The significant decline in cancer mortality over the past three decades is, in part, attributable to reductions in smoking following the implementation of public health campaigns and policy initiatives.
- Nearly 20 percent of US cancer diagnoses are related to excess body weight, unhealthy dietary patterns, alcohol intake, and physical inactivity.
- Vaccination against human papillomavirus (HPV) nearly eliminates the risk of cervical cancer, vulvar cancers, and penile or anus cancers caused by HPV.
- Exposure to high levels of chemicals in the environment, including air pollution, radon, endocrine-disrupting chemicals, and industrial chemicals, can increase an individual’s risk of certain types of cancers. Workers who are exposed to carcinogens and those who participate in night-shift work are also at an elevated risk of developing certain types of cancers.
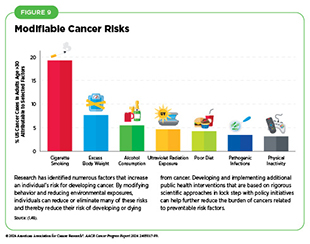
Research in basic, translational, and population sciences has broadened our understanding of the factors that increase an individual’s risk of developing cancer (see Figure 9). Modifiable risk factors, including tobacco use, unhealthy diet, physical inactivity, ultraviolet (UV) exposure, excessive alcohol consumption, pathogenic infections, and obesity, contribute to the development of 40 percent of all cancers (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. Given that several of these risks can be avoided or reduced, many cases of cancer can potentially be prevented.
In the United States, the age-adjusted overall cancer death rate declined by 33 percent between 1991 and 2021. This reduction is attributable in part to public health interventions as well as policy initiatives that reduced smoking and removed barriers to cancer screening, such as by reducing or eliminating co-payments for mammograms (4)Siegel RL, et al. (2024) CA Cancer J Clin, 74: 12. DOI: 10.3322/caac.21820.(172)Richman IB, et al. (2023) JAMA Netw Open, 6: e234898. DOI: 10.1001/jamanetworkopen.2023.4898.. However, while smoking rates have declined significantly, the increasing prevalence of other risk factors, including obesity among US children and adults, is a cause for public health concern. Additionally, there is a lack of widespread utilization in the United States of preventive interventions such as vaccination against cancer-causing viruses including human papillomavirus (HPV), which is the primary cause of cervical cancer.
Air pollution, water contamination, carcinogenic chemicals in consumable goods (e.g., cars and furniture), endocrine-disrupting chemicals, and naturally occurring radon gas increase a person’s risk for certain types of cancer, including common cancers such as lung cancer. While most individuals are exposed to these pollutants to some extent, some populations, such as those who live in low-income communities and rural areas, or on tribal lands, may be exposed to higher levels (30)American Lung Association. State of the Air 2023 Report. Accessed: March 17, 2024.(173)Bradley AC, et al. (2024) Environ Sci Technol, 58: 4226. DOI: 10.1021/acs.est.3c03230.(174)Tessum CW, et al. (2021) Sci Adv, 7: eabf4491. DOI: 10.1126/sciadv.abf4491.(175)Carroll R, et al. (2023) Environ Res, 239: 117349. DOI: 10.1016/j.envres.2023.117349.(176)Cheng I, et al. (2022) Am J Respir Crit Care Med, 206: 1008. DOI: 10.1164/rccm.202107-1770OC.(177)Yazzie SA, et al. (2020) Int J Environ Res Public Health, 17: 2813. DOI: 10.3390/ijerph17082813.. Occupational exposures—any type of physical, chemical, or biological agents encountered in a person’s employment that would increase the risk of injury or disease—such as to hazardous materials encountered during firefighting, silica dust in mines, and noxious fumes in fabrication and roofing can also increase a person’s risk for developing cancer.
Emerging data indicate that certain cancer risk factors are also associated with worse outcomes after a cancer diagnosis, including development of secondary cancers. In addition, cancer risk factors contribute to other chronic diseases, such as cardiovascular and respiratory diseases and diabetes. Increased recognition of these modifiable risk factors can help local and national public health organizations enhance prevention efforts and lessen the negative health and economic impact of these diseases, including cancer.
Eliminate Tobacco Use
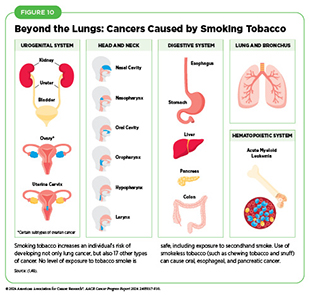
The use of tobacco products is the leading preventable cause of cancer and is associated with the development of 17 different types of cancer in addition to lung cancer (see Figure 10). Nearly 20 percent of all cancer cases and almost 30 percent of all cancer-related deaths are caused by smoking cigarettes (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. In the United States, between 80 percent and 90 percent of lung cancer deaths are attributable to smoking (178)Warren GW, et al. (2013) Am Soc Clin Oncol Educ Book, 33: 359. DOI: 10.14694/EdBook_AM.2013.33.359.. On average, people who smoke die 10 years younger than those who have never smoked (179)Jha P, et al. (2013) N Engl J Med, 368: 341. DOI: 10.1056/NEJMsa1211128..
Research over the past 50 years has consistently demonstrated that byproducts released from smoking tobacco products, such as cigarettes, cause permanent cellular and molecular alterations, which lead to cancer (180)Alexandrov LB, et al. (2016) Science, 354: 618. DOI: 10.1126/science.aag0299.(181)Pezzuto A, et al. (2019) Future Sci OA, 5: FSO394. DOI: 10.2144/fsoa-2019-0017.(182)Yang Y, et al. (2023) J Hazard Mater, 455: 131556. DOI: 10.1016/j.jhazmat.2023.131556.. Furthermore, smoking causes many other chronic conditions, including chronic obstructive pulmonary disease (COPD), asthma, and many types of cardiovascular diseases, particularly coronary artery disease.
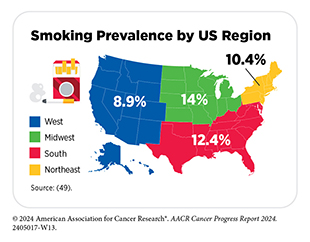
Thanks to nationwide tobacco control initiatives, cigarette smoking among US adults has been declining. In fact, cigarette smoking rates among US adults have decreased from 42.4 percent in 1965 to 11.5 percent in 2021 (49)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. DOI: 10.15585/mmwr.mm7218a1.. However, even in 2021, the most recent year for which such data are available, an estimated 46 million US adults reported using any tobacco product (e.g., cigarettes, cigars, pipes) (49)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. DOI: 10.15585/mmwr.mm7218a1.. In the United States there are geographical differences in smoking rates, which has led to certain regions with high smoking prevalence being associated with higher rates of lung cancer mortality (183)Shreves AH, et al. (2023) Cancer Epidemiol Biomarkers Prev, 32: 193..
There are striking sociodemographic disparities in the use of tobacco products as well as in exposure to secondhand smoke, also a cancer risk factor, as highlighted in the AACR Cancer Disparities Progress Report 2024. Overall tobacco use is higher among US residents who live in rural areas and in the Midwest, those with lower levels of household income and educational attainment, those who are uninsured or insured by Medicaid, those experiencing psychological distress, and those who have a disability (49)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. DOI: 10.15585/mmwr.mm7218a1.(184)Loretan CG, et al. (2022) Prev Chronic Dis, 19: E87. DOI: 10.5888/pcd19.220184.. Furthermore, US adults who identify as belonging to the sexual and gender minority (SGM) population have higher rates of using tobacco products.
Similar to the trend in adults, tobacco use among US youth such as middle and high school students is also declining, with 6.6 percent of middle and 12.6 percent of high school students reporting current use of a tobacco product in 2023 (185). The number of high school students with current use of any tobacco product declined from 2.51 million in 2022 to 1.97 million in 2023, representing 540,000 fewer high school students using tobacco products (185)Birdsey J, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 1173. DOI: 10.15585/mmwr.mm7244a1.. Specifically, the proportion of middle and high school students who have ever used a cigarette in 2023 was 4.3 and 8.5 percent, respectively, equating to 510,000 middle and 1.3 million high school students (185)Birdsey J, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 1173. DOI: 10.15585/mmwr.mm7244a1..
Flavored tobacco products, such as menthol cigarettes, pose a significant health risk, at least partly because they lead to increased nicotine dependence and reduced smoking cessation compared to nonmenthol cigarettes (186)Villanti AC, et al. (2021) Nicotine Tob Res, 23: 1318. DOI: 10.1093/ntr/ntaa224.(187)Watkins SL, et al. (2022) J Adolesc Health, 71: 226. DOI: 10.1016/j.jadohealth.2022.02.013.. Overall, 38.8 percent of Americans who smoke use menthol cigarettes and their use is more common in Black individuals (188)Villanti AC, et al. (2016) Tob Control, 25: ii14. DOI: 10.1136/tobaccocontrol-2016-053329.. Evidence shows that young adults are more likely to try menthol cigarettes and are more likely to continue smoking into adulthood compared to young adults who try nonmenthol cigarettes (186)Villanti AC, et al. (2021) Nicotine Tob Res, 23: 1318. DOI: 10.1093/ntr/ntaa224.. In addition, 40.4 percent of middle and high school students who smoke report using menthol cigarettes (185)Birdsey J, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 1173. DOI: 10.15585/mmwr.mm7244a1.. This is greater than the percentage of adults who smoke menthol cigarettes.
There is strong evidence that smoking cessation has both immediate and long-term health benefits, especially when stopping at a younger age. Those who stop smoking reduce their risk of developing cancers of the larynx, oral cavity, and pharynx by half after 10 years of cessation (189)Ahmed AA, et al. (2015) Circ Heart Fail, 8: 694. DOI: 10.1161/CIRCHEARTFAILURE.114.001885.(190)Duncan MS, et al. (2019) JAMA, 322: 642. DOI: 10.1001/jama.2019.10298.. After 20 years, the risk of developing these cancers is lowered to the same level as someone who never smoked (189)Ahmed AA, et al. (2015) Circ Heart Fail, 8: 694. DOI: 10.1161/CIRCHEARTFAILURE.114.001885.(190)Duncan MS, et al. (2019) JAMA, 322: 642. DOI: 10.1001/jama.2019.10298.. Evidence from a large study demonstrated that, among individuals who stopped smoking before age 45, all-cause mortality was similar to that of a person who never smoked (191)Thomson B, et al. (2022) JAMA Netw Open, 5: e2231480. DOI: 10.1001/jamanetworkopen.2022.31480..
Evidence-based interventions at local, state, and federal levels, including tobacco price increases, public health interventions, marketing restrictions and bans on menthol cigarettes, subsidized smoking cessation counseling (such as through insurance), FDA-approved medications, and smoke-free laws, must be utilized to continue the downward trend of tobacco use (192)Fu SS, et al. (2023) JAMA Netw Open, 6: e2329903. DOI: 10.1001/jamanetworkopen.2023.29903..
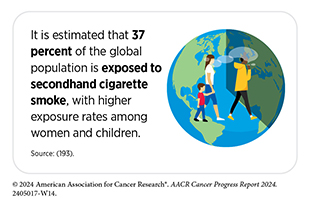
Exposure to secondhand smoke, which occurs when people inhale smoke exhaled by people who smoke or from burning tobacco products, can cause cancer. Furthermore, exposure to secondhand smoke increases the risk of heart disease (8 percent), stroke (5 percent), and type 2 diabetes (1 percent) (193). Encouragingly, secondhand smoke exposure has declined in the United States from 27.7 percent between 2009 and 2010 to 20.7 percent between 2017 and 2018 (194)Brody D, et al. (2021) MMWR Morb Mortal Wkly Rep, 70: 224. DOI: 10.15585/mmwr.mm7006a6., the most recent time for which such data were available. Despite this decline, secondhand smoke is estimated to cause 41,000 deaths each year among adults in the United States, with 7,300 deaths attributed to lung cancer (195)US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress A Report of the Surgeon General. Accessed: March 17, 2024.. Enacting smoke-free laws that prohibit smoking in public places, such as in parks, restaurants, and public transit, can eliminate the risk of secondhand smoke and are essential to reduce the negative health effects on those who do not smoke.
Electronic cigarettes, commonly known as e-cigarettes, were first introduced in the United States in 2006, and have gained popularity among those who have never used tobacco products. Since 2014, e-cigarettes have been the most used tobacco product among middle and high school students (196)Centers for Disease Control and Prevention. Youth and Tobacco Use | Smoking and Tobacco Use. Accessed:. In 2023, 10 percent of middle and high school students used e-cigarettes, with 25 percent of users reporting daily use of e-cigarettes (185)Birdsey J, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 1173. DOI: 10.15585/mmwr.mm7244a1.. Of middle and high school students who used e-cigarettes daily, nearly nine out of 10 reported using flavored e-cigarette products (185)Birdsey J, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 1173. DOI: 10.15585/mmwr.mm7244a1.. The primary drivers of use among adolescents were peer pressure and living with a person who uses tobacco (197)Le TTT (2023) JAMA Netw Open, 6: e2337101. DOI: 10.1001/jamanetworkopen.2023.37101.. E-cigarettes are also popular among those who want to stop smoking; however, the benefits of e-cigarettes for smoking cessation are not as well established (198)Auer R, et al. (2024) N Engl J Med, 390: 601. DOI: 10.1056/NEJMoa2308815.. More rigorous research evaluating the benefits of e-cigarettes in smoking cessation using randomized clinical trials is needed.
The landscape of e-cigarette devices has evolved over the years to include different types of products, such as prefilled pods (e.g., JUUL) or cartridge-based and disposable devices (e.g., Puff Bar), among others. E-cigarettes can deliver nicotine, a highly addictive substance that is harmful to the developing brain, much faster than traditional tobacco products (199)Prochaska JJ, et al. (2022) Tob Control, 31: e88. DOI: 10.1136/tobaccocontrol-2020-056367..
Recent estimates show that e-cigarette usage was highest among individuals ages 18 to 24 years, with 18.6 percent reporting current use; among these, 71.5 percent of individuals ages 18 to 20 years had never smoked combustible cigarettes (200)Erhabor J, et al. (2023) JAMA Netw Open, 6: e2340859. DOI: 10.1001/jamanetworkopen.2023.40859..
While e-cigarettes emit fewer carcinogens than combustible tobacco, they still expose individuals to many toxic chemicals, including metals that can damage DNA and trigger inflammation (201)Goniewicz ML, et al. (2018) JAMA Netw Open, 1: e185937. DOI: 10.1001/jamanetworkopen.2018.5937.(202)Herbst RS, et al. (2022) Clin Cancer Res, 28: 4861.. Furthermore, people who use e-cigarettes are 3 to 4 times more likely to ever smoke a combustible cigarette than people who have never used e-cigarettes (202)Herbst RS, et al. (2022) Clin Cancer Res, 28: 4861.. Further research is warranted on e-cigarettes and their long-term health effects, especially in teens and young adults so that appropriate preventive interventions can be implemented.
Another area in which more research is needed is the health consequences of smoking marijuana. For example, there is concern among public health experts that it could cause cancer because it involves the burning of an organic material, much like smoking tobacco (203)Ghasemiesfe M, et al. (2019) JAMA Netw Open, 2: e1916318. DOI: 10.1001/jamanetworkopen.2019.16318.. The need for this research is driven by the growing number of states that have legalized marijuana use for medical and/or recreational purposes. Currently in the United States, 74 percent of Americans live in a state where marijuana is legal for either recreational or medical use (204)Pew Research Center. Most Americans Now Live in a Legal Marijuana State – and Most Have At Least One Dispensary in Their County. Accessed: March 26, 2024..
Use of cannabidiol (CBD), an active ingredient in marijuana, in e-cigarettes among US middle and high school students is particularly concerning, with 21.3 percent reporting use in the previous month (205)Dai HD, et al. (2023) JAMA Netw Open, 6: e2329167. DOI: 10.1001/jamanetworkopen.2023.29167.. CBD use in e-cigarettes, often referred to as vaping, is higher among Hispanic and SGM populations (205)Dai HD, et al. (2023) JAMA Netw Open, 6: e2329167. DOI: 10.1001/jamanetworkopen.2023.29167.. Although the cancer risk and other adverse health outcomes associated with vaping CBD are not well established, continued monitoring and research are needed.
Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active
More than 20 percent of new cancer cases and more than 17 percent of cancer deaths in US adults are attributable to a combination of excess body weight, poor diet, physical inactivity, and alcohol consumption (see Figure 11) (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.(206)Islami F, et al. (2018) CA Cancer J Clin, 68: 31. DOI: 10.3322/caac.21440.(207)Islami F, et al. (2019) JAMA Oncol, 5: 384. DOI: 10.1001/jamaoncol.2018.5639.. Following a healthier lifestyle may reduce the risk of developing certain cancers as well as many other adverse health outcomes.
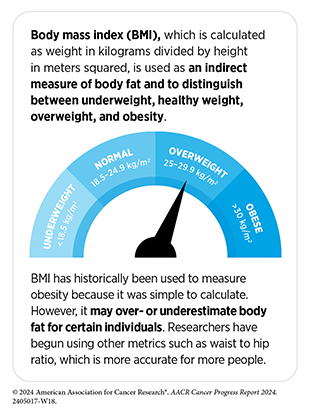
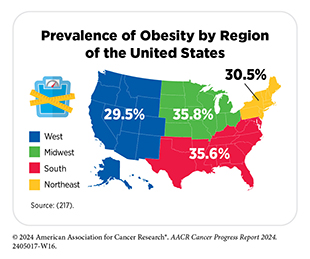
Excess body weight is responsible for 7.6 percent of all cancers (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. Among US adults, the rate of obesity during 2017 to 2020 was 41.9 percent (215)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: March 17, 2024.. This is a 37 percent increase from the year 2000, when the rate was 30.5 percent (215)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: March 17, 2024.. During this same time, severe obesity among US adults nearly doubled, with an increase from 4.7 percent to 9.2 percent (215)Centers for Disease Control and Prevention. Adult Obesity Facts. Accessed: March 17, 2024.. Globally, rates of obesity have doubled between 1990 and 2022, with 16 percent of adults over the age of 18 who were obese in 2022 (216)World Health Organization. Obesity and Overweight. Accessed: July 10, 2024.. As with smoking, adults who are obese have an increased risk of many chronic diseases, including diabetes, cardiovascular disease, stroke, and cancer (84)American Association for Cancer Research. AACR Cancer Progress Report 2022. Accessed: July 5, 2023..
Weight loss interventions have proven effective in reducing or eliminating the risk of cancers associated with obesity (219)Schauer DP, et al. (2017) Obesity (Silver Spring), 25 Suppl 2: S52. DOI: 10.1002/oby.22002.(220)Bruno DS, et al. (2020) Ann Transl Med, 8: S13. DOI: 10.21037/atm.2019.09.26.. Bariatric surgery is a collection of procedures that are done to help people who are obese lose weight when effectively paired with eating a healthy diet and regular exercise. Bariatric surgery has been shown to lower the risk of developing and/or dying from certain obesity-associated cancers (221)Adams TD, et al. (2023) Obesity (Silver Spring), 31: 574. DOI: 10.1002/oby.23646.(222)Aminian A, et al. (2022) JAMA, 327: 2423. DOI: 10.1001/jama.2022.9009..
Another type of weight loss strategy that has been on the rise is the use of weight loss drugs such as semaglutide (brand names Ozempic and Wegovy). These drugs, called GLP-1 receptor agonists, work by mimicking the hormone GLP-1, which controls the body’s insulin levels and leads to appetite suppression and feeling fuller for longer periods of time after eating. These drugs, in combination with eating a healthy diet and exercise, have led to dramatic weight loss for many individuals.
Although the effect of these drugs on weight loss are encouraging, more research is required to understand whether these medications can reduce the rates of obesity-associated cancers. In this regard, studies evaluating the long-term effects of GLP-1RA (a drug very similar to semaglutide) among diabetic patients demonstrate their potential to reduce the risk of cancer (223)Wang L, et al. (2024) JAMA Oncol, 10: 256. DOI: 10.1001/jamaoncol.2023.5573.. After 15 years of follow-up, researchers found that the risk of colorectal cancer in patients who were given the therapeutic decreased by half compared to patients who received other types of diabetic medication (e.g., insulin) (223)Wang L, et al. (2024) JAMA Oncol, 10: 256. DOI: 10.1001/jamaoncol.2023.5573.. While this research is promising, it is important to note that no long-term studies of these treatments have been done with non-diabetic patients. It will be important to continue monitoring the long-term effects of these weight loss medications in non-diabetic patients and their ability to reduce obesity-related cancers.
Poor diet, consisting of red meat and processed foods and lacking fresh fruits or vegetables, is responsible for the development of more than 4.2 percent of all cancers, with several studies demonstrating a link between consumption of highly processed foods and increased cancer incidence (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.(224)Morales-Berstein F, et al. (2024) Eur J Nutr, 63: 377. DOI: 10.1007/s00394-023-03270-1.(225)Jin Q, et al. (2023) Br J Cancer, 129: 1978. DOI: 10.1038/s41416-023-02469-7.(226)Chang K, et al. (2023) EClinicalMedicine, 56: 101840. DOI: 10.1016/j.eclinm.2023.101840..
The widespread availability and low cost of fast food—food that can be prepared quickly and easily and that is sold in restaurants and snack bars as a quick meal or to be taken out— led to 37 percent of US adults (ages 40 to 59) and 45 percent of US young adults (ages 20 to 39) consuming fast food on any given day during 2013–2016 (227)Centers for Disease Control and Prevention. Fast Food Consumption Among Adults in the United States, 2013–2016. Accessed: July 5, 2023.. Unfortunately, fast foods are often of poor nutritional value, calorie dense, high in salt content, and low in fiber (228)Meine GC, et al. (2024) Am J Gastroenterol, 119: 1056. DOI: 10.14309/ajg.0000000000002826.(229)Caceres-Matos R, et al. (2024) Gastrointest Disord, 6: 164. DOI: 10.3390/gidisord6010012(230)Visioli F, et al. (2024) Lancet Reg Health Eur, 38: 100863. DOI: 10.1016/j.lanepe.2024.100863..
Intake of red meat specifically should be limited to no more than three servings a week (12 to 18 ounces a week) and should not include processed meats (e.g., hot dogs, bacon, and salami), because these foods can increase the risk of colorectal, rectal, and potentially other cancers including prostate and pancreatic cancer (228)Meine GC, et al. (2024) Am J Gastroenterol, 119: 1056. DOI: 10.14309/ajg.0000000000002826.(229)Caceres-Matos R, et al. (2024) Gastrointest Disord, 6: 164. DOI: 10.3390/gidisord6010012(230)Visioli F, et al. (2024) Lancet Reg Health Eur, 38: 100863. DOI: 10.1016/j.lanepe.2024.100863.(231)Sivasubramanian BP, et al. (2023) Cureus, 15: e45324. DOI: 10.7759/cureus.45324.(232)Di Y, et al. (2023) BMC Cancer, 23: 782. DOI: 10.1186/s12885-023-11218-1.(233)Kim Y (2023) Cancer Causes Control, 34: 569. DOI: 10.1007/s10552-023-01698-8.. Sugar-sweetened beverages, which include any drink that contains added sugars, such as soda, fruit and sports drinks, and energy drinks, or coffee and tea with added sugars, have also been associated with increasing the risk of several cancers including liver and colon cancers, as well as other chronic diseases including diabetes and kidney disease (234)Zhao L, et al. (2023) JAMA, 330: 537. DOI: 10.1001/jama.2023.12618.(235)Feng L, et al. (2023) Eur J Clin Nutr, 77: 941. DOI: 10.1038/s41430-023-01302-x.(236)de Lorgeril M, et al. (2020) Transl Cancer Res, 9: 3172. DOI: 10.21037/tcr-2020-003.(237)McCullough ML, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 1907.(238)Tseng TS, et al. (2021) World J Diabetes, 12: 1530. DOI: 10.4239/wjd.v12.i9.1530.(239)Heo GY, et al. (2024) JAMA Netw Open, 7: e2356885. DOI: 10.1001/jamanetworkopen.2023.56885.(240)Cai XY, et al. (2022) Clin Kidney J, 15: 718. DOI: 10.1093/ckj/sfab227.. High fructose corn syrup, a common ingredient used as a sweetener in many processed foods and beverages, has also been found to promote intestinal tumor growth in experimental models, although more research, including epidemiological data in humans, is warranted (241)Goncalves MD, et al. (2019) Science, 363: 1345. DOI: 10.1126/science.aat8515..
One strategy to lower consumption of foods high in sugar is to implement taxes on sugar-sweetened beverages, such as those introduced in several cities in the United States. In cities with such taxes, significant reductions were made in the consumption of sugar-sweetened beverages compared to cities that did not implement these types of taxes (242)Hua SV, et al. (2023) JAMA Netw Open, 6: e2323200. DOI: 10.1001/jamanetworkopen.2023.23200.(243)Kaplan S, et al. (2024) JAMA Health Forum, 5: e234737. DOI: 10.1001/jamahealthforum.2023.4737.(244)Bleich SN, et al. (2021) JAMA Netw Open, 4: e2113527. DOI: 10.1001/jamanetworkopen.2021.13527.. As of 2022, eight US jurisdictions and more than 50 countries have implemented some type of tax on sugar-sweetened beverages (243)Kaplan S, et al. (2024) JAMA Health Forum, 5: e234737. DOI: 10.1001/jamahealthforum.2023.4737.. Pilot initiatives such as these are a step in the right direction and continuous evaluation will further determine their long-term health benefits and impact on diet, obesity, and cancer burden.
Consumption of a diet rich in fresh fruits and vegetables, nuts, whole grains, and fish can help lower the risk of developing certain cancers and many other chronic conditions (245)Bui LP, et al. (2024) Am J Clin Nutr, 120: 80. DOI: 10.1016/j.ajcnut.2024.03.019.(246)Cai Y, et al. (2024) Am J Clin Nutr, 119: 406. DOI: 10.1016/j.ajcnut.2023.11.015. (see Sidebar 10). One study of nearly 80,000 men from diverse backgrounds found that adherence to a healthy diet lowered risk for certain types of colorectal cancers (247)Hang D, et al. (2023) J Natl Cancer Inst, 115: 155. DOI: 10.1093/jnci/djac221.. Increasing access to healthy foods such as by eliminating food deserts, which are geographical areas with a low density of grocery stores; promoting the benefits of healthy foods in decreasing the risk of cancer and other chronic diseases through public education campaigns and initiatives; and reducing government subsidies for crops like corn and soybeans, which are used to make inexpensive sugars, including corn syrup, that are used in highly processed foods in favor of subsidies for whole foods like fruits and vegetables are imperative to improve Americans’ diets and reduce the risk and incidence of cancer and other chronic diseases.
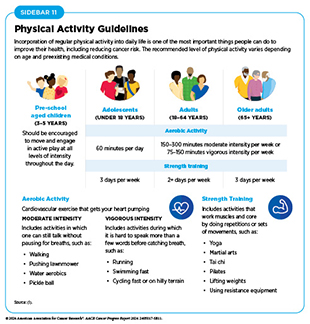
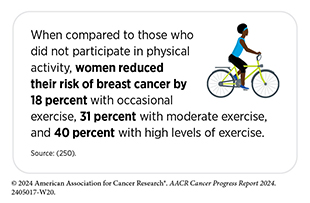
Engaging in regular physical activity at the levels recommended by the Centers for Disease Control and Prevention (CDC) can reduce the risk of nine different types of cancer, with research indicating that over 46,000 US cancer cases annually could potentially be avoided if everyone met the recommended CDC guidelines for physical activity (see Sidebar 11) (248)Lopez-Bueno R, et al. (2023) JAMA Intern Med, 183: 982. DOI: 10.1001/jamainternmed.2023.3093.(249)Minihan AK, et al. (2022) Med Sci Sports Exerc, 54: 417. DOI: 10.1249/MSS.0000000000002801.. One study found that among 500,000 people who participated in a balanced combination of moderate and vigorous aerobic and muscle strengthening exercises, there was a 50 percent lower rate of all-cause and cancer-specific mortality (248)Lopez-Bueno R, et al. (2023) JAMA Intern Med, 183: 982. DOI: 10.1001/jamainternmed.2023.3093..
There are many barriers that may prevent individuals from being physically active, including cost and access to fitness facilities, low neighborhood walkability, lack of green spaces, inadequate tree canopy cover, and family obligations (251)Withall J, et al. (2011) BMC Public Health, 11: 507. DOI: 10.1186/1471-2458-11-507.(252)Patel NA, et al. (2022) Kans J Med, 15: 267. DOI: 10.17161/kjm.vol15.17592.(253)Engelberg JK, et al. (2016) BMC Public Health, 16: 395. DOI: 10.1186/s12889-016-3055-4.(254)Thornton CM, et al. (2016) SSM Popul Health, 2: 206. DOI: 10.1016/j.ssmph.2016.03.004.. These barriers are exacerbated in racial and ethnic minority individuals and medically underserved populations. Based on recent data, physical inactivity is higher among Hispanic (31.7 percent) and non-Hispanic (NH) Black (30.3 percent) populations, compared to those who are NH White (23.4 percent) (255)Centers for Disease Control and Prevention. Physical Inactivity is More Common among Racial and Ethnic Minorities in Most States. Accessed: July 5, 2023.. There are also geographic disparities, with only 16 percent of people in suburban and rural areas meeting the recommended physical activity guidelines, compared to 27.8 percent of those living in urban areas (256)Abildso CG, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 85. DOI: 10.15585/mmwr.mm7204a1..
A sedentary lifestyle can increase the risk of certain cancers. As one example, researchers found that a person’s risk of pancreatic cancer was increased in a proportionate manner for every hour spent watching television, which was used as a measure of sedentary behavior (257)Gentiluomo M, et al. (2024) J Endocr Soc, 8: bvae017. DOI: 10.1210/jendso/bvae017.. The study further showed that the more an individual watched television, the higher their BMI was, which partially explains why sedentary behavior like watching television increases pancreatic cancer risk (257)Gentiluomo M, et al. (2024) J Endocr Soc, 8: bvae017. DOI: 10.1210/jendso/bvae017..
Developing widespread public health campaigns to increase physical activity in the US population is vital if we are to change the current trends of sedentary lifestyles. As one example, The Active People, Healthy Nation initiative in the United States aims to help 27 million people become more physically active by 2027 by designing activity-friendly communities, encouraging physical activity at school, and consulting community leaders to implement relevant programs to encourage physical activity.
Reduce Alcohol Consumption
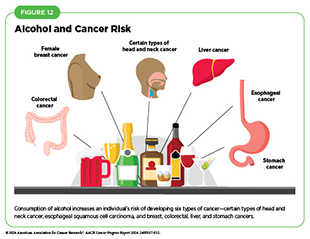
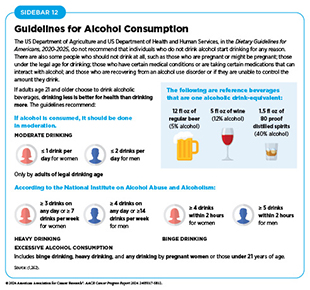
Excessive levels of alcohol consumption increase the risk for six different types of cancer (see Figure 12) and is linked to more than 200 diseases. In the United States, 5.4 percent of cancers were attributed to alcohol consumption, in 2019, the most recent year for which data are available (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. Of concern, a recent survey found that 51 percent of Americans did not know that the consumption of alcohol increases the risk of certain types of cancer, such as colorectal cancer (258)The Ohio State University Comprehensive Cancer Center. Survey: Many People Don’t Know Alcohol, High Fat Processed Foods, and Lack of Exercise Are Risk Factors for Colorectal Cancer. Accessed: July 10, 2024..
Research indicates that those who reduce alcohol consumption or stop drinking altogether can decrease their risk of developing alcohol-related cancers by 8 percent and can reduce their risk of all cancer by 4 percent compared to those who sustain or increase their consumption of alcohol (259)Yoo JE, et al. (2022) JAMA Netw Open, 5: e2228544. DOI: 10.1001/jamanetworkopen.2022.28544.. Public messaging campaigns (such as cancer-specific warning labels displayed on alcoholic beverages) along with effective clinical strategies that reduce or eliminate alcohol consumption must be considered to reduce the burden of alcohol-related cancers (see Sidebar 12).
Brief counseling interventions delivered in primary care settings can reduce excessive alcohol consumption (260)Lee AK, et al. (2023) JAMA Intern Med, 183: 319. DOI: 10.1001/jamainternmed.2022.7083.. In addition, more complex behavioral interventions and evidence-based medical interventions are effective tools in treating alcohol use disorder, though these strategies are often under-utilized despite their effectiveness in reducing alcohol consumption (261)McPheeters M, et al. (2023) JAMA, 330: 1653. DOI: 10.1001/jama.2023.19761..
Protect Skin From UV Exposure
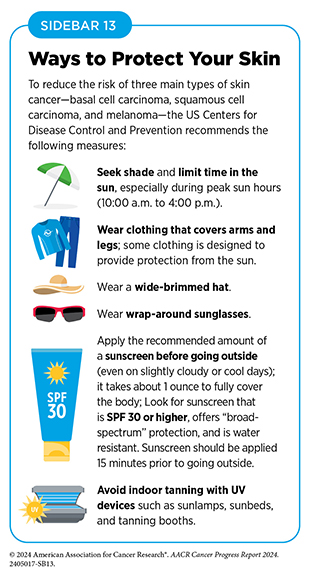
Ultraviolet (UV) radiation is a type of light emitted primarily from the sun but also from artificial sources, such as tanning beds. Exposure to all sources of UV radiation can lead to the development of skin cancers, including basal cell carcinoma, squamous cell carcinoma, and melanoma, which is the most aggressive form of skin cancer. In 2024, there will be an estimated 100,640 new diagnoses of melanoma of the skin and 8,290 deaths (see Table 1).
Ultraviolet radiation accounts for 95 percent of skin melanomas and 4.6 percent of all cancers (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.(206)Islami F, et al. (2018) CA Cancer J Clin, 68: 31. DOI: 10.3322/caac.21440.. This is because UV radiation can damage cellular DNA, with continued exposure leading to cancer. Anyone can develop skin cancer, but some people are at a higher risk, especially those who are light skinned and get easily sunburned.
It has been reported that there is a lack of understanding in the US population regarding how skin cancer develops and when to use sun protection (263)Strome A, et al. (2021) JAMA Netw Open, 4: e2134550. DOI: 10.1001/jamanetworkopen.2021.34550.. According to data from CDC, 29 percent of US adults and 64 percent of adolescents experienced sunburn at least once in the past year in 2021 (264)Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System (YRBSS). Accessed: July 5, 2023.(265)Centers for Disease Control and Prevention. National Health Interview Survey. Accessed: July 5, 2023.. This is concerning, as severe sunburn increases the risk of developing all three types of skin cancer (up to two and a half times for melanoma), compared to no history of severe sunburn (266)Wu S, et al. (2016) Am J Epidemiol, 183: 824. DOI: 10.1093/aje/kwv282.. One study reported that women who experienced at least five episodes of severe sunburns between the ages of 15 and 20 years were 80 percent more likely to develop melanoma later in life, compared to those who did not experience sunburns (267)Wu S, et al. (2014) Cancer Epidemiol Biomarkers Prev, 23: 1080..
One common misconception is that people cannot get sunburned on cloudy days. However, up to 80 percent of harmful UV sunrays can penetrate clouds. It is recommended that individuals practice sun-safe habits anytime they are outside to limit exposure to harmful UV radiation (see Sidebar 13).
Indoor tanning exposes individuals to the same harmful UV radiation as from the sun but in an artificial setting. Fortunately, rates of indoor tanning have been declining over the past decade, particularly among US youth (268)Holman DM, et al. (2019) J Community Health, 44: 1086. DOI: 10.1007/s10900-019-00685-y.. Currently, 44 states and the District of Columbia either ban or regulate the use of indoor tanning devices by minors (269)Skin Cancer Foundation. Indoor Tanning Legislation: Here’s Where We Stand. Accessed: July 5, 2023.. All states should enact legislation banning indoor tanning for minors, to continue the downward trend of tanning bed usage, especially among youth.
Prevent and Eliminate Infection From Cancer-causing Pathogens
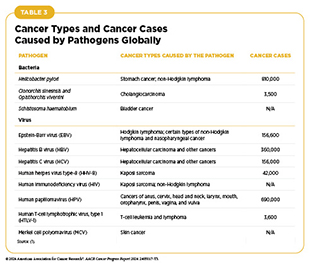
Cancer-causing pathogens (bacteria, viruses, and parasites) increase a person’s risk for several types of cancer (see Table 3). Infection with these agents can change the way a cell behaves, weaken the immune system, and cause chronic inflammation, all of which can lead to cancer. In the United States, about 3.4 percent of all cancer cases are attributable to infection with pathogens (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. Globally, an estimated 13 percent (2.2 million) of all cancer cases in 2018 were attributable to pathogenic infections, with more than 90 percent of these cases attributable to four pathogens: human papillomavirus (HPV), hepatitis B (HBV), hepatitis C (HCV), and Helicobacter pylori (212)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the Risk of Cancer. Accessed: July 6, 2023..
Individuals can significantly lower their risks by protecting themselves from infection through preventive measures such as vaccination or by seeking treatment, if available, to eliminate an infection (see Sidebar 14).
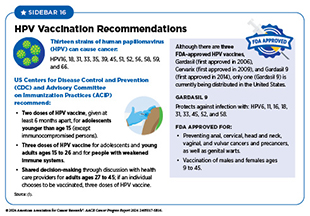
HPV is a group of more than 200 related viruses that are responsible for almost all cervical cancers, 90 percent of anal cancers, and 70 percent of oropharyngeal cancers, as well as most penile, vaginal, and vulvar cancers. While most HPV infections do not cause cancer, infection with high-risk strains of HPV for long periods of time (i.e. persistent infection) can lead to cancer. There are at least 12 high-risk HPV types and include HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59 with HPV 16 and 18 being responsible for most HPV-related cancers (270)National Cancer Institute. HPV and Cancer. Accessed: August 11, 2022.. These high-risk HPVs cause 1.2 percent and 2.5 percent of all cancers in men and women, respectively, in the United States (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858.. Globally, HPV-related cancers make up about 5 percent of all cancers (270)National Cancer Institute. HPV and Cancer. Accessed: August 11, 2022..
The HPV vaccine is approved for males and females ages 9 to 45, with recommendations for the first doses beginning at age 11 to 12 (see Sidebar 16). The HPV vaccine currently used in the United States, Gardasil 9, can protect against nine of the 12 high-risk HPV strains (see Human Papillomavirus and AYA Populations).
Chronic infection from HBV and HCV can cause liver cancer and can be a risk factor for other malignancies, such as non-Hodgkin lymphoma. Globally, the most common risk factor for liver cancer is chronic infection with HBV and HCV. In the United States, after new reported cases of HBV remained stable from 2013 through 2019, there was an abrupt decrease of 32 percent in reported cases in 2020, with a further decrease of 14 percent between 2020 and 2021 and another decrease of 6 percent in 2022 (271)Centers for Disease Control and Prevention. 2022 Hepatitis C. Viral Hepatitis Surveillance Report. Accessed: July 7, 2024.. These decreases are potentially attributable to the COVID-19 pandemic, which may have led to reduced testing but not necessarily reduced infections (272)Centers for Disease Control and Prevention. 2020 Hepatitis B. Viral Hepatitis Surveillance Report. Accessed: March 26, 2024..
For the first time since 2015, cases of acute HCV infection decreased 6 percent between 2021 and 2022 (271)Centers for Disease Control and Prevention. 2022 Hepatitis C. Viral Hepatitis Surveillance Report. Accessed: July 7, 2024.. Despite this modest decrease, rates of acute HCV infection are still two-fold higher than the rates in 2015 and are highest among persons ages 30 to 39 (271)Centers for Disease Control and Prevention. 2022 Hepatitis C. Viral Hepatitis Surveillance Report. Accessed: July 7, 2024.. To eliminate viral hepatitis as a public health threat, the US Department of Health and Human Services (HHS) released the Viral Hepatitis National Strategic Plan for the United States: A Roadmap to Elimination (2021– 2025) in 2022. The primary goals are to prevent new infections, improve health outcomes for infected individuals, reduce disparities and health inequities, increase surveillance, and bring together all relevant constituents in coordinating efforts to address the hepatitis epidemic.
Helicobacter pylori (H. pylori) is a type of bacteria that has been shown to cause gastric cancer if left untreated. This is due to inflammation of the gastric (i.e., stomach) tissue caused by H. pylori infection that, when present for an extended period, increases the likelihood of two types of cancer, gastric adenocarcinoma and gastric mucosa–associated lymphoid tissue (MALT) lymphoma, a rare type of non-Hodgkin lymphoma. H. pylori infection is higher among AI/AN communities. Among Navajo adults in Arizona, the H. pylori prevalence is 62 percent, while 74 percent of the Alaska Native population are reportedly infected with H. pylori, compared to 36 percent in the overall US population.
Large bodies of evidence have demonstrated a link between chronic H. pylori infection and the development of cancer. In geographic regions where there are high rates of H. pylori infection, such as in Asian countries, residents have a higher risk of gastric cancer (273)Han Z, et al. (2023) Helicobacter, 28: e12950. DOI: 10.1111/hel.12950.. Other epidemiologic studies show that people with chronic H. pylori infection have increased risk of developing non-cardia gastric adenocarcinoma and that treatment of H. pylori infection decreases gastric cancer risk (274)Kumar S, et al. (2020) Gastroenterology, 158: 527. DOI: 10.1053/j.gastro.2019.10.019.. Additionally, nearly all patients who develop MALT lymphoma show signs of H. pylori infection, and when these patients are treated with antibiotics, their tumors shrink (275)Parsonnet J, et al. (1994) N Engl J Med, 330: 1267. DOI: 10.1056/NEJM199405053301803.(276)Stathis A, et al. (2009) Ann Oncol, 20: 1086. DOI: 10.1093/annonc/mdn760.(277)Kiesewetter B, et al. (2013) Blood, 122: 1350. DOI: 10.1182/blood-2013-02-486522..
Fortunately, overall, new cases of H. pylori–associated gastric cancer have declined at a rate of 1.5 percent each year for the past decade; however, rates of H. pylori–associated gastric cancer are not equal among all population groups (278)Lai Y, et al. (2022) Front Public Health, 10: 1056157. DOI: 10.3389/fpubh.2022.1056157.(279)American Cancer Society. Stomach (Gastric) Cancer Key Statistics. Accessed: August 7, 2024.. Among those diagnosed with H. pylori infection, racial and ethnic minority populations and those who smoke are at a greater risk of gastric cancer (280)Garman KS, et al. (2024) Gastric Cancer, 27: 28. DOI: 10.1007/s10120-023-01448-4..
Limit Exposure to Environmental Risk Factors
Environmental pollutants are encountered in the air, drinking water, and food, making them nearly impossible to avoid. Federal government agencies, including the Environmental Protection Agency (EPA) and HHS, set guidelines for the acceptable exposure limits allowed in the environment. However, some individuals experience higher levels of exposure to certain pollutants due to their living conditions and/or daily activities. Environmental carcinogens, which are substances that can lead to cancer and are present in the environment, include arsenic, asbestos, radon, lead, radiation, and other chemical pollutants. Exposure to higher than acceptable levels of environmental carcinogens, without appropriate protection, can increase the risk of cancer. The International Agency for Research on Cancer (IARC) and the US National Toxicology Program (NTP) are both responsible for evaluating substances and exposures and classifying them as carcinogens at the global and national level, respectively.
Of increasing concern among public health experts is climate change, which refers to a change in temperature and weather patterns across the globe because of human activity. There is strong scientific evidence that climate change is occurring, and that it has the potential to worsen exposure to carcinogens. For instance, wildfires in the western United States and Canada, which have increased in intensity in recent years due to climate change (281)US Global Change Research Program. Fourth National Climate Assessment. Volume II: Impacts, Risks, and Adaptation in the United States. Accessed: March 17, 2024., have led to increased exposure to certain metal toxins, such as carcinogenic forms of chromium known to increase cancer risk (282)Lopez AM, et al. (2023) Nat Commun, 14: 8007. DOI: 10.1038/s41467-023-43101-9..
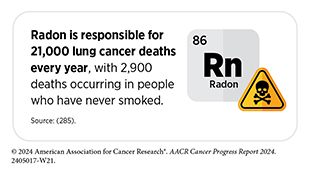
Radon is a naturally occurring radioactive gas that is produced from the breakdown of uranium in soil, rock, and water. Radon gas can seep into homes through cracks in the floor or walls and through gaps around pipes, wires, or pumps. The levels of naturally occurring radon vary widely based on geographic location and are highest in areas rich in radioactive ore. Additionally, byproducts from previous mining of uranium—for example in the Southwest—have led to increased levels of radon in nearby areas (177)Yazzie SA, et al. (2020) Int J Environ Res Public Health, 17: 2813. DOI: 10.3390/ijerph17082813..
Radon is the number one cause of lung cancer among non-smokers and is the second leading cause of lung cancer overall, contributing to approximately 12 percent of lung cancers in the United States annually (283)Riudavets M, et al. (2022) Cancers (Basel), 14: 3142. DOI: 10.3390/cancers14133142.(284)Liu Y, et al. (2024) Crit Rev Oncol Hematol, 198: 104363. DOI: 10.1016/j.critrevonc.2024.104363.(285)United States Environmental Protection Agency. Health Risk of Radon. Accessed: July 7, 2024..
Radon testing using approved test kits, especially in crawl spaces and basements where radon is most concentrated, should be used to mitigate exposure. EPA maintains a database of resources available to obtain radon testing kits, sometimes at little to no cost.
Living near industrial areas can increase exposure to toxic chemicals and metals. These exposures can increase the risk for certain types of cancer, such as hematologic malignancies as well as thyroid, lung, breast, and uterine cancers (175)Carroll R, et al. (2023) Environ Res, 239: 117349. DOI: 10.1016/j.envres.2023.117349.(176)Cheng I, et al. (2022) Am J Respir Crit Care Med, 206: 1008. DOI: 10.1164/rccm.202107-1770OC.(286)Jephcote C, et al. (2020) Environ Health, 19: 53. DOI: 10.1186/s12940-020-00582-1.(287)van Gerwen M, et al. (2023) EBioMedicine, 97: 104831. DOI: 10.1016/j.ebiom.2023.104831.(288)Liu H, et al. (2023) Front Oncol, 13: 1282651. DOI: 10.3389/fonc.2023.1282651..
Air pollution is contamination of the indoor or outdoor environment by any chemical, physical, or biological agent that modifies the natural characteristics of the atmosphere with major pollutants including particulate matter, carbon monoxide, ozone, nitrogen dioxide, and sulfur dioxide. In 2013, IARC concluded that particle pollution may cause lung cancer and subsequently classified it as a potential cause of cancer in humans (289)Loomis D, et al. (2013) Lancet Oncol, 14: 1262. DOI: 10.1016/s1470-2045(13)70487-x.(290)Berg CD, et al (2023) J Thorac Oncol, 18: 1277. DOI: 10.1016/j.jtho.2023.05.024.. Air pollution may also be attributable to polycyclic aromatic hydrocarbons (PAHs), which are chemicals that have been associated with several cancers, including cancers of the lung and breast (291)Shen J, et al. (2017) Br J Cancer, 116: 1229. DOI: 10.1038/bjc.2017.81.(292)Korsh J, et al. (2015) Breast Care (Basel), 10: 316. DOI: 10.1159/000436956..
In 2024, 131.2 million people lived in places with unhealthy levels of particulate pollution and 63.7 million people living in the United States were exposed to daily, unhealthy spikes in particle pollution (30)American Lung Association. State of the Air 2023 Report. Accessed: March 17, 2024.. This equates to 11.7 percent more people exposed to daily, unhealthy spikes compared to 2023 (30)American Lung Association. State of the Air 2023 Report. Accessed: March 17, 2024.. Low-income populations and racial and ethnic minority groups are among those who often experience higher exposure to pollutants (30)American Lung Association. State of the Air 2023 Report. Accessed: March 17, 2024.(173)Bradley AC, et al. (2024) Environ Sci Technol, 58: 4226. DOI: 10.1021/acs.est.3c03230.(174)Tessum CW, et al. (2021) Sci Adv, 7: eabf4491. DOI: 10.1126/sciadv.abf4491.. Those who live in urban areas, particularly those with low socioeconomic status, are exposed to higher levels of certain traffic-related air pollutants, which are associated with an increased risk of lung cancer (175)Carroll R, et al. (2023) Environ Res, 239: 117349. DOI: 10.1016/j.envres.2023.117349.(176)Cheng I, et al. (2022) Am J Respir Crit Care Med, 206: 1008. DOI: 10.1164/rccm.202107-1770OC..
Increasingly, the use of flame-retardant compounds in car interiors, building materials, and other consumable products are being recognized as carcinogenic. Several studies have demonstrated that these compounds are linked to increasing cancer risk, with one study showing consistent exposure to a common flame retardant significantly increased the risk of cancer mortality by 300 percent (293)Liu B, et al. (2024) JAMA Netw Open, 7: e243127. DOI: 10.1001/jamanetworkopen.2024.3127.(294)Hoehn RM, et al. (2024) Environ Sci Technol, 58: 8825. DOI: 10.1021/acs.est.3c10440..
The endocrine system is made up of the glands and organs that make hormones and release them directly into the blood so they can travel to, and regulate the functions of, body tissues and organs. Endocrine-disrupting chemicals can be natural or human-made, and may mimic, block, or interfere with the body’s hormones. Endocrine-disrupting chemicals, such as per- and poly-fluoroalkyl substances (PFAS) or chlordane, hexachlorocyclohexane, and polychlorinated biphenyls, have been shown to increase the risk of certain cancers, such as thyroid and breast cancers (287)van Gerwen M, et al. (2023) EBioMedicine, 97: 104831. DOI: 10.1016/j.ebiom.2023.104831.(288)Liu H, et al. (2023) Front Oncol, 13: 1282651. DOI: 10.3389/fonc.2023.1282651.. An emerging concern is the use of personal care products, such as hair straightening products, which contain hazardous chemicals with endocrine-disrupting properties and are associated with increased risk of uterine and breast cancers (295)Chang CJ, et al. (2022) J Natl Cancer Inst, 114: 1636. DOI: 10.1093/jnci/djac165.(296)Bertrand KA, et al. (2023) Environ Res, 239: 117228. DOI: 10.1016/j.envres.2023.117228.(297)Llanos AAM, et al. (2017) Carcinogenesis, 38: 883. DOI: 10.1093/carcin/bgx060..
Drinking water can also contain contaminants including PFAS, asbestos, arsenic, radon, agricultural chemicals, and hazardous waste (298)Morris RD (1995) Environ Health Perspect, 103 Suppl 8: 225. DOI: 10.1289/ehp.95103s8225.. American Indian or Alaska Native (AI/AN) individuals are 19 times more likely than White individuals to live in a household without indoor plumbing, requiring them to source water from communal wells (299)Harris RB, et al. (2022) Int J Environ Res Public Health, 19: 797. DOI: 10.3390/ijerph19020797.(300)Tanana H, et al. (2021) Health Secur, 19: S78. DOI: 10.1089/hs.2021.0034.. These water sources are more prone to being contaminated with bacteria, arsenic, and uranium (299)Harris RB, et al. (2022) Int J Environ Res Public Health, 19: 797. DOI: 10.3390/ijerph19020797.(300)Tanana H, et al. (2021) Health Secur, 19: S78. DOI: 10.1089/hs.2021.0034., all of which increase the risk of several types of cancer, including gastric, liver, lung, bladder, and kidney cancers (298)Morris RD (1995) Environ Health Perspect, 103 Suppl 8: 225. DOI: 10.1289/ehp.95103s8225.(299)Harris RB, et al. (2022) Int J Environ Res Public Health, 19: 797. DOI: 10.3390/ijerph19020797.(301)Wroblewski LE, et al. (2010) Clin Microbiol Rev, 23: 713. DOI: 10.1128/CMR.00011-10.. Evidence also demonstrates that pollution with PFAS is higher in communities in proximity to polluting industries such as airports, industrial sites, wastewater treatment plants, and military fire training areas (302)Liddie JM, et al. (2023) Environmental Science & Technology, 57: 7902. DOI: 10.1021/acs.est.2c07255..
Coordinated efforts such as those being initiated by Cohorts for Environmental Exposures and Cancer Risks, build collaborative infrastructure, and facilitate integrated scientific research for enhancing the understanding of environmental exposures influencing cancer etiology, and the genetic, behavioral, and structural factors that modify risk across diverse populations.
Higher than normal levels of exposure to carcinogens have led IARC to classify certain occupations, such as firefighting and industrial painting, and work environments, such as iron and steel foundries or working around welding fumes, as class 1 carcinogens, meaning they are cancer-causing to humans. For instance, firefighters are at a greater risk of developing several types of cancer because of the constant exposure to smoke and other hazardous materials (303)Lee DJ, et al. (2023) Front Oncol, 13: 1130754. DOI: 10.3389/fonc.2023.1130754.(304)Kunz KR, et al. (2023) Front Public Health, 11: 1126066. DOI: 10.3389/fpubh.2023.1126066.. To reduce the risk of occupational exposure to carcinogens, workers should consistently wear personal protective equipment (PPE) that reduces or eliminates their exposure and decontaminate PPE after working in environments with carcinogens and other hazardous materials.
Other risk factors associated with a person’s occupation, including lack of sleep and night-shift work, have also been shown to increase their risk of developing certain types of cancers and other chronic diseases including diabetes and obesity (305)McDermott JE, et al. (2024) J Proteome Res, 23: 1547. DOI: 10.1021/acs.jproteome.3c00418.. CDC reports that about 11 million adults in the United States frequently work night shifts, with certain groups, such as men, and Black and non-Hispanic individuals, more likely to do this type of work. In one recent study, researchers found that women age 50 or older who worked both day and night shifts were twice as likely to develop breast cancer as those who only worked day shifts (306)International Agency for Research on Cancer Working Group on the Identification of Carcinogenic Hazards to Humans. Night Shift Work. Accessed: March 17, 2024..
Although the underlying mechanisms are not clear, researchers believe that disruption of the body’s circadian rhythm (i.e., the internal clock) can alter biological processes that normally prevent cancer development (307)Huang C, et al. (2023) Cancer Biol Med, 20: 1. DOI: 10.20892/j.issn.2095-3941.2022.0474.. Emerging research indicates that avoiding lighting that disrupts circadian rhythms, for example, lighting that is low in blue light, may help reduce cancer risk (308)Sahin L, et al. (2022) Lighting Research & Technology, 54: 441. DOI: 10.1177/14771535211040985.(309)Figueiro MG, et al. (2010) Int J Endocrinol, 2010: 829351. DOI: 10.1155/2010/829351.(310)Faraut B, et al. (2019) Front Neurosci, 13: 1366. DOI: 10.3389/fnins.2019.01366.. Long-term research is needed to understand how avoiding exposure to certain light sources, particularly at night, may help regulate the circadian rhythms and thus may reduce cancer risk.
As we learn more about environmental and occupational cancer risk factors and identify those segments of the US population who are exposed to these factors, new and equitable policies need to be developed and implemented to reduce cancer risk and improve the health of all populations.
Be Cognizant of Hormonal Factors
Pregnancy and Breastfeeding
Studies have shown that a woman’s risk of developing breast cancer is associated with reproductive factors such as pregnancy and breastfeeding that regulate their exposure to estrogen and progesterone, two hormones produced by their ovaries. Evidence has shown that women who have given birth are at a reduced risk of developing estrogen receptor–positive (ER+) tumors compared to women who have never given birth. However, this protective effect is only observed a decade or more after a woman’s last pregnancy (311)Nichols HB, et al. (2019) Ann Intern Med, 170: 22. DOI: 10.7326/M18-1323.(312)Ambrosone CB, et al. (2020) Cancer Res, 80: 4871.(313)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706. DOI: 10.1093/jnci/djac117..
During the period immediately following pregnancy, women are at an elevated risk of developing pregnancy-associated breast cancers, which refer to breast cancers diagnosed during gestation, lactation, and within five years postpartum (314). Evidence has demonstrated that both estrogen receptor–negative (ER–) tumors and triple-negative breast cancer are the most common subtypes of pregnancy-associated cancers (311)Nichols HB, et al. (2019) Ann Intern Med, 170: 22. DOI: 10.7326/M18-1323.(313)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706. DOI: 10.1093/jnci/djac117.(315)Vohra SN, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 561.. In the United States, there are about 3,500 cases of pregnancy-associated breast cancer each year (314)Proussaloglou EM, et al. (2023) Pathol Res Pract, 244: 154413. DOI: 10.1016/j.prp.2023.154413.. Furthermore, the mother’s age at pregnancy also influences breast cancer risk. Women who are older when they become pregnant are at increased risk of certain types of breast cancer (316)John EM, et al. (2024) Breast Cancer Res, 26: 88. DOI: 10.1186/s13058-024-01834-5..
Breastfeeding, specifically lactation, has been linked with a reduced risk of breast cancer (317)Millikan RC, et al. (2008) Breast Cancer Res Treat, 109: 123. DOI: 10.1007/s10549-007-9632-6.(318)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723.(319)Fortner RT, et al. (2019) Breast Cancer Res, 21: 40. DOI: 10.1186/s13058-019-1119-y., with increased duration of breastfeeding associated with further decrease in risk (212)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the Risk of Cancer. Accessed: July 6, 2023.(313)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706. DOI: 10.1093/jnci/djac117.(318)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723.(320)Anstey EH, et al. (2017) Am J Prev Med, 53: S40. DOI: 10.1016/j.amepre.2017.04.024.(321)Palmer JR, et al. (2014) J Natl Cancer Inst, 106: dju237. DOI: 10.1093/jnci/dju237.(322)John EM, et al. (2018) Int J Cancer, 142: 2273. DOI: 10.1002/ijc.31258.. A recent analysis evaluating the association of pregnancy and breastfeeding with the development of breast cancer found that breastfeeding was consistently associated with decreased risk of all subtypes of breast cancer (323)Mao X, et al. (2023) BMC Cancer, 23: 644. DOI: 10.1186/s12885-023-11049-0.. However, this risk differed across race and ethnicities.
Fully understanding the relationship of pregnancy and breastfeeding with the risk of breast cancer in women will be important to implement interventional strategies that can reduce this risk.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) refers to treatments that aim to relieve the common symptoms of menopause and the long-term biological changes, such as bone loss, that take place after menopause. These changes occur due to the decline in levels of the hormones estrogen and progesterone. HRT usually involves treatment with estrogen and progestin or estrogen alone in women who have undergone a hysterectomy, which is the surgery to remove all or part of the uterus. This is because when estrogen is given alone, but not in combination with progestin, it is associated with an increased risk of endometrial cancer, a type of cancer that forms in the tissue lining of the uterus.
Data show that women who use the estrogen and progestin combination have an increased risk of developing breast cancer (324)Chlebowski RT, et al. (2020) JAMA, 324: 369. DOI: 10.1001/jama.2020.9482.(325)Chlebowski RT, et al. (2008) Arch Intern Med, 168: 370. DOI: 10.1001/archinternmed.2007.123.. The risk is greater with longer duration of use and is nearly two-fold higher among women who have used estrogen and progestin in combination for 10 years or longer compared to those who never used HRT (326)Chlebowski RT, et al. (2009) N Engl J Med, 360: 573. DOI: 10.1056/NEJMoa0807684.(327)Collaborative Group on Hormonal Factors in Breast C (2019) Lancet, 394: 1159. DOI: 10.1016/S0140-6736(19)31709-X.(328)Wang SM, et al. (2020) Breast Cancer Res, 22: 129. DOI: 10.1186/s13058-020-01365-9.. Women who are no longer using HRT have a lower risk than current users but remain at an elevated risk for more than a decade after they have stopped taking the drugs (327)Collaborative Group on Hormonal Factors in Breast C (2019) Lancet, 394: 1159. DOI: 10.1016/S0140-6736(19)31709-X.. Individuals who seek HRT should discuss with their health care providers the advantages and possible risks, before deciding what is right for them.
One area of ongoing investigation in exogenous hormone use is the differential cancer risks among individuals undergoing gender-affirming hormonal therapy (GAHT) (329)Jackson SS, et al. (2022) Trends Cancer, 8: 273. DOI: 10.1016/j.trecan.2022.01.005.. While current data are limited, there is emerging evidence indicating an increased risk of breast cancer, but a lower risk of prostate cancer, among trans women who received GAHT compared to age-matched cisgender men. Trans men who received GAHT had a lower risk of breast cancer compared to age-matched cisgender women (330)de Blok CJM, et al. (2019) BMJ, 365: l1652. DOI: 10.1136/bmj.l1652.(331)de Nie I, et al. (2020) J Clin Endocrinol Metab, 105: e3293. DOI: 10.1210/clinem/dgaa412.. New evidence indicates that this lower risk of breast cancer in trans men may be due to protective effects of receiving androgen therapy during their transition (332)Raths F, et al. (2023) Cell Genom, 3: 100272. DOI: 10.1016/j.xgen.2023.100272.. Long-term population-based studies are needed to comprehensively assess the risk of cancers in these understudied and medically underserved populations.

Increasing Cancer Risk Among Children and AYAs
Inherited genetic mutations play an important role in cancer development in children and AYA. Modifiable risk factors play a far less critical role in the development of childhood cancers compared to cancers in adults. Regardless, there is some evidence that exposure to certain modifiable factors can increase the risk of cancer among children, as discussed below.
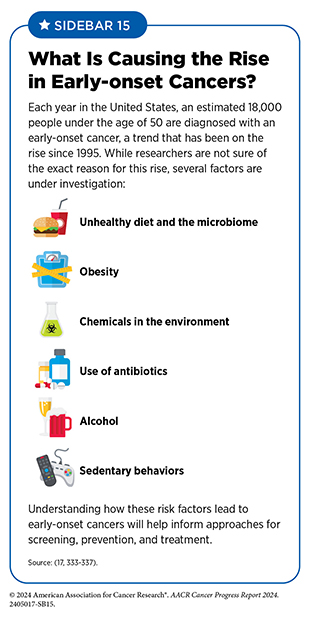
AYA individuals can be exposed to the same types of modifiable cancer risk factors as adults. When combined with genetic predispositions, e.g., Lynch syndrome (see Genetic Alterations), such exposures can further increase the risk of cancer development. There has been a rise in certain types of early-onset cancers caused by a combination of factors including genetic predisposition, diet, and obesity. Infection with certain pathogens can also increase the risk of cancer in this group (see Sidebar 15). This section discusses the unique risk factors faced by children and AYA individuals.
Tobacco Use in Children and AYAs
Exposure to smoking and its byproducts, either in the womb or through secondhand smoke exposure, can increase cancer risk for children and AYAs (338)Rudant J, et al. (2008) Cancer Causes Control, 19: 1277. DOI: 10.1007/s10552-008-9199-5.(339)Metayer C, et al. (2013) Cancer Epidemiol Biomarkers Prev, 22: 1600.(340)Chang JS, et al. (2006) Am J Epidemiol, 163: 1091. DOI: 10.1093/aje/kwj143.(341)Boffetta P, et al. (2000) Environ Health Perspect, 108: 73. DOI: 10.1289/ehp.0010873.
(342)Centers for Disease Control and Prevention. Smoking, Pregnancy, and Babies. Accessed: July 7, 2024..
Smoking during pregnancy can lead to many adverse health effects, including complications such as birth defects, premature birth/low birth weight, damage to the organs of the developing fetus, and increased risk of cancer after the child is born (339)Metayer C, et al. (2013) Cancer Epidemiol Biomarkers Prev, 22: 1600.(340)Chang JS, et al. (2006) Am J Epidemiol, 163: 1091. DOI: 10.1093/aje/kwj143.(341)Boffetta P, et al. (2000) Environ Health Perspect, 108: 73. DOI: 10.1289/ehp.0010873.(342)Centers for Disease Control and Prevention. Smoking, Pregnancy, and Babies. Accessed: July 7, 2024.(343)Stjernfeldt M, et al. (1986) Lancet, 1: 1350. DOI: 10.1016/s0140-6736(86)91664-8.. As one example, it has been observed that mothers who are pregnant and smoke increase the risk of brain and central nervous system tumors after the birth of the child (344)Rumrich IK, et al. (2016) PLoS One, 11: e0165040. DOI: 10.1371/journal.pone.0165040.. Another study found that maternal smoking during pregnancy doubled the risk of gliomas and tripled the risk of retinoblastomas in children 5 years or younger (345)Heck JE, et al. (2016) Int J Cancer, 139: 613. DOI: 10.1002/ijc.30111..
Secondhand smoke, which can cause spontaneous miscarriage in pregnant women, can increase the risk of childhood acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) (341)Boffetta P, et al. (2000) Environ Health Perspect, 108: 73. DOI: 10.1289/ehp.0010873.(347)Milne E, et al. (2012) Am J Epidemiol, 175: 43. DOI: 10.1093/aje/kwr275.(348)Chunxia D, et al. (2019) Medicine (Baltimore), 98: e16454. DOI: 10.1097/MD.0000000000016454.(349)Edraki M, et al. (2011) East Mediterr Health J, 17: 303.. Secondhand smoke exposure among children has also been found to increase the development of lung cancer in adulthood (350)Tredaniel J, et al. (1994) Paediatr Perinat Epidemiol, 8: 233. DOI: 10.1111/j.1365-3016.1994.tb00455.x..
Smoking during adolescence is a strong predictor of continued tobacco use as an adult, and smoking in AYA populations can increase the risk of cancer, particularly lung cancer, during adulthood (see Eliminate Tobacco Use). US states that have a higher prevalence of smoking among AYA groups have higher rates of cancer, independent of educational attainment, employment, or economic status (351)Jacob A, et al. (2020) J Clin Oncol, 38: e13626. DOI: 10.1200/JCO.2020.38.15_suppl.e13626..
Body Weight, Diet, and Physical Activity in Children and AYAs
Although being overweight or obese does not necessarily lead to cancer in children and adolescent groups, data show that being overweight or obese during this stage of life increases the likelihood of developing cancer as an adult (352)Jensen BW, et al. (2023) J Natl Cancer Inst, 115: 43. DOI: 10.1093/jnci/djac192.. For instance, men with high BMI at the age of 18 were more likely to develop cancers as older adults (on average, 30 years later) compared to those with a normal BMI (353)Onerup A, et al. (2024) Obesity (Silver Spring), 32: 376. DOI: 10.1002/oby.23942.. Another study found that weight gain after the age of 18 increased breast cancer incidence in postmenopausal but not in premenopausal women (354)Han Y, et al. (2024) Breast Cancer Res, 26: 39. DOI: 10.1186/s13058-024-01804-x.. Therefore, the rise in obesity among children and teens (2 to 19 years of age) in the past five decades, from 5 percent in the 1970s to approximately 19.7 percent during the period between 2017 and 2020 is concerning (355)Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. Accessed: March 17, 2024.. It is imperative that all stakeholders work together to address the rise in obesity among all age groups, with early interventions among the youngest and most vulnerable being essential to reducing obesity as adults.
In AYA populations, there is a worrying increase in early-onset cancers, which research indicates is due to a combination of genetic risk factors coupled with the obesity epidemic, poor diet, and a lack of physical activity (see Sidebar 15). Of particular concern is the recent rise in early-onset colorectal cancer (EOCRC). In the United States, rates of EOCRC are expected to double by 2030 among those 29 to 35 years old, while rates in older adults are expected to decrease (18)Sinicrope FA (2022) N Engl J Med, 386: 1547. DOI: 10.1056/NEJMra2200869.(356)Rahib L, et al. (2021) JAMA Netw Open, 4: e214708. DOI: 10.1001/jamanetworkopen.2021.4708.(357)Saraiva MR, et al. (2023) World J Gastroenterol, 29: 1289. DOI: 10.3748/wjg.v29.i8.1289.. Although mechanisms are not entirely known, it is becoming increasingly clear that genetics, coupled with modifiable risk factors such as obesity and alcohol, is attributable to the rise in EOCRC (358)Laskar RS, et al. (2024) Ann Oncol, 35: 523. DOI: 10.1016/j.annonc.2024.02.008.(359)Chen J, et al. (2024) Int J Cancer, 154: 1930. DOI: 10.1002/ijc.34887.(360)Dai R, et al. (2024) Cancers (Basel), 16: 676. DOI: 10.3390/cancers16030676..
Eating a healthy diet can help reduce the risk of many chronic conditions, including cancer (see Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active). Unfortunately, compared to other age groups, the diet quality of adolescents is poor, with elevated consumption of foods that are high in fat and refined carbohydrates and low in fiber, and inadequate consumption of fresh fruits and vegetables (361)Hu K, et al. (2023) J Nutr Educ Behav, 55: 851. DOI: 10.1016/j.jneb.2023.10.003.(362)Lipsky LM, et al. (2017) Am J Clin Nutr, 105: 1424. DOI: 10.3945/ajcn.116.150029.. The poor uptake of healthy foods among this population can be due to numerous factors, including food insecurity, family dietary habits, convenience, and lack of affordable access to healthy foods (363)Livingstone KM, et al. (2023) Int J Behav Nutr Phys Act, 20: 70. DOI: 10.1186/s12966-023-01477-3.. The poor dietary patterns can carry on into adulthood and increase the risk of many obesity-associated cancers (361)Hu K, et al. (2023) J Nutr Educ Behav, 55: 851. DOI: 10.1016/j.jneb.2023.10.003. (see Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active) (364)Joh HK, et al. (2021) Gastroenterology, 161: 128. DOI: 10.1053/j.gastro.2021.03.028.(365)Hur J, et al. (2021) Gut, 70: 2330. DOI: 10.1136/gutjnl-2020-323450.. Reducing or eliminating consumption of highly processed foods, fast foods, and foods and beverages high in sugar is essential to curbing the obesity epidemic and reducing the burden of associated cancers.
Emerging evidence has demonstrated that antibiotics, which are commonly prescribed to eliminate bacterial infections, may increase the risk of early-onset colorectal cancer (366)Jiang F, et al. (2023) Int J Cancer, 153: 1602. DOI: 10.1002/ijc.34648.(367)McDowell R, et al. (2022) Br J Cancer, 126: 957. DOI: 10.1038/s41416-021-01665-7.(368)Chao C, et al. (2024) J Clin Oncol, 42: e15653. DOI: 10.1200/JCO.2024.42.16_suppl.e15653.. Higher rates of antibiotic consumption among those younger than 50 years of age were associated with an increase of 1.5 times in colon cancer incidence compared to an increase of only 1.1 times in those older than 50 (367)McDowell R, et al. (2022) Br J Cancer, 126: 957. DOI: 10.1038/s41416-021-01665-7.. While the mechanisms of this increase are not well understood, researchers believe that antibiotics disrupt the normal gut bacteria, called the microbiome, upsetting the careful balance that promotes a healthy digestive system.
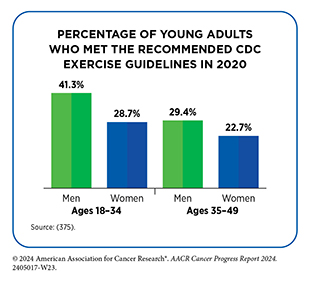
Key to maintaining a healthy weight and reducing the risk of cancer in all age groups is meeting the recommended CDC guidelines for physical activity (see Sidebar 11). Unfortunately, 20 percent of US children ages 6 to 17 do not meet the guideline of a minimum of 60 minutes of exercise per day (369)Kuzik N, et al. (2023) Front Public Health, 11: 1172168. DOI: 10.3389/fpubh.2023.1172168.. This is concerning because childhood physical activity level predicts future physical activity levels as an adult (370)Telama R, et al. (2005) Am J Prev Med, 28: 267. DOI: 10.1016/j.amepre.2004.12.003.(371)Fraser BJ, et al. (2017) J Sci Med Sport, 20: 927. DOI: 10.1016/j.jsams.2017.03.021.(372)Pongiglione B, et al. (2020) Int J Epidemiol, 49: 1749. DOI: 10.1093/ije/dyaa131.. Further evidence has linked low physical activity levels at a young age with the risk for developing cancer as an adult (373,374). Lower levels of exercise are also observed among young adults and adults, with only one third of young adults meeting the recommended physical activity guidelines. Unfortunately, the amount of exercise only trends downward among those ages 35 to 49.
Regular exercise can improve overall health and reduce negative health outcomes for all age groups; however, adopting healthy exercise patterns early on in life can reduce the likelihood of chronic diseases, including cancer, in adulthood.
Alcohol Exposure in Children and AYAs
For women who are pregnant, alcohol consumption can affect the developing fetus and increase the risk of childhood cancer after birth. Research has shown an association between the degree of alcohol consumed during pregnancy and the likelihood of the child developing leukemia after birth up to the age of 14 (376)Orsi L, et al. (2015) Cancer Causes Control, 26: 1003. DOI: 10.1007/s10552-015-0593-5.(377)Karalexi MA, et al. (2017) Eur J Cancer Prev, 26: 433. DOI: 10.1097/CEJ.0000000000000350.. A large meta-analysis found that moderate drinking during pregnancy increased the risk of AML in offspring by 1.6 times, while high alcohol consumption increased AML risk by 2.4 times (377)Karalexi MA, et al. (2017) Eur J Cancer Prev, 26: 433. DOI: 10.1097/CEJ.0000000000000350..
Alcohol intake at an early age can increase the risk of cancer later in life (378)Mayen AL, et al. (2022) Eur J Epidemiol, 37: 915. DOI: 10.1007/s10654-022-00900-6.(379)Jin EH, et al. (2023) J Clin Oncol, 41: 3816. DOI: 10.1200/JCO.22.01895.. One study found that those who have high consumption of alcohol in early adulthood increased the risk of early-onset colorectal cancer 1.5 times compared to those who did not consume alcohol even after adjusting for other factors like smoking (336)Hur J, et al. (2021) Eur J Epidemiol, 36: 325. DOI: 10.1007/s10654-021-00723-x..
The rise in early-onset cancers has also been attributed to the consumption of alcohol earlier in life; however, the research is still ongoing to confirm these findings (60)Ugai T, et al. (2022) Nat Rev Clin Oncol, 19: 656. DOI: 10.1038/s41571-022-00672-8.(379)Jin EH, et al. (2023) J Clin Oncol, 41: 3816. DOI: 10.1200/JCO.22.01895.(380)O’Sullivan DE, et al. (2022) Clin Gastroenterol Hepatol, 20: 1229. DOI: 10.1016/j.cgh.2021.01.037.(381)Chen X, et al. (2022) EClinicalMedicine, 49: 101460. DOI: 10.1016/j.eclinm.2022.101460.. Continued research into the effects of alcohol exposure on cancer risk in children and AYAs is necessary to reverse the upward trend of early-onset cancers.
Human Papillomavirus and AYA Populations
Thanks to the development of the HPV vaccine nearly two decades ago, those who receive the vaccine as children nearly eliminate their risk of developing HPV-associated cancers. The HPV vaccine is approved for males and females ages 9 to 45, with recommendations for the first doses beginning at age 11 to 12 (see Sidebar 16).
Despite clear evidence showing that the HPV vaccine reduces cervical cancer incidence, the uptake of the vaccine has been suboptimal in the United States (382)Mix JM, et al. (2021) Cancer Epidemiol Biomarkers Prev, 30: 30.. This is partly because there is no national mandate in the United States requiring HPV vaccination to attend school. However, some states have implemented their own vaccine requirements. As of 2024, four US states (Hawaii, Rhode Island, Virginia, and the District of Columbia) require the vaccine for entry into secondary schools. Rural areas have very low rates of HPV vaccination among teens, necessitating culturally tailored interventions to increase vaccination in these populations (383)Swiecki-Sikora AL, et al. (2019) J Rural Health, 35: 506. DOI: 10.1111/jrh.12353..
In 2022, only 62.6 percent of eligible children and adolescents (ages 13-17 years) had received the recommended two doses (384)Pingali C, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 912. DOI: 10.15585/mmwr.mm7234a3.. While these numbers have improved compared to past years, rates of HPV vaccination in the US have been lower than in other countries such as the United Kingdom (UK) and Australia. In 2022, in the US, only 38.6 percent of children ages 9 to 17 had received one or more doses of the HPV vaccine, compared to 76.5 percent of children in the UK and 84.2 percent of children in Australia (385)Australian Government Department of Health and Aged Care. Human papillomavirus (HPV) immunisation data. Accessed: August 7, 2024.(386)UK Health Security Agency. Human papillomavirus (HPV) vaccination coverage in adolescents in England: 2022 to 2023. Accessed: August 7, 2024.(387)Centers for Disease Control and Prevention. Human Papillomavirus Vaccination Coverage in Children Ages 9–17 Years: United States, 2022. Accessed: August 7, 2024.. Historically higher rates of vaccination have led to near eradication of cervical cancer among women in some countries. For example, in 2020 in Scotland, no new cases of cervical cancer were reported among AYA women who were vaccinated against HPV between 1988 and 1996 (388)Palmer TJ, et al. (2024) J Natl Cancer Inst, 116: 857. DOI: 10.1093/jnci/djad263..
Environmental Risk Factors in Children and AYAs
Studies have evaluated how exposure to environmental carcinogens, specifically in children and young adults, can increase the risk of certain types of cancers.
Exposure of AYA and children to pesticides either directly through work in the agricultural industry or indirectly from wastewater, in the air, or from cohabitating with family members who work on farms, can increase the risk of developing certain types of cancers, such as childhood leukemia (389)Karalexi MA, et al. (2021) Environ Pollut, 285: 117376. DOI: 10.1016/j.envpol.2021.117376.(390)Gunier RB, et al. (2017) Environ Res, 156: 57. DOI: 10.1016/j.envres.2017.03.001.(391)Patel DM, et al. (2020) Int J Cancer, 146: 943. DOI: 10.1002/ijc.32388.(392)Hyland C, et al. (2018) Int J Cancer, 143: 1295. DOI: 10.1002/ijc.31522.. Exposure to pesticides during pregnancy has been shown to increase the risk of leukemia after birth and during adolescence (393)Park AS, et al. (2020) Int J Hyg Environ Health, 226: 113486. DOI: 10.1016/j.ijheh.2020.113486..
Parental occupations that are associated with using known carcinogens have also been associated with increasing cancer risk in children who live in the same household (394)Rossides M, et al. (2022) Environ Health Perspect, 130: 77002. DOI: 10.1289/EHP11035.(395)Savitz DA, et al. (1990) Environ Health Perspect, 88: 325. DOI: 10.1289/ehp.9088325.. One study found that occupational exposure among parents to crystalline silica, common in mining and demolition work, and/or chromium doubled the risk of childhood ALL and AML (396)Onyije FM, et al. (2022) Environ Int, 167: 107409. DOI: 10.1016/j.envint.2022.107409..
Air pollution, which is composed of fine particulate matter, has also been shown to increase mortality from cancer in children and AYAs. Certain levels of air pollution can increase cancer mortality for childhood lymphomas and central nervous system tumors as well as AYA central nervous system tumors and carcinomas (397)Ou JY, et al. (2020) Cancer Epidemiol Biomarkers Prev, 29: 1929..
Continued research into understanding the types and duration of exposures to environmental carcinogens and how these exposures increase the risk of cancers among children and AYA populations is essential.
Next Section: Screening for Early Detection Previous Section: Understanding the Path to Cancer Development