- Challenges Faced by Cancer Survivors
- Physical Challenges
- Unique Challenges Faced by Pediatric and Adolescent and Young Adult (AYA) Cancer Survivors
- Health-related Quality of Life
- Financial Toxicity
- Promoting Healthy Behaviors
- Integrating Palliative Care
- Improving Mental Health
- Supporting Caregivers
- Paving the Way for Health Equity in Cancer Survivorship
Disparities in Cancer Survivorship
In this section, you will learn:
- Cancer survivorship encompasses the physical and mental health–related issues, as well as the social and financial challenges, encountered by anyone who has received a cancer diagnosis.
- Patients belonging to racial and ethnic minority groups and medically underserved populations experience higher rates of adverse side effects, poorer quality of life, and higher financial toxicity from a cancer diagnosis.
- To improve the survivorship experience for racial and ethnic minority groups and medically underserved populations, patient navigators, patient advocates, and culturally sensitive intervention/navigation programs need to be used.
According to the NCI, a person is considered a cancer survivor from the time of cancer diagnosis through the balance of the person’s life. With 18.1 million cancer survivors in the United States as of 2022, many more people are living through and beyond their cancer. While these numbers are promising, medically underserved populations have higher rates of morbidity and mortality for many types of cancers (42)Haque AT, et al. (2023) J Natl Cancer Inst, 115: 822. [LINK NOT AVAILABLE](799)Gorin SS, et al. (2017) Ann Behav Med, 51: 532. [LINK NOT AVAILABLE]. With the number of US individuals over the age of 65 and the diversity of the US population increasing, the number of cancer survivors who belong to racially and ethnically minoritized groups is projected to grow over the next few decades. Unless more equitable cancer control efforts are put in place, disparities across the cancer continuum, including survivorship, will potentially widen.
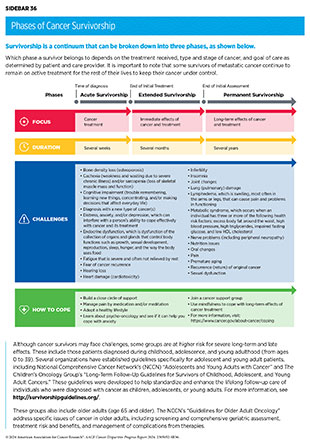
As more people are living longer and fuller lives after a cancer diagnosis, thanks to improved diagnosis and treatment options, greater attention is needed to understand survivorship experiences. These experiences include the physical, psychosocial, and economic adversities caused by a cancer diagnosis. Cancer survivors are at risk for late effects or secondary health problems due to their cancer treatment and therefore require long-term follow-up care, that includes screening for these late effects (see Sidebar 36). Survivorship care should include cancer prevention counseling and assessment for late effects including the increased risk of secondary cancers.
While all survivors of cancer have unique experiences, it is becoming clear that those belonging to medically underserved populations shoulder a disproportionate burden of the adverse effects of cancer survivorship. Understanding the challenges faced by these groups will help inform cancer care strategies and personalized recommendations for those who are more vulnerable, leading to a better quality of life. A cancer diagnosis also impacts family members, caregivers, and friends who are often the main support network for the survivor. This fact necessitates widening the focus of research, support, and care beyond the cancer patient and survivor to include individuals who make up the support system.
The following sections highlight the challenges in health-related quality of life and survivorship faced by cancer survivors and their support network, strategies to improve quality of life, and approaches that have been shown to deliver care most effectively.
Challenges Faced by Cancer Survivors
Cancer survivors often face challenges throughout their survivorship journey (see Sidebar 36). The number of cancer survivors living with a functional limitation, defined as difficulty in performing any of 12 routine physical or social activities without assistance (e.g., sitting for more than 2 hours or participating in social activities), more than doubled from 3.6 million in 1999 to 8.2 million in 2018 (800). The functional limitations can vary based on the type of cancer diagnosed and were highest among survivors of pancreatic (80.3 percent) and lung cancer (76.5 percent) and lowest for those who had melanoma (62.2 percent) or breast (61.8 percent) and prostate cancers (59.5 percent) (800)Patel VR, et al. (2023) JAMA Oncol, 9: 1001. [LINK NOT AVAILABLE].
Physical Challenges
Survivors experience a wide range of short- and long-term symptoms caused by cancer or its treatments (see Sidebar 36) as highlighted in the personal stories of Darlene Pruess and Irasema Partida Chavez. Short-term effects include hair loss, pain, nausea, vomiting, and loss of smell and appetite with varying severity of symptoms, depending on the person, cancer type, and treatment. As cancer survivors are living longer because of better therapies, the development of long-term side effects such as heart damage (cardiotoxicity), lung damage, loss of bone density, and cognitive decline is becoming more common. Increasing evidence shows disparities in both long-term and late effects of cancer treatments in medically underserved populations (see Sidebar 36). As evident from such studies, there are population-specific differences in the rates of cardiovascular complications, lymphedema, peripheral neuropathies, metabolic disorders, diabetes, recurrence of cancer, and development of new, secondary cancers.
Many common cancer treatments damage the cardiovascular system, further exacerbating complications in cancer survivors. Research has shown that cancer survivors have an “excess heart age”—a measure of cardiovascular damage and risk factor for a heart attack—of eight and a half years in men and six and a half years in women compared to those individuals who have never received a cancer diagnosis (801)Scott LC, et al. (2021) MMWR Morb Mortal Wkly Rep, 70: 1. [LINK NOT AVAILABLE]. Average excess heart age was shown to be higher in cancer patients who are NH Black, have low educational attainment, live in rural areas, and have lower income (802)Nielsen S, et al. (2023) Urol Oncol, 41: 429 e15. [LINK NOT AVAILABLE](803)Raisi-Estabragh Z, et al. (2023) Int J Cardiol Cardiovasc Risk Prev, 19: 200218. [LINK NOT AVAILABLE]. Accelerated aging in cancer survivors has also been associated with experiences of racism. Black cancer survivors who experienced major discrimination had higher levels of functional deficits associated with age-related disease (804)Mandelblatt JS, et al. (2023) Cancer, 129: 1557. [LINK NOT AVAILABLE].
Lymphedema results from damage to the lymphatic system after cancer surgery and is a common long-term side effect among survivors of colorectal, endometrial, and breast cancer (806)Zhang X, et al. (2022) JAMA Netw Open, 5: e221671. [LINK NOT AVAILABLE]. Lymphedema disrupts normal draining of the lymphatic fluid, leading to accumulation in the surrounding tissue and resulting in painful swelling, most commonly in the arms and legs (806)Zhang X, et al. (2022) JAMA Netw Open, 5: e221671. [LINK NOT AVAILABLE](807)Hayes SC, et al. (2008) J Clin Oncol, 26: 3536. [LINK NOT AVAILABLE](808)Armer JM, et al. (2019) JAMA Surg, 154: 800. [LINK NOT AVAILABLE]. Research shows that Black and Hispanic women are more likely to develop breast cancer–related lymphedema compared to White women (809)Montagna G, et al. (2022) JAMA Oncol, 8: 1195. [LINK NOT AVAILABLE](810)Ren Y, et al. (2022) Cancer, 128: 4119. [LINK NOT AVAILABLE]. Minoritized populations, who often have limited access to medical resources, including surgery, physical therapy, and medical equipment, coupled with barriers to maintaining a healthy diet and exercising to reduce swelling, are at an increased risk for lymphedema occurrence and severity, and worse quality of life (809)Montagna G, et al. (2022) JAMA Oncol, 8: 1195. [LINK NOT AVAILABLE](810)Ren Y, et al. (2022) Cancer, 128: 4119. [LINK NOT AVAILABLE](811)Rock CL, et al. (2022) CA Cancer J Clin, 72: 230. [LINK NOT AVAILABLE](812)Donahue PMC, et al. (2023) Breast Cancer Res Treat, 200: 1. [LINK NOT AVAILABLE](813)Yedjou CG, et al. (2019) Adv Exp Med Biol, 1152: 31. [LINK NOT AVAILABLE].
As cancer survivors continue to thrive and live longer, their risk of secondary cancers increases. Younger adult cancer survivors are 1.4 to 2 times more likely to develop secondary cancers than older cancer survivors (814)Leung TH, et al. (2023) Cancer Med, 12: 22316. [LINK NOT AVAILABLE]. It is critical to ensure access for survivorship care that can screen for the development of secondary cancers and provide counsel, including cancer prevention and control strategies such as regular exercise, tobacco cessation, and limited alcohol consumption and sunscreen use. According to a recent study, NH Black female breast cancer survivors are at the highest risk of developing secondary cancers among all minority groups (814)Leung TH, et al. (2023) Cancer Med, 12: 22316. [LINK NOT AVAILABLE]. Many factors can contribute to racial and ethnic differences in secondary cancer risk, including geography, cultural differences, language barriers, insurance coverage, genetics, and lifestyle factors (670)Reeder-Hayes KE, et al. (2023) Cancer, 129: 925. [LINK NOT AVAILABLE](759)Mata DA, et al. (2023) N Engl J Med, 388: 281. [LINK NOT AVAILABLE].
Another common side effect related to treatment is chemotherapy-induced peripheral neuropathy (CIPN). CIPN is caused by chemotherapy drugs damaging nerves that control the sensations and movements of the arms, legs, hands, and feet, thus leading to pain; abnormal reflexes, abnormal sensations, such as buzzing or tingling; and inability to control certain bodily functions, such as excessive sweating or loss of bladder control. CIPN is common in Black cancer survivors, with 68 percent of survivors experiencing this side effect (815)Sreeram K, et al. (2023) Cancer Causes Control, 34: 459. [LINK NOT AVAILABLE]. Studies have shown that a lack of vitamin D is associated with increased CIPN. Black individuals in general, and cancer survivors in particular, have higher rates of vitamin D insufficiency, which partially explains the higher rates of CIPN in this population (816)Ames BN, et al. (2021) Nutrients, 13: 499. [LINK NOT AVAILABLE](817)Galsky MD, et al. (2022) J Clin Oncol, 40: TPS4613. [LINK NOT AVAILABLE].
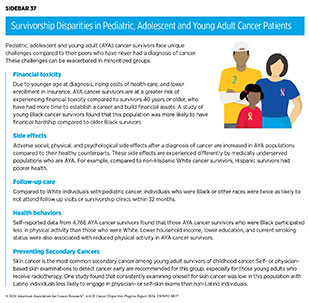
Unique Challenges Faced by Pediatric and Adolescent and Young Adult (AYA) Cancer Survivors
Pediatric cancer survivors are those diagnosed between ages less than 1 year to 14 years, while AYAs are diagnosed between ages 15 and 39 years. With tremendous advances in treatments, 85 percent of AYA and pediatric survivors are alive at least 5 years after diagnosis in 2019 compared to only 58 percent of pediatric and 68 percent of AYA survivors 40 years ago (818)National Cancer Institute. Cancer in children and adolescents. Accessed: June 30, 2022. .
Unique challenges experienced by these groups include greater risk of chronic health problems that arise later in life but are attributable to cancer treatment at a young age, which are termed late effects, employment difficulties, financial toxicities, psychological challenges, secondary cancers, and worse quality of life (819)Erdmann F, et al. (2021) Cancer Epidemiol, 71: 101733. [LINK NOT AVAILABLE]. These challenges are further compounded if pediatric/AYA survivors belong to a racial or ethnic minority or a medically underserved group (see Sidebar 37). To improve long-term follow-up care and optimize quality of life, it is essential to understand how disease burden in these vulnerable patient populations differs by race/ethnicity, sexual orientation and gender identity, and geographic location.
Health-related Quality of Life
Health-related quality of life (HRQOL) offers a comprehensive view of the impact a disease and its treatment can have on a patient’s physical, functional, psychological, social, and financial well-being. Cancer survivors who belong to medically underserved populations are at an elevated risk of worse HRQOL, which has been shown to increase the likelihood of cancer recurrence and mortality (829)Sitlinger A, et al. (2018) Surg Oncol Clin N Am, 27: 675. [LINK NOT AVAILABLE](830)Park J, et al. (2021) Cancer, 127: 1114. [LINK NOT AVAILABLE](831)Eichler M, et al. (2022) Br J Cancer, 126: 1346. [LINK NOT AVAILABLE]. One study found that compared to NH White cancer survivors, survivors who were AI/AN, Cuban, Dominican, and Puerto Rican, as well as those from the Caribbean, were more likely to experience worse HRQOL (832)Reeve BB, et al. (2023) J Natl Cancer Inst, 115: 258. [LINK NOT AVAILABLE]. Lower HRQOL is associated with being unemployed, having other comorbidities, eating an unhealthy diet, and experiencing a high fear of cancer recurrence (833)Manne S, et al. (2023) BMC Cancer, 23: 664. [LINK NOT AVAILABLE].
A diagnosis of cancer can pose serious challenges to a person’s mental and emotional health. Many survivors experience anxiety (7 percent to 10 percent of patients), depression (8 percent to 24 percent of patients), and distress (25 percent to 41 percent of patients) following the completion of cancer treatment (289)American Association for Cancer Research. AACR Cancer Progress Report 2022. Accessed: July 5, 2023. (834)Rincones O, et al. (2021) Cancer Manag Res, 13: 3803. [LINK NOT AVAILABLE](835)Papini C, et al. (2023) Cancer, 129: 1117. [LINK NOT AVAILABLE](836)Chang WH, et al. (2022) Nat Med, 28: 860. [LINK NOT AVAILABLE]. A study in patients with 26 different cancer types found that 98 percent of patients with testicular cancer, 78 percent of patients with cervical cancer, and 69 percent of patients with Hodgkin lymphoma experienced a depressive event (836)Chang WH, et al. (2022) Nat Med, 28: 860. [LINK NOT AVAILABLE]. Many of the adverse influences of SDOH can lead to greater negative mental health outcomes among survivors who experience health disparities. For instance, poor access to mental health care, housing instability, and food insecurity, which are higher in certain populations, can worsen mental health (837)Camacho-Rivera M, et al. (2022) Health Equity, 6: 729. [LINK NOT AVAILABLE](838)Robien K, et al. (2023) J Acad Nutr Diet, 123: 330. [LINK NOT AVAILABLE](839)Katayama ES, et al. (2024) Ann Surg Oncol, 31: 49. [LINK NOT AVAILABLE](840)Robinson JRM, et al. (2023) J Cancer Surviv, DOI: 10.1007/ s11764-023-01471-5. [LINK NOT AVAILABLE](841)Islam JY, et al. (2022) Health Equity, 6: 435. [LINK NOT AVAILABLE](842)Sharareh N, et al. (2024) J Gen Intern Med, 39: 52. [LINK NOT AVAILABLE].
Even when survivors are treated at NCI-designated cancer centers, there are identified gaps and poor access to services for cancer survivors, including those for mental health (843)Reinhart CA, et al. (2020) J Cancer Surviv, 14: 43. [LINK NOT AVAILABLE]. One study of NCI-designated cancer centers found that while main hub hospitals, which are often located in large metropolitan areas, adequately provided services for cancer survivors, including support for treatment side effects, health behavior information, and mental health services, the affiliated satellite locations, which are often located in less dense, rural areas, provided these services less than one-quarter of the time (843)Reinhart CA, et al. (2020) J Cancer Surviv, 14: 43. [LINK NOT AVAILABLE].
AI/AN groups, which are comprised of 574 federally recognized tribes or people groups and are highly diverse communities, experience disparities in cancer survival rates and social and physical quality of life and have the poorest 5-year survival rate from cancer of any racial group (see section on American Indian or Alaska Native (AI/AN) Population) (844)Bastian TD, et al. (2020) JCO Glob Oncol, 6: 161. [LINK NOT AVAILABLE](845)Burhansstipanov L, et al. (2012) J Cancer Educ, 27: S106. [LINK NOT AVAILABLE]. AI/AN cancer survivors have higher spiritual quality of life compared to those who belong to other races and ethnicities. Further, because of the diversity among AI/AN tribal groups, spirituality characteristics are highly individualistic (845)Burhansstipanov L, et al. (2012) J Cancer Educ, 27: S106. [LINK NOT AVAILABLE]. Studies looking at quality of life among American Indian cancer survivors in South Dakota found that spirituality and social support were strong predictors for positive outcomes (846)Lee YS, et al. (2023) J Evid Based Soc Work (2019), 20: 536. [LINK NOT AVAILABLE]. Further research has shown that the best way to support AI/AN cancer survivors is a systematic approach that leverages community strengths and partnerships to support all factors influencing a survivor’s quality of life, including physical, spiritual, mental/emotional, and social aspects (844)Bastian TD, et al. (2020) JCO Glob Oncol, 6: 161. [LINK NOT AVAILABLE]. Researchers must ensure that interventions for Indigenous populations align with the cultural values of cancer survivors from these populations (844)Bastian TD, et al. (2020) JCO Glob Oncol, 6: 161. [LINK NOT AVAILABLE].
Asian cancer survivors are highly diverse, representing a wide range of race and ethnicities (see Sidebar 2). Some segments of this population, however, experience worse HRQOL. Asian survivors are also less likely to be screened for psychological distress by health care providers, compared to survivors from other races and ethnicities (847)Rohan EA, et al. (2022) JCO Oncol Pract, 18: e1704. [LINK NOT AVAILABLE].
Studies of breast, prostate, or colorectal cancer survivors who are Black report poorer quality of life and physical and mental health, compared to cancer survivors who are White (849)Samuel CA, et al. (2016) Breast Cancer Res Treat, 160: 1. [LINK NOT AVAILABLE](850)Pinheiro LC, et al. (2015) Cancer, 121: 1312. [LINK NOT AVAILABLE](851)Claridy MD, et al. (2018) Qual Life Res, 27: 2067. [LINK NOT AVAILABLE](852)Matthews AK, et al. (2012) Cancer Nurs, 35: 355. [LINK NOT AVAILABLE]. One way to improve psychological outcomes among Black cancer survivors is to make use of pyscho-oncologic services, which use health care professionals to address the behavioral, emotional, psychological, and social challenges faced by cancer survivors and their caregivers (853)Lechner SC, et al. (2012) Couns Psychol, 41: 286. [LINK NOT AVAILABLE](854)Whitehead NE, et al. (2015) Psychooncology, 24: 497. [LINK NOT AVAILABLE]. Unfortunately, Black survivors often do not get the psycho-oncological help they need. For instance, one study of Black cancer patients found that Black women were referred to psycho-oncology services only 2 percent of the time compared to 10 percent for White women (855)Aburizik A, et al. (2023) Psychooncology, 32: 933. [LINK NOT AVAILABLE].
Hispanic/Latino cancer survivors experience lower HRQOL and mental health compared to other racial and ethnic groups (856)Samuel CA, et al. (2020) Qual Life Res, 29: 2615. [LINK NOT AVAILABLE]. Mental and HRQOL disparities might be exacerbated due to the fact that Hispanic/Latino survivors are not screened for psychological distress as often as survivors who belong to other racial and ethnic populations (847)Rohan EA, et al. (2022) JCO Oncol Pract, 18: e1704. [LINK NOT AVAILABLE]. Emerging data demonstrate some important strategies to improve mental health among this population. First, positive family functioning (e.g., family cohesiveness) was correlated with higher quality of life, which consequently was associated with lower levels of anxiety, depression, and hopelessness (857)Torres-Blasco N, et al. (2023) Palliat Support Care, 21: 461. [LINK NOT AVAILABLE](858)Carrion IV, et al. (2022) Human Soc Sci Comm, 9: 357. [LINK NOT AVAILABLE]. Evidence shows that the use of culturally appropriate, bilingual interventions was also beneficial in improving psychosocial outcomes for both patients and caregivers who are Hispanic/Latino (859)Guan T, et al. (2023) Front Psychol, 14: 1052229. [LINK NOT AVAILABLE].
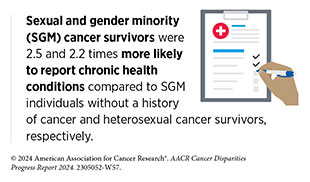
Patients from SGM populations are susceptible to worse psychosocial and HRQOL compared to heterosexual patients (860)Hoyt MA, et al. (2023) J Psychosoc Oncol, 41: 661. [LINK NOT AVAILABLE](861)Schefter A, et al. (2022) Cancer Rep (Hoboken), 5: e1461. [LINK NOT AVAILABLE](862)Hutchcraft ML, et al. (2021) LGBT Health, 8: 68. [LINK NOT AVAILABLE](863)Hart TL, et al. (2014) J Sex Med, 11: 2308. [LINK NOT AVAILABLE]. In part, this can be attributed to lack of trust in health care systems and non-inclusive health care environments experienced by this population across the cancer care continuum. SGM cancer survivors treated at a hospital that had a more inclusive environment were six times more likely to be satisfied with the care they received for their cancer than those who had been treated in an environment that was not welcoming to SGM individuals (864)Kamen CS, et al. (2024) Cancer, 130: 1292. [LINK NOT AVAILABLE]. Those who reported feeling satisfied with their care felt they had improved physical and mental health (864)Kamen CS, et al. (2024) Cancer, 130: 1292. [LINK NOT AVAILABLE](865)Franco-Rocha OY, et al. (2023) Psychooncology, 32: 834. [LINK NOT AVAILABLE].
Financial Toxicity
Financial toxicity refers to the financial hardship associated with cancer treatment and its management. Evidence indicates that cancer survivors who experience financial toxicity, such as difficulty in paying for prescriptions, mental health care, and other health services, and/or who delay medical care due to cost, are also at greater risk of mortality, regardless of insurance status (866)Yabroff KR, et al. (2022) J Natl Cancer Inst, 114: 863. [LINK NOT AVAILABLE].
Financial toxicity is pervasive and is, in part, exacerbated by the rising costs of cancer care (867)Tak HJ, et al. (2023) J Natl Cancer Inst, 115: 239. [LINK NOT AVAILABLE]. For instance, between 2009 and 2016, the average cost of treatment increased 29 percent for breast cancer, 11 percent for lung cancer, and 4 percent for prostate cancer. In addition, out-of-pocket costs have also increased by 15 percent for all patients with cancer (867)Tak HJ, et al. (2023) J Natl Cancer Inst, 115: 239. [LINK NOT AVAILABLE].
The burden of cancer disproportionately affects those who are living in poverty (see section on Populations Living Under Poverty). Additionally, chronic diseases such as cancer have consistent high costs of care that unfairly impact populations from low SES, pushing them deeper into poverty. Low-income Americans have difficulty in paying for cancer care, even when insured. With increasing enrollment of many US workers in high-deductible health insurance plans (868)Centers for Disease Control and Prevention. High-deductible Health Plan Enrollment Among Adults Aged 18–64 With Employment-based Insurance Coverage. Accessed: March 17, 2024. , which offer lower up-front costs in exchange for high deductibles (from $2,500 up to $5,000) (869)Zafar SY (2016) J Natl Cancer Inst, 108: djv370. [LINK NOT AVAILABLE], even insured patients with cancer may struggle with debt related to treatment and follow-up care. In fact, roughly 50 percent of Americans cannot afford to pay for their deductibles (869)Zafar SY (2016) J Natl Cancer Inst, 108: djv370. [LINK NOT AVAILABLE]. Cancer patients who are uninsured are more likely to be Black and Hispanic, and even when insured, Black and Hispanic patients are more likely to experience financial toxicity (875)Ng AP, et al. (2022) Gynecol Oncol, 166: 200. [LINK NOT AVAILABLE]. Unfortunately, the inability to afford treatments or the accumulation of debt leads to an increased likelihood of bankruptcy among cancer survivors.
Low-income cancer survivors also experience worse cancer outcomes because of barriers in maintaining and receiving support after treatment (876)Noel CW, et al. (2023) JAMA Otolaryngol Head Neck Surg, 149: 63. [LINK NOT AVAILABLE](877)White V, et al. (2023) Med J Aust, 219: 28. [LINK NOT AVAILABLE](878)Karim MA, et al. (2022) Cancer Res Commun, 2: 1119. [LINK NOT AVAILABLE]. Patients and survivors who have low income are more likely to miss their appointments. Those who are Black or Latino also have higher odds of missed appointments (715)Chen AM (2023) Front Health Serv, 3: 1288329. [LINK NOT AVAILABLE].
Survivors can face challenges in maintaining a job or going back to a previous job after the conclusion of cancer treatment. This is troubling because having a job decreases the likelihood of financial toxicity and improves HRQOL (879)Andreu Y, et al. (2023) Health Qual Life Outcomes, 21: 44. [LINK NOT AVAILABLE]. Based on a recent study, cancer survivors between the ages of 50 and 64 years were more likely to have a work-limiting disability and less likely to be employed than those without a history of cancer, equating to 505,768 fewer employed individuals between 2010 and 2016 (880)Grabowski DC, et al. (2023) Jama Network Open, 6: e2315823. [LINK NOT AVAILABLE].
Several programs have been shown to mitigate the damaging effects of financial toxicity (see Sidebar 41). Programs that provide monetary assistance to help offset the cost of treatment can help mitigate high out-of-pocket spending (881)Ragavan MV, et al. (2024) JCO Oncol Pract, 20: 291. [LINK NOT AVAILABLE]. However, these programs do not work for those who have extremely high costs associated with their cancer treatment (881)Ragavan MV, et al. (2024) JCO Oncol Pract, 20: 291. [LINK NOT AVAILABLE]. Furthermore, non-White patients and those who speak English as a second language are half as likely to receive financial assistance as White and English-speaking patients, respectively (881)Ragavan MV, et al. (2024) JCO Oncol Pract, 20: 291. [LINK NOT AVAILABLE].
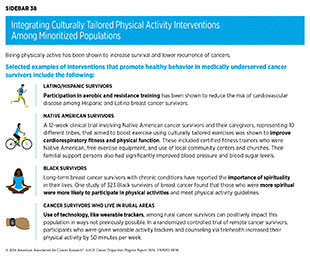
Promoting Healthy Behaviors
Healthy behaviors, such as increasing physical activity, eating a healthy diet, reducing alcohol consumption, and not smoking, can significantly improve both health outcomes and HRQOL for cancer survivors (see Sidebar 38). In fact, it is increasingly appreciated that adopting healthy behaviors after a diagnosis of cancer, but prior to beginning cancer treatment, can significantly improve outcomes for patients (882)Giles C, et al. (2019) BMJ, 366: l5120. [LINK NOT AVAILABLE](883)Molenaar CJL, et al. (2023) JAMA Surg, 158: 572. [LINK NOT AVAILABLE]. A patient who is healthy at the start of treatment can undergo treatment with higher doses of drug, is less susceptible to certain side effects, and has an immune system that is primed to fight cancer better (884)Loewen I, et al. (2021) J Otolaryngol Head Neck Surg, 50: 2. [LINK NOT AVAILABLE].
Many of the barriers to participating in healthy behaviors discussed earlier (see Disparities in the Burden of Preventable Cancer Risk Factors) also exist for cancer survivors. Lack of access to exercise facilities and other types of recreational activity for racially and ethnically minoritized and medically underserved cancer survivors reduces participation in physical activity (885)Conderino SE, et al. (2021) Am J Prev Med, 61: 394. [LINK NOT AVAILABLE]. As one example, rural cancer survivors who had low access to fitness facilities and outdoor space for activities (like biking trails) were less active and did not participate in physical activity compared to those who did have access (886)Stevens CJ, et al. (2023) J Natl Cancer Inst Monogr, 2023: 125. [LINK NOT AVAILABLE].
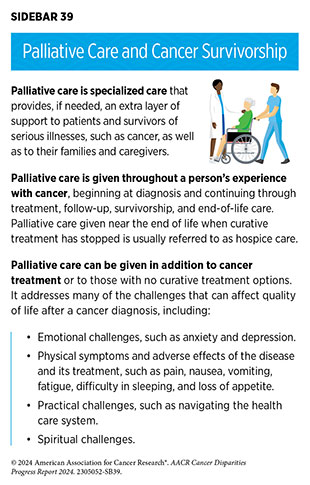
Integrating Palliative Care
Palliative care is an approach to prevent or treat the symptoms and side effects of any disease, including cancer, by addressing the physical, psychological, financial, social, and spiritual needs that arise from the disease and associated treatments (see Sidebar 39). Palliative care is facilitated by a multidisciplinary team of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers and has been shown to improve quality of life for patients, families, and caregivers (887)Radbruch L, et al. (2020) J Pain Symptom Manage, 60: 754. [LINK NOT AVAILABLE].
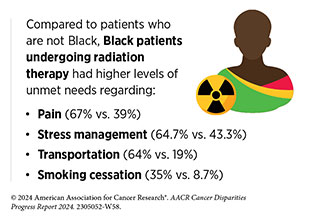
Despite the advantages of palliative care, there are disparities (888,889) in and barriers to utilization by racial and ethnic minorities (890)Khullar K, et al. (2022) BMJ Support Palliat Care., SGM populations (891)van Klinken M, et al. (2023) Semin Oncol Nurs, 39: 151500. [LINK NOT AVAILABLE](892)Haviland K, et al. (2021) Health Soc Care Community, 29: 305. [LINK NOT AVAILABLE], and those living in geographically remote areas (893,894). As one example, in a survey of nurses, physicians, social workers, and chaplains, 23 percent observed discriminatory care to transgender patients with cancer (895)Berkman C, et al. (2024) Palliat Support Care, 22: 3. [LINK NOT AVAILABLE].
Improving Mental Health
The psychological challenges faced by survivors of cancer necessitate approaches that improve the mental well-being of this population. There are several approaches that can be utilized, including mind-body interventions, support groups, improved mental health screening, physical activity, and community engagement (896)Liska TM, et al. (2020) Health Qual Life Outcomes, 18: 197. [LINK NOT AVAILABLE](897)Shani P, et al. (2022) Integr Cancer Ther, 21: 15347354221103275. [LINK NOT AVAILABLE](898)Smith SK, et al. (2018) Am Soc Clin Oncol Educ Book, 38: 813. [LINK NOT AVAILABLE](899)Flores NJ, et al. (2021) Cureus, 13: e14158. [LINK NOT AVAILABLE].
In one meta-analysis that analyzed mind-body exercises (e.g., meditation, yoga) in Black individuals found that these exercises are viewed as acceptable ways to improve quality of life, pain interference, fatigue, anxiety, depression, and physical health among participants (897)Shani P, et al. (2022) Integr Cancer Ther, 21: 15347354221103275. [LINK NOT AVAILABLE]. Unfortunately, these interventions can be inaccessible for the Black population due to cost or geographic location (897)Shani P, et al. (2022) Integr Cancer Ther, 21: 15347354221103275. [LINK NOT AVAILABLE].
Research shows that a cancer diagnosis can promote “post-traumatic growth,” which describes the positive life changes that can develop from traumatic, stressful experiences, such as a diagnosis of cancer (see Sidebar 40). Posttraumatic growth may lead to perceptions of new possibilities, closer relationships with family and friends, development of personal strength, spiritual development, and a greater appreciation for life. Although the concept of posttraumatic growth is not new, its potential is just beginning to be appreciated within the cancer care community.
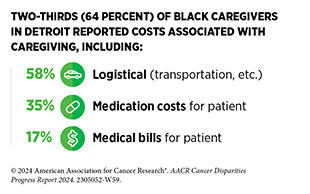
Supporting Caregivers
Caregivers comprise family members or friends who help patients with long-term chronic illness and manage any and all aspects of their care. One in five US adults (ages 18 to 64), accounting for over 53 million people, provided care for another person in 2020, a significant increase from 43.5 million in 2015 (904)National Partnership for Women and Families. Paid Leave Could Keep More Than 6 Million Caregivers Connected to the Labor Force by 2030. Accessed: March 26, 2024. . It is further estimated that four million of these caregivers are caring for an adult cancer patient. More evidence of the challenges faced by caregivers is becoming clear, and there are many opportunities to assist this vulnerable population.
Survivors require many resources that are often provided by their caregivers, including arranging transportation, helping with day-to-day activities such as doctor visits, providing medical care or other clinical tasks, coordinating care, and giving emotional support. This support often leads to caregivers deferring their own health care. One report shows that caregivers who are actively taking care of a family member are less likely to seek medical care, including physician and emergency room visits. Caregivers of individuals with cancer also had an elevated risk of cardiovascular disease (905)Lee LJ, et al. (2022) Stress, 25: 258. [LINK NOT AVAILABLE]. This is especially concerning among Black and Hispanic caregivers, who spend more time caregiving compared to their White counterparts, potentially exacerbating health disparities in these communities (906)Fenton A, et al. (2022) Support Care Cancer, 30: 9625. [LINK NOT AVAILABLE].
Caregivers are also susceptible to financial toxicity, and this is prevalent among those who support individuals with cancer. These caregivers often delay their own care as cost-related coping mechanisms. These coping mechanisms are more common among those who are poor and lack health insurance. Among a survey of nearly 1,000 African American caregivers in Detroit, 52 percent experienced financial toxicity (907)Hastert TA, et al. (2024) J Cancer Surviv, 18: 565. [LINK NOT AVAILABLE]. Similarly, Hispanic caregivers of children with cancer reported having household material hardship and financial toxicity nearly twice as often as NH White and Asian caregivers (908)Evans EM, et al. (2023) Pediatr Blood Cancer: e30496. [LINK NOT AVAILABLE].
Paving the Way for Health Equity in Cancer Survivorship
The disparities in various aspects of cancer survivorship as highlighted in this section necessitate a comprehensive multidisciplinary approach to address the deficiencies experienced by medically underserved groups. It is imperative that researchers, health care systems, professional organizations, insurance groups, and care teams work together to meet the specific needs of the community and the patient.
Community-centered approaches are required to better understand the challenges faced by cancer survivors who belong to racial and ethnic minority groups and medically underserved populations (909)Patel MI, et al. (2024) J Clin Oncol, 42: 518. [LINK NOT AVAILABLE]. Patient advocates are uniquely positioned to bridge a critical gap between survivors and researchers. Patient advocates have immense influence within their communities because they understand the unique needs and challenges within the community; partnering with patient advocates can help inform research questions and clinical study designs. Patient advocates can also help disseminate new information gleaned from research studies into the community so that it is readily accessible and favorably received.
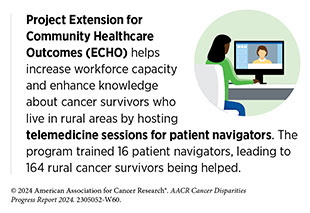
Patient navigators are individuals dedicated to assisting patients with cancer, survivors, family, and caregivers by facilitating and navigating through the health care system for access to timely and quality care. Utilization of patient navigation has been shown to benefit patients across the cancer care continuum, especially in medically underserved population groups, and to reduce the overall costs associated with cancer (see Sidebar 41). In 2024, in response to the White House’s Cancer Moonshot Initiative, seven leading health insurance companies committed to expanding coverage to patient navigation services for cancer patients and those with other serious illnesses, which were previously not covered by insurance. The expanded coverage includes covering and reimbursing navigation services, capturing utilization of navigation services across patient demographics, and tracking health outcomes of patients who utilize patient navigation services. Additionally, these insurance providers have committed to supporting standardization of patient navigation services to align with the Oncology Navigation Standards of Professional Practice, which sets out knowledge and practices navigators should provide in order to deliver standardized, high-quality services. Finally, these health plans have pledged to educate providers, including payers and cancer centers, which service millions of Americans, on how to cover these navigation services (910)The White House. FACT SHEET: Biden Cancer Moonshot Announces Commitments from Leading Health Insurers and Oncology Providers to Make Navigation Services Accessible to More than 150 Million Americans. Accessed April 24, 2024. .
In the wake of the COVID-19 pandemic, there was increased reliance on the use of telehealth, which uses digital information and communication technologies to access health care services remotely and manage a patient’s health care. Utilization of telehealth services among cancer survivors in rural settings increased by 70 percent compared to pre-pandemic levels (912)Lewis-Thames M, et al. (2023) Innov Aging, 7: 228. [LINK NOT AVAILABLE]. Telehealth has helped cancer patients in rural settings receive survivorship care and patient navigation services (913)Morris BB, et al. (2022) J Rural Health, 38: 493. [LINK NOT AVAILABLE](914)Thota R, et al. (2020) JCO Oncol Pract, 16: e557. [LINK NOT AVAILABLE]; however, utilization among rural survivors is still much lower than among cancer survivors who live in urban settings and are closer to major hospital centers (915)Lee MJ, et al. (2023) J Clin Oncol, 41: e13686. [LINK NOT AVAILABLE]. Further investigation into how to best utilize telehealth strategies among rural cancer survivors is warranted to help bring these essential services to this vulnerable population.
A key to charting an equitable path forward for cancer survivors who belong to medically underserved populations is the use of community-based, tailored solutions that meet the specific needs of every patient and include patient advocates and patient navigators as key partners. Such approaches will help implement strategies that address the specific social, psychological, medical, and physical needs of the patient while tying in cultural norms and perceptions, ultimately increasing quality of life, bolstering adherence to follow-up care, identifying financial concerns, providing equitable health care, and reducing the overall cost of cancer care (920)Edward JS, et al. (2023) JCO Oncol Pract, 19: e696. [LINK NOT AVAILABLE](921)Walls M, et al. (2021) Front Public Health, 9: 788285. [LINK NOT AVAILABLE](922)Smith GL, et al. (2022) CA Cancer J Clin, 72: 437. [LINK NOT AVAILABLE].
Next Section: Overcoming Cancer Disparities Through Diversity in Cancer Training and Workforce Previous Section: Disparities in Clinical Research and Cancer Treatment