- Eliminate Tobacco Use
- Maintain a Healthy Weight, Eat a Healthy Diet, Stay Active, and Avoid Sedentary Behavior
- Limit Alcohol Consumption
- Protect Skin from UV Exposure
- Prevent and Eliminate Infection with Cancer-causing Pathogens
- Be Cognizant of Reproductive and Hormonal Influences
- Limit Exposure to Environmental Carcinogens
Preventing Cancer: Identifying Risk Factors
In this section, you will learn:
- In the United States, four out of 10 cancer cases and almost half of all cancer-related deaths are associated with preventable risk factors.
- Tobacco use is the leading preventable cause of cancer.
- Nearly 20 percent of U.S. cancer diagnoses are related to excess body weight, alcohol, poor diet, and physical inactivity.
- Many cases of skin cancer could be prevented by protecting the skin from ultraviolet radiation from the sun and indoor tanning devices.
- Nearly all cases of cervical cancer could be prevented by HPV vaccination, but 46 percent of U.S. adolescents have not received the recommended doses of the vaccine.
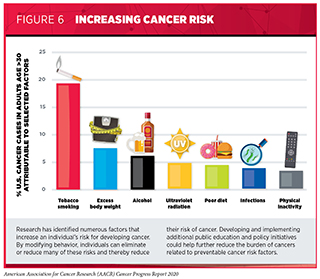
Thanks to decades of research, we have identified several factors that increase a person’s risk of developing and/or dying from cancer. Given that several of these risk factors such as smoking, excess body weight, unhealthy diet, exposure to ultraviolet (UV) radiation, and infection with certain pathogens can be avoided, many cases of cancer could potentially be prevented (see Figure 6). Researchers estimate that more than 40 percent of the cancer cases diagnosed in the United States in 2014 and nearly half of all deaths from cancer were caused by one or more of these potentially avoidable cancer risk factors (110)Islami F, Sauer AG, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin [Internet]. 2017;68:31–54..
Many cancer risk factors are also associated with other chronic diseases, such as cardiovascular disease, respiratory diseases, and diabetes. Thus, public education and policy initiatives to reduce or eliminate exposure to potentially modifiable cancer risk factors have the potential to reduce the burden of several other diseases in addition to cancer. In fact, according to a recent report, middle-aged individuals (50 years old) who adhere to a low-risk, healthy lifestyle by never smoking, eating healthily, staying active, maintaining a healthy weight, and limiting alcohol consumption have a more than five years higher life expectancy free of major chronic diseases such as diabetes, cardiovascular diseases, and cancer compared with those who do not adopt such low-risk behaviors (111)Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ [Internet]. British Medical Journal Publishing Group; 2020 [cited 2020 Jun 30];368..
Unfortunately, federal support of cancer prevention research evaluating the leading risk factors of U.S. mortality and morbidity is seriously inadequate relative to the negative impact of these factors in the United States (112). Therefore, it is imperative that support for prevention research testing randomized interventions, especially those addressing multiple risk factors or causes, should become a national priority.
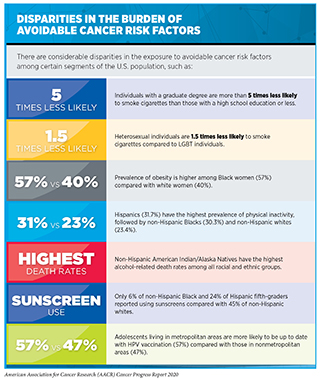
Another critical issue hindering improvement in public health is our inability to effectively communicate the current knowledge on avoidable cancer risk factors to the general population. According to some recent surveys, many individuals both in the United States and across the globe are still unaware of the significant cancer risks associated with obesity, physical inactivity, and alcohol use (113)For P, Society A, Clinical OF. Prepared for American Society of Clinical Oncology National Cancer Opinion Survey. Natl Cancer Opin Surv Harris Poll behalf ASCO, 2017 [Internet]. 2017;(114)International Public Opinion Survey on Cancer. 2020;44.. This emphasizes the continued need for widespread dissemination of our current knowledge of cancer risk factors, as well as the implementation of known preventive strategies to reduce risky behaviors. Targeted efforts are also needed for certain segments of the U.S. population, such as racial and ethnic minorities, and other underserved groups who are disproportionately exposed to many of the potentially avoidable risk factors and have not benefited equally from the existing cancer prevention and control interventions (115) (see sidebar on Disparities in the Burden of Avoidable Cancer Risk Factors). Future interventions that are evidence-based, sustainable, targeted, and culturally tailored need to be implemented to benefit communities with the greatest need, thereby ensuring improved health outcomes for all Americans.
Eliminate Tobacco Use
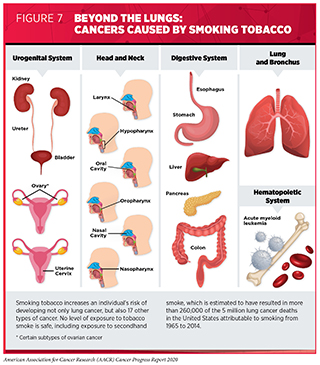
Tobacco use is the leading preventable cause of cancer because it exposes individuals to many harmful chemicals that damage DNA, causing genetic and epigenetic alterations that lead to cancer development (122)Barrow TM, Klett H, Toth R, Böhm J, Gigic B, Habermann N, et al. Smoking is associated with hypermethylation of the APC 1A promoter in colorectal cancer: the ColoCare Study. J Pathol [Internet]. 2017 [cited 2018 Mar 15];243:366–75.(123)Vaz M, Hwang SY, Kagiampakis I, Phallen J, Patil A, O’Hagan HM, et al. Chronic Cigarette Smoke-Induced Epigenomic Changes Precede Sensitization of Bronchial Epithelial Cells to Single-Step Transformation by KRAS Mutations. Cancer Cell [Internet]. 2017 [cited 2018 Mar 15];32:360-376.e6.(124). Smoking tobacco has been shown to increase the risk of developing 17 different types of cancer in addition to lung cancer (see Figure 7). Fortunately, quitting at any age can reduce these risks. Researchers have found that quitting smoking allows new, healthy cells to actively replenish the damaged cells in the lining of our airways leading to a protective effect against lung cancer (125)Yoshida K, Gowers KHC, Lee-Six H, Chandrasekharan DP, Coorens T, Maughan EF, et al. Tobacco smoking and somatic mutations in human bronchial epithelium. Nature [Internet]. Nature Publishing Group; 2020 [cited 2020 Jun 30];578:266–72.. According to a recent report from the U.S. Surgeon General, smoking cessation reduces risk for many adverse health effects in addition to reducing risks from cancer, including cardiovascular diseases and chronic obstructive pulmonary disease (COPD) among others (126). In fact, quitting smoking can reduce the risk of premature death and add up to a decade to life expectancy. In addition to its health benefits, smoking cessation can also reduce the substantial financial burden on smokers and the health care system.
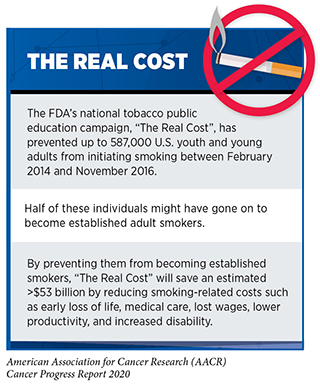
Thanks to the implementation of nationwide comprehensive tobacco control initiatives, cigarette smoking among U.S. adults has been declining steadily. In 2018, which is the most recent year for which data are available, 13.7 percent of U.S. adults ages 18 and older smoked cigarettes, which is the lowest prevalence recorded since 1965 (116). Exposure to secondhand smoke, which increases the risk of lung cancer among nonsmokers, has also dropped substantially over the past three decades (127)Tsai J, Homa DM, Gentzke AS, Mahoney M, Sharapova SR, Sosnoff CS, et al. Exposure to Secondhand Smoke Among Nonsmokers — United States, 1988–2014. MMWR Morb Mortal Wkly Rep [Internet]. 2018;67:1342–6.. Notably, 95 percent of adults who smoke report trying their first cigarette before the age of 21. Therefore, preventing or delaying the initiation of tobacco product use among youth and young adults may have a significant positive impact on smoking-related health outcomes (128)Bonnie RJ, Stratton K, Kwan LY, editors. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products [Internet]. Washington, D.C.: National Academies Press; 2015 [cited 2019 May 21].. It is also encouraging that initiation of tobacco products, including cigarettes, has been declining among youth and young adults with a significantly lower percentage of individuals ages 12 to 24 reporting smoking initiation in 2018 compared with 2008 (129)Cancer Trends Progress Report National Cancer Institute, NIH, DHHS, Bethesda, MD, March 2020, https://progressreport.cancer.gov. [Internet]. [cited 2020 Jun 30].. To further accelerate this progress against tobacco use among youth and young adults a new policy was implemented on December 20, 2019, when the U.S. Congress signed legislation amending the Federal Food, Drug, and Cosmetic Act, and raising the federal minimum age of sale of all tobacco products from 18 to 21 years (130)Tobacco 21 | FDA [Internet]. [cited 2020 Jun 30]..
Despite these positive trends we cannot overlook the fact that in the United States more than 49 million adults and nearly 11 million youth and young adults reported using a tobacco product in 2018 and 2019, respectively (116)(132)TW W, AS G, MR C, KA C, E H-H, MD S, et al. Tobacco Product Use and Associated Factors Among Middle and High School Students – United States, 2019. MMWR Surveill Summ [Internet]. MMWR Surveill Summ; 2019 [cited 2020 Jun 30];68.. In addition, according to recent estimates around 58 million nonsmokers, including 14 million children ages 3 to 11 years, were exposed to secondhand smoke between 2013 and 2014 (127)Tsai J, Homa DM, Gentzke AS, Mahoney M, Sharapova SR, Sosnoff CS, et al. Exposure to Secondhand Smoke Among Nonsmokers — United States, 1988–2014. MMWR Morb Mortal Wkly Rep [Internet]. 2018;67:1342–6.. There are striking sociodemographic disparities in the use of tobacco products as well as secondhand smoke exposure. For instance, tobacco use is higher among non-Hispanic American Indian/Alaska Native adults compared with other racial or ethnic groups, among residents of the Midwest or southern United States compared with the rest of the country, among individuals with lower levels of household income, among adults who were uninsured, and among individuals with disabilities or serious psychological distress (116).
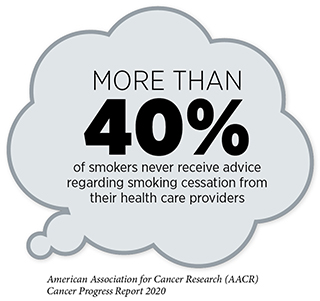
It is imperative that all stakeholders continue to work together to identify evidence-based, population-level interventions such as tobacco price increases, public health campaigns, age and marketing restrictions, cessation counseling and medications, and smoke-free laws to reduce smoking rates and smoking-related cancer burden in the United States. Two recent reports indicate that innovative interventions offered in unique clinical settings, such as the Emergency Department while patients present with semi-urgent or non-urgent treatments, or at pediatricians’ offices while parents are visiting with their child’s doctor, can be effective in increasing smoking cessation among adults (133)WHC L, KY H, MP W, DYT C, KKW L, W X, et al. Effectiveness of a Brief Self-determination Theory-Based Smoking Cessation Intervention for Smokers at Emergency Departments in Hong Kong: A Randomized Clinical Trial. JAMA Intern Med [Internet]. JAMA Intern Med; 2019 [cited 2020 Jun 30];180.(134)E N-B, JE D, B HW, NA R, DJ O, DE L, et al. Treating Parents for Tobacco Use in the Pediatric Setting: The Clinical Effort Against Secondhand Smoke Exposure Cluster Randomized Clinical Trial. JAMA Pediatr [Internet]. JAMA Pediatr; 2019 [cited 2020 Jun 30];173.. These findings are important since each year over half of adult smokers try to quit smoking but less than 10 percent are successful (126). Notably, FDA-approved therapeutics and behavioral counseling have both been shown to improve the chances of quitting and using them together can double the odds of quitting successfully (126).
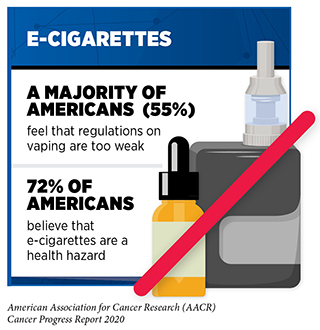
The use of other combustible tobacco products (for example, cigars), smokeless tobacco products (for example, chewing tobacco and snuff), and waterpipes (hookahs) is also associated with adverse health outcomes including cancer (135)Christensen CH, Rostron B, Cosgrove C, Altekruse SF, Hartman AM, Gibson JT, et al. Association of Cigarette, Cigar, and Pipe Use With Mortality Risk in the US Population. JAMA Intern Med [Internet]. American Medical Association; 2018 [cited 2018 May 4];178:469.. Electronic cigarettes (e-cigarettes) are a rapidly emerging tobacco product. An alarming trend in recent years is the growing popularity of e-cigarettes among U.S. youth and young adults. E-cigarettes were first introduced to the U.S. market in 2007, and since 2014 they have been the most commonly used tobacco product among U.S. middle and high school students (136) (see sidebar on E-Cigarettes: What Have We Learned and What Do We Need to Know?).
E-cigarettes come in flavors that appeal to youth and young adults and deliver very high levels of nicotine, an extremely addictive substance that is harmful to the developing brain (153). The continued surge in e-cigarette use among this vulnerable population has been an ongoing public health challenge. Not only is the percentage of current users increasing every year, but recent data also indicate that more e-cigarette users are starting to use these products at a younger age (154)Vallone DM, Cuccia AF, Briggs J, Xiao H, Schillo BA, Hair EC. Electronic Cigarette and JUUL Use Among Adolescents and Young Adults. JAMA Pediatr [Internet]. American Medical Association; 2020 [cited 2020 Jun 30];174:277.(140)Cullen KA, Gentzke AS, Sawdey MD, Chang JT, Anic GM, Wang TW, et al. e-Cigarette Use Among Youth in the United States, 2019. JAMA [Internet]. American Medical Association; 2019 [cited 2020 Jun 30];322:2095.(155)Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends in Adolescent Vaping, 2017–2019. N Engl J Med [Internet]. Massachusetts Medical Society; 2019 [cited 2020 Jun 30];381:1490–1.. The percentage of youth who had used their first e-cigarette by age 14 increased from 8.8% in 2014 to 28.6% in 2018 (156)Evans-Polce R, Veliz P, Boyd CJ, McCabe V V., McCabe SE. Trends in E-Cigarette, Cigarette, Cigar, and Smokeless Tobacco Use Among US Adolescent Cohorts, 2014–2018. Am J Public Health [Internet]. American Public Health Association; 2020 [cited 2020 Jun 30];110:163–5.. Exposure to secondhand aerosol (SHA) from e-cigarettes can expose nonusers to potentially harmful substances including nicotine, carbonyl compounds, tobacco-specific nitrosamines, heavy metals, and glycols. Concurrent with the recent surge in e-cigarette use among U.S. youth and young adults, there has also been an increase in SHA exposure among U.S. middle and high school students (157)Dai H. Exposure to Secondhand Aerosol From Electronic Cigarettes Among US Youth From 2015 to 2018. JAMA Pediatr [Internet]. American Medical Association; 2020 [cited 2020 Jun 30];174:298.. This is especially concerning since individuals who are exposed to SHA are more susceptible to using e-cigarettes or cigarettes later in life (157)Dai H. Exposure to Secondhand Aerosol From Electronic Cigarettes Among US Youth From 2015 to 2018. JAMA Pediatr [Internet]. American Medical Association; 2020 [cited 2020 Jun 30];174:298..
The availability of kid-friendly flavors, exposure to product marketing, and misperceptions about harm are some of the reasons behind the continued use of e-cigarettes among youth and young adults. In fact, according to a 2019 national survey, 20 percent of young adults in the U.S. perceived e-cigarettes as “harmless” (158). While a more recent survey from the U.K. suggests an increase in the proportion of adults age 16 and older who perceive e-cigarettes as harmful, post–EVALI outbreak, whether the same holds true in the U.S. and whether such change in perception leads to a long-term change in e-cigarette use among youth and young adults remains to be evaluated (159)Tattan-Birch H, Brown J, Shahab L, Jackson SE. Association of the US Outbreak of Vaping-Associated Lung Injury With Perceived Harm of e-Cigarettes Compared With Cigarettes. JAMA Netw Open [Internet]. American Medical Association; 2020 [cited 2020 Jun 30];3:e206981..
For the most part, efforts to limit the rapid spread of e-cigarette use among youth and young adults have been inadequate. In December 2018, the Office of the U.S. Surgeon General issued an advisory declaring e-cigarette use in youth an epidemic, and since then the FDA, the federal government, and many local governments have proposed several restrictions on e-cigarettes including bans on certain flavors to curb youth appeal (see Supporting Public Health Policies to Reduce the Use of Tobacco Products). It is imperative that all stakeholders continue to work together to determine the long-term health outcomes associated with e-cigarettes and identify new and effective strategies to implement population-level regulations to reduce e-cigarette use among youth and young adults.
Maintain a Healthy Weight, Eat a Healthy Diet, Stay Active, and Avoid Sedentary Behavior
Nearly 20 percent of new cancer cases and 16 percent of cancer deaths in U.S. adults are attributable to a combination of being overweight or obese, poor diet, physical inactivity, and excessive alcohol consumption (110)Islami F, Sauer AG, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin [Internet]. 2017;68:31–54.. Being overweight or obese as an adult increases a person’s risk for 15 types of cancer whereas being physically active reduces risk for nine types of cancer (see Figure 8). Therefore, maintaining a healthy weight, being physically active, avoiding sedentary behavior, and consuming a balanced diet are effective ways a person can lower the risk of developing or dying from cancer (see sidebar on Reduce Your Risk for Cancer by Maintaining a Healthy Weight, Being Physically Active, and Consuming a Balanced Diet). Identifying the ways by which obesity, unhealthy diet, and physical inactivity increase cancer risk and quantifying the magnitude of such risks are areas of active research investigation (161)Mariosa D, Carreras-Torres R, Martin RM, Johansson M, Brennan P. Commentary: What can Mendelian randomization tell us about causes of cancer? Int J Epidemiol [Internet]. Oxford Academic; 2019 [cited 2020 Jul 1];48:816–21..
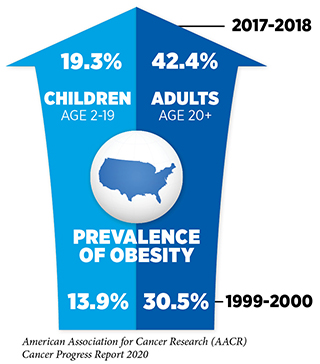
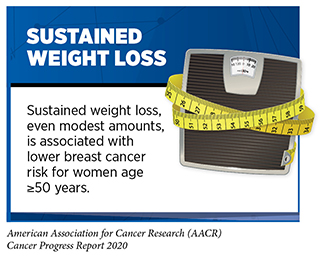
In 2014, an estimated seven and eight percent of all U.S. cancer cases and deaths, respectively, were attributable to excess body weight. Beyond cancer, obesity increases the risk of developing several other health problems including type 2 diabetes, high blood pressure, heart disease, stroke, liver disease, and kidney disease (169)Harrison R. The State of Obesity: 2019. 1905;10:1055.. Therefore, it is concerning that in the U.S. and around the globe the prevalence of obesity has been rising steadily. In the United States, 42 percent of adults age 20 and older were obese in 2018, and according to a recent projection, by the year 2030, nearly 50 percent of all U.S. adults age 18 and older will have obesity (117)Craig M. Hales, M.D., Margaret D. Carroll, M.S.P.H., Cheryl D. Fryar, M.S.P.H., and Cynthia L. Ogden PD. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief [Internet]. 2020;1–8.(170)Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med [Internet]. Massachusetts Medical Society; 2019 [cited 2020 Jul 1];381:2440–50.. An area of particular concern is childhood obesity, since for many children excess body weight extends into adulthood and increases the risk of adverse health outcomes (171)Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N Engl J Med [Internet]. Massachusetts Medical Society; 2018 [cited 2019 May 28];379:1303–12.(172)Levi Z, Rottenberg Y, Twig G, Katz L, Leiba A, Derazne E, et al. Adolescent overweight and obesity and the risk for pancreatic cancer among men and women: a nationwide study of 1.79 million Israeli adolescents. Cancer [Internet]. John Wiley & Sons, Ltd; 2019 [cited 2019 May 28];125:118–26.(173)Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL, et al. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N Engl J Med [Internet]. 2017;377:2145–53.. In 2018, nearly 20 percent of children ages 2 to 19 years were obese (174). Concurrent with the steady rise in obesity rates in the United States, the incidence of several obesity-associated cancers has also been rising at an alarming rate, especially among young adults (175)(176)Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Heal [Internet]. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY 4.0 license; 2019;0:1–11.. While further research is needed to elucidate whether weight loss can effectively mitigate cancer risks and curb these emerging trends, intervention to reduce obesity is certainly a top priority in public health.
Complex and interrelated factors ranging from socioeconomic, environmental, and biological to individual lifestyle factors contribute to obesity. There is, however, sufficient evidence that consumption of high-calorie, energy-dense food and beverages and insufficient physical activity play a significant role (169)Harrison R. The State of Obesity: 2019. 1905;10:1055.. In the United States, more than 5 percent of all newly diagnosed cancer cases among adults are attributable to eating a poor diet (179)Zhang FF, Cudhea F, Shan Z, Michaud DS, Imamura F, Eom H, et al. Preventable Cancer Burden Associated with Poor Diet in the United States. JNCI Cancer Spectr [Internet]. 2019 [cited 2019 Jun 19];. Low intake of healthy foods such as whole grains, fruits, nuts, and seeds combined with high consumption of unhealthy foods such as sugar-sweetened drinks and high levels of red and processed meats are, in fact, responsible for one in five deaths globally (180)Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet [Internet]. 2019;6736..
Intensive efforts by all stakeholders are needed if we are to increase the number of people who consume a balanced diet, such as that recommended by the U.S. Department of Health and Human Services and the U.S. Department of Agriculture in the 2015—2020 Dietary Guidelines for Americans (181). Unfortunately, the burden of many diet-related diseases, including cancer, is disparately high in low-income neighborhoods lacking access to healthy food retailers such as supermarkets, while having an overabundance of convenience stores with unhealthy and fast food options (169)Harrison R. The State of Obesity: 2019. 1905;10:1055.. One initiative that has been effective in increasing the consumption of healthy food and lowering the rates of obesity among children from low-income families is the Special Supplemental Nutrition Program for Women Infants and Children (WIC) (182)Daepp MIG, Gortmaker SL, Wang YC, Long MW, Kenney EL. WIC Food Package Changes: Trends in Childhood Obesity Prevalence. Pediatrics [Internet]. 2019 [cited 2019 Jun 19];143:e20182841.. Data from more than 12 million children ages 2 to 4 whose families are enrolled in the WIC program show that obesity rates declined from 16 percent in 2010 to less than 14 percent in 2016. A potential factor that may have contributed is the consumption of more fruit, vegetables, and whole wheat products which are made available through this program (183). Initiatives such as WIC are extremely important given that obesity during early childhood is associated with sustained overweight or obesity in adolescence or adulthood and that obesity during adolescence can increase the risk of developing cancer later in life.
Evidence-based public policies can play an important role in promoting healthy dietary habits. In this regard, the FDA recently began requiring food manufacturers to display updated nutrition labels on their product packaging. These labels must include information on added sugars and display calories and serving sizes in bolder and larger type (184). Another approach proposed in a recent report suggests that labeling food and beverages with information on how much exercise it would require to burn off its caloric content might be an effective way of encouraging people to make healthier food choices (185)Daley AJ, McGee E, Bayliss S, Coombe A, Parretti HM. Effects of physical activity calorie equivalent food labelling to reduce food selection and consumption: systematic review and meta-analysis of randomised controlled studies. J Epidemiol Community Heal [Internet]. BMJ Publishing Group Ltd; 2020 [cited 2020 Jul 1];74:269–75.. Yet another public policy aimed at reducing obesity is the introduction of taxes on sugar-sweetened beverages (SSBs) in several local jurisdictions in the United States (186). SSBs are a major contributor to caloric intake among U.S. youth and adults (187)Rosiner A, Herrick K, Gahche JJ, Park S, Kumar G, Pan L, et al. Sugar-sweetened beverage consumption among adults-18 States, 2012. Morb Mortal Wkly Rep [Internet]. 2014;63:686–90.(188)Rosiner A, Herrick K, Gahche JJ, Park S. Sugar-sweetened Beverage Consumption Among U.S. Youth, 2011–2014. NCHS Data Brief [Internet]. 2017;1–7.. Thus, it is encouraging that since the implementation of taxes on SSBs, there are already some indications of reduction in consumption, in several cities within the U.S. and in some cases in lower-income, racially and ethnically diverse neighborhoods (189)Powell LM, Leider J, Léger PT. The Impact of a Sweetened Beverage Tax on Beverage Volume Sold in Cook County, Illinois, and Its Border Area. Ann Intern Med [Internet]. 2020 [cited 2020 Jul 1];172:390.(190)(191). Interestingly, according to two recent reports, taxing the amount of sugar in an SSB instead of the volume of the beverage could generate significantly greater health and economic benefits (192)AH G, BB L, D T, H A. Designing Better Sugary Drink Taxes. Science [Internet]. Science; 2019 [cited 2020 Jul 1];365.(193)Y L, D M, S S, J L, PE W, M M, et al. Health Impact and Cost-Effectiveness of Volume, Tiered, and Absolute Sugar Content SugarSweetened Beverage Tax Policies in the United States: A Microsimulation Study. Circulation [Internet]. Circulation; 2020 [cited 2020 Jul 1];. Continued research is necessary to identify the optimal approaches to regulating food and nutrition that maximize health benefits and to evaluate the long-term effects of these policies on obesity and obesity-related health outcomes such as cancer.
Three percent of overall cancer cases in the United States can be attributed to physical inactivity (110)Islami F, Sauer AG, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin [Internet]. 2017;68:31–54.. According to a recent report, being sedentary (inactive) for 13 or more hours per day can increase the risk of dying from cancer by 82 percent (194)Gilchrist SC, Howard VJ, Akinyemiju T, Judd SE, Cushman M, Hooker SP, et al. Association of Sedentary Behavior With Cancer Mortality in Middle-aged and Older US Adults. JAMA Oncol [Internet]. 2020 [cited 2020 Jul 1];. Engaging in recommended amounts of physical activity can lower the risks for developing nine types of cancer (see Figure 8 and sidebar on Physical Activity Guidelines), and in fact there is emerging evidence that there may be risk reduction for even more cancer types (165)(167)(166). Physical activity also reduces the risk of dying from cancer. For example, research shows that replacing just 30 minutes of sedentary behavior with a moderately intense physical activity such as biking can reduce the risk of dying from cancer by 30 percent (194)Gilchrist SC, Howard VJ, Akinyemiju T, Judd SE, Cushman M, Hooker SP, et al. Association of Sedentary Behavior With Cancer Mortality in Middle-aged and Older US Adults. JAMA Oncol [Internet]. 2020 [cited 2020 Jul 1];; running, even once a week, can significantly reduce the risk of dying from cancer and cardiovascular diseases (195)Pedisic Z, Shrestha N, Kovalchik S, Stamatakis E, Liangruenrom N, Grgic J, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med [Internet]. BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2019 [cited 2020 Jul 1];. Considering this evidence, it is concerning that more than 1 in 7 adults across all U.S. states and territories are physically inactive, and only a quarter of children and youth ages 6 to 17 get the recommended hour of moderate-to-vigorous exercise a day (118)Adult Physical Inactivity Prevalence Maps by Race/Ethnicity | Physical Activity | CDC [Internet]. [cited 2020 Jan 17].(196). It is imperative that health care professionals and policy makers work together to increase awareness of the benefits of physical activity and support efforts to implement programs and policies to facilitate a physically active lifestyle for all Americans.
Limit Alcohol Consumption
Drinking alcohol increases the risk for six different types of cancer (198) (see Figure 9). Even modest use of alcohol may increase cancer risk, but the greatest risks are associated with excessive and/or long-term consumption (199)Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol [Internet]. Elsevier; 2017 [cited 2018 Apr 3];70:913–22.(200)White AJ, DeRoo LA, Weinberg CR, Sandler DP. Lifetime Alcohol Intake, Binge Drinking Behaviors, and Breast Cancer Risk. Am J Epidemiol [Internet]. Oxford University Press; 2017 [cited 2018 May 7];186:541–9.(201)LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol [Internet]. 2018 [cited 2018 May 3];36:83–93.(202)Hydes TJ, Burton R, Inskip H, Bellis MA, Sheron N. A comparison of gender-linked population cancer risks between alcohol and tobacco: how many cigarettes are there in a bottle of wine? BMC Public Health [Internet]. BioMed Central; 2019 [cited 2019 May 10];19:316.(see sidebar on Guidelines for Alcohol Consumption). Researchers have identified multiple ways in which alcohol may increase the risk of cancer, including directly damaging cellular DNA and proteins through the production of toxic chemicals, once alcohol is metabolized after drinking (203). Alcohol can also increase levels of estrogen and other hormones that are associated with breast cancer (204). Several reports indicate that the use of alcohol has been rising in the U.S. in recent years (205)Alcohol Consumption | Cancer Trends Progress Report [Internet]. [cited 2020 Jul 1]. (206)(207)Han BH, Moore AA, Ferris R, Palamar JJ. Binge Drinking Among Older Adults in the United States, 2015 to 2017. J Am Geriatr Soc [Internet]. John Wiley & Sons, Ltd; 2019 [cited 2020 Mar 16];67:2139–44.. Concurrent with increases in consumption, rates of alcohol-related deaths have also increased at an alarming rate (208)(209)S S, MS S, AF B, EA H, DR W, Y C, et al. Trends in Alcohol-Induced Deaths in the United States, 2000-2016. JAMA Netw open [Internet]. JAMA Netw Open; 2020 [cited 2020 Jul 1];3..
Beyond the United States, alcohol poses a significant public health challenge globally. In fact, alcohol-use disorders are now the most prevalent of all substance-use disorders worldwide (213)GBD 2016 Alcohol and Drug Use Collaborators L, Charlson F, Ferrari A, Santomauro D, Erskine H, Mantilla-Herrara A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The lancet Psychiatry [Internet]. Elsevier; 2018 [cited 2019 May 10];5:987–1012., and in 2016, 4.2 percent of all cancer deaths globally were attributed to alcohol consumption (26). These data underscore the importance of adhering to comprehensive guidelines to limit alcohol intake (for those who drink) and minimize the risk of developing a disease or dying due to alcohol. Future efforts focusing on public education and evidence-based policy interventions, such as regulating alcohol retail density, taxes, and prices, need to be implemented along with effective clinical strategies to reduce the burden of cancer related to alcohol abuse. In this regard, several recent studies reported that when alcohol bottles contain conspicuous labels providing information on the risks of alcohol consumption and/or drinking guidelines, people are better informed about alcohol’s adverse effects and may limit their drinking (214)Zhao J, Stockwell T, Vallance K, Hobin E. The Effects of Alcohol Warning Labels on Population Alcohol Consumption: An Interrupted Time Series Analysis of Alcohol Sales in Yukon, Canada. J Stud Alcohol Drugs [Internet]. Rutgers University; 2020 [cited 2020 Jul 1];81:225–37.(215)Hobin E, Weerasinghe A, Vallance K, Hammond D, McGavock J, Greenfield TK, et al. Testing Alcohol Labels as a Tool to Communicate Cancer Risk to Drinkers: A Real-World Quasi-Experimental Study. J Stud Alcohol Drugs [Internet]. Rutgers University; 2020 [cited 2020 Jul 1];81:249–61..
Protect Skin from UV Exposure
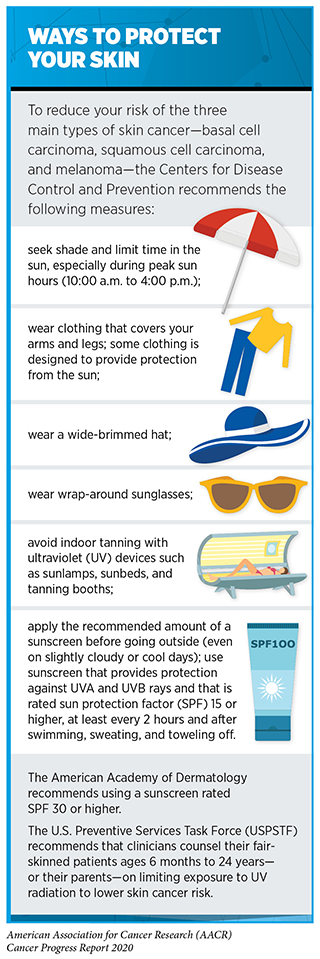
All three main types of skin cancer—basal cell carcinoma, squamous cell carcinoma, and melanoma, the deadliest form of skin cancer—are largely caused by exposure to UV radiation from the sun or indoor tanning devices. In fact, more than 90 percent of the total cases of melanoma during 2011–2015 in the United States were attributable to UV exposure (216)Islami F, Sauer AG, Miller KD, Fedewa SA, Minihan AK, Geller AC, et al. Cutaneous melanomas attributable to ultraviolet radiation exposure by state. Int J Cancer [Internet]. John Wiley & Sons, Ltd; 2020 [cited 2020 Jul 1];ijc.32921.. Sunburn, a clear indication of overexposure to UV radiation, is a preventable risk factor for skin cancer and those events occurring in childhood pose the greatest risk (217)Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson D V, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol [Internet]. NIH Public Access; 2008 [cited 2019 Jul 10];18:614–27.. Therefore, one of the most effective ways a person can reduce his or her risk of skin cancer is by practicing sun-safe habits and not using UV indoor tanning devices (see sidebar on Ways to Protect Your Skin).
In the United States, melanoma incidence has been rising for decades among non-Hispanic whites (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2 [Internet]. [cited 2020 Jun 29].(218)AP T, FJ G. Melanoma Incidence Among Non-Hispanic Whites in All 50 US States From 2001 Through 2015. J Natl Cancer Inst [Internet]. J Natl Cancer Inst; 2020 [cited 2020 Jul 1];112.. To break this trend, multiple sectors including health care, the federal government, business, advocacy, and communities have coordinated efforts through public health campaigns, restrictive policies on tanning, and by encouraging sun-protective behaviors to reduce melanoma risks. As a result, indoor tanning among U.S. youth and adults has declined significantly (219)Guy GP, Watson M, Seidenberg AB, Hartman AM, Holman DM, Perna F. Trends in indoor tanning and its association with sunburn among US adults. J Am Acad Dermatol [Internet]. 2017 [cited 2018 Jun 18];76:1191–3.(220)Guy GP, Berkowitz Z, Everett Jones S, Watson M, Richardson LC. Prevalence of Indoor Tanning and Association With Sunburn Among Youth in the United States. JAMA dermatology [Internet]. 2017 [cited 2018 Jun 18];153:387–90.and early indications suggest that melanoma incidence is also beginning to decline among youth and young adults (ages 10 to 29 years), even though it continues to rise among those older than 40 (218)AP T, FJ G. Melanoma Incidence Among Non-Hispanic Whites in All 50 US States From 2001 Through 2015. J Natl Cancer Inst [Internet]. J Natl Cancer Inst; 2020 [cited 2020 Jul 1];112.(221)Paulson KG, Gupta D, Kim TS, Veatch JR, Byrd DR, Bhatia S, et al. Age-Specific Incidence of Melanoma in the United States. JAMA Dermatology [Internet]. American Medical Association; 2020 [cited 2020 Jul 1];156:57.. Notably, even in 2015, more than 35 percent of adults reported experiencing sunburns, either through outdoor exposure or indoor tanning, in the past year (222). It is also concerning that even though 68 percent of Americans know that skin cancer is the most common cancer in the United States, only 42 percent put sunscreen on parts of their bodies exposed to the sun (223)IPSOS Public Affairs e-Nation survey conducted May 9, 2019 on behalf of The Blue Cross Blue Shield Association. 2017;32:81–4..
Continued efforts from all sectors are necessary to identify and implement more effective interventions to promote sun-safe behavior and reduce the burden of skin cancers. In this regard, a recent clinical trial that tested an intervention using a face-aging mobile app which altered “selfies” to show UV radiation’s effects on an individual’s future faces along with information about UV protection improved the skin cancer preventive behavior of high school students (224)Brinker TJ, Faria BL, de Faria OM, Klode J, Schadendorf D, Utikal JS, et al. Effect of a Face-Aging Mobile App–Based Intervention on Skin Cancer Protection Behavior in Secondary Schools in Brazil. JAMA Dermatology [Internet]. 2020 [cited 2020 Jul 1];.
Prevent and Eliminate Infection with Cancer-causing Pathogens
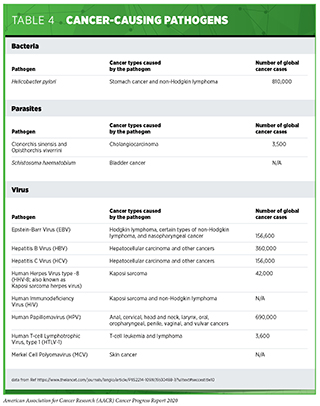
Persistent infection with several pathogens—bacteria, viruses, and parasites that cause disease—increases a person’s risk for several types of cancer (see Table 4). The primary causes of infection-attributable cancers are human papillomavirus (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), and Helicobacter pylori (110)Islami F, Sauer AG, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin [Internet]. 2017;68:31–54.(226)de Martel C, Georges D, Bray F, Ferlay J, Clifford GM, Martel C de, et al. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Heal [Internet]. International Agency for Research on Cancer; 2020 [cited 2020 Jul 1];8:e180–90.(227)Hong CY, Sinn DH, Kang D, Paik SW, Guallar E, Cho J, et al. Incidence of extrahepatic cancers among individuals with chronic hepatitis B or C virus infection: A nationwide cohort study. J Viral Hepat [Internet]. John Wiley & Sons, Ltd; 2020 [cited 2020 Aug 6];jvh.13304.. In the United States, about 3 percent of all cancer cases are attributable to infection with pathogens while globally, an estimated 13 percent of all cancer cases are attributable to infections (110)Islami F, Sauer AG, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin [Internet]. 2017;68:31–54.(226)de Martel C, Georges D, Bray F, Ferlay J, Clifford GM, Martel C de, et al. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Heal [Internet]. International Agency for Research on Cancer; 2020 [cited 2020 Jul 1];8:e180–90.. Individuals can significantly lower their risks by protecting themselves from infection or by obtaining treatment, if available, to eliminate an infection (see sidebar on Preventing or Eliminating Infection with the Four Main Cancer-causing Pathogens). It is important to note that even though strategies to eliminate, treat, or prevent infection with Helicobacter pylori, HBV, HCV, and HPV can significantly lower an individual’s risks for developing cancers, these strategies are not effective at treating infection-related cancers once they develop.
The annual rate of hepatitis C infection has tripled between 2009 and 2018, with infection rates highest among individuals ages 20 to 39 (228). Notably, only about 60 percent of HCV-positive individuals are aware of their status. Because of these alarming trends the CDC and the USPSTF recently updated their prior guidelines on HCV screening calling for universal screening at least once in their lifetime for all average-risk individuals age 18 and older (229)(230)DK O, KW D, AH K, MJ B, M C, AB C, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA [Internet]. JAMA; 2020 [cited 2020 Jul 1];. The CDC also recommends pregnant women to be tested once during each pregnancy. People with continued risk, such as injection drug use, need to be screened regularly.
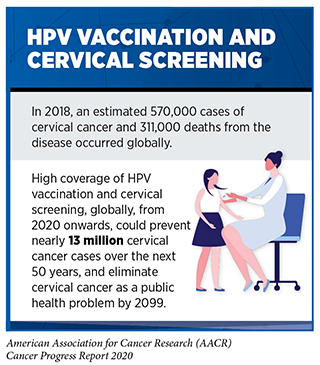
It is estimated that an average of 34,800 cancers reported annually in the United States during 2012–2016 were attributable to HPV infection (231). Notably, most of these cancers are caused by strains of HPV that are targeted by the vaccine Gardasil 9. HPV vaccines are highly effective and can prevent up to 90 percent of HPV-related cancers. Moreover, recent data indicate that in addition to directly protecting individuals who receive the vaccine, increased levels of vaccination may also promote herd immunity among the unvaccinated (232)AK C, BI G, T B, W X, RKL P, L K, et al. Prevalence of Oral HPV Infection in Unvaccinated Men and Women in the United States, 2009-2016. JAMA [Internet]. JAMA; 2019 [cited 2020 Jul 1];322.. Unfortunately, despite the multiple benefits, in 2019, only 57 percent of girls and 52 percent of boys were up to date with the recommended HPV vaccination regimen (121)Elam-Evans LD, Yankey D, Singleton JA, Sterrett N, Markowitz LE, Williams CL, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2019. MMWR Morb Mortal Wkly Rep [Internet]. 2020 [cited 2020 Aug 20];69:1109–16.. While these numbers show slight improvement over earlier years, and there has also been some increase in uptake among young adults ages 18 to 26, vaccination rates in the United States are much lower than they are in other developed countries such as Australia where high vaccination rates (above 70 percent) are predicted to eliminate cervical cancer within the next 20 years (233)(234)Hall MT, Simms KT, Lew J-B, Smith MA, Brotherton JM, Saville M, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. Lancet Public Heal [Internet]. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC-BY-NC-ND 4.0 license; 2018;2667:1–9..
Until recently, cervical cancer was the most common HPV-related cancer in the United States. However, the incidence of HPV-related oropharyngeal and anal cancers has been increasing and oropharyngeal squamous cell carcinoma was recently reported to have become the most common HPV-associated cancer in the United States (237)Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in Human Papillomavirus–Associated Cancers — United States, 1999–2015. MMWR Morb Mortal Wkly Rep [Internet]. 2018;67:918–24.(238)Deshmukh AA, Suk R, Shiels MS, Sonawane K, Nyitray AG, Liu Y, et al. Recent Trends in Squamous Cell Carcinoma of the Anus Incidence and Mortality in the United States, 2001–2015. JNCI J Natl Cancer Inst [Internet]. 2019 [cited 2020 Jul 1];. There are, however, no formal screening tests for oropharyngeal or anal cancers. Therefore, developing effective strategies to increase the uptake of HPV vaccines could have immense public health benefits. In this regard, a recent study reported that protection provided by a single dose of the HPV vaccine is as durable as protection from the two-dose regimen (239)Rodriguez AM, Zeybek B, Vaughn M, Westra J, Kaul S, Montealegre JR, et al. Comparison of the long‐term impact and clinical outcomes of fewer doses and standard doses of human papillomavirus vaccine in the United States: A database study. Cancer [Internet]. John Wiley & Sons, Ltd; 2020 [cited 2020 Jul 1];126:1656–67.. A single shot regimen can potentially improve vaccination rates and reduce health care and associated costs. Ongoing research is also needed to identify effective communications strategies that allow physicians to encourage HPV vaccination with successful implementation. It has been documented that an assertive rather than a passive approach by physicians while raising the issue of HPV vaccination with parents may increase vaccination in young adolescents, although recent reports indicate that some doctors do not follow this approach (240)(241)Kempe A, O’Leary ST, Markowitz LE, Crane LA, Hurley LP, Brtnikova M, et al. HPV Vaccine Delivery Practices by Primary Care Physicians. Pediatrics [Internet]. American Academy of Pediatrics; 2019 [cited 2020 Jul 1];144.. Another policy that may increase vaccination uptake is HPV immunization school-entry requirements. According to a recent report, three U.S. jurisdictions with such requirements had higher levels of vaccination initiation compared with jurisdictions in the same region without any requirements (242)Ko JS, Goldbeck CS, Baughan EB, Klausner JD. Association Between Human Papillomavirus Vaccination School-Entry Requirements and Vaccination Initiation. JAMA Pediatr [Internet]. 2020 [cited 2020 Jul 1];.
Be Cognizant of Reproductive and Hormonal Influences
Breastfeeding
There is strong evidence that breastfeeding decreases the risk of breast cancer in the mother (243)AICR, WCRF. Lactation and the risk of cancer. 2018;. Women who breastfeed have a lower risk of a particularly aggressive type of breast cancer known as triple-negative breast cancer (244)Palmer JR, Viscidi E, Troester MA, Hong C-C, Schedin P, Bethea TN, et al. Parity, lactation, and breast cancer subtypes in African American women: results from the AMBER Consortium. J Natl Cancer Inst [Internet]. 2014 [cited 2019 Jun 19];106.. According to recent data (245)Islami F, Liu Y, Jemal A, Zhou J, Weiderpass E, Colditz G, et al. Breastfeeding and breast cancer risk by receptor status–a systematic review and meta-analysis. Ann Oncol Off J Eur Soc Med Oncol [Internet]. 2015 [cited 2019 Jun 19];26:2398–407., breastfeeding is associated with a 22 percent reduction in the risk of developing triple-negative breast cancer, whereas weaker or no correlations have been observed with other types of breast cancer. Emerging evidence suggests that breastfeeding may also be associated with a lower risk of ovarian cancer, conferring reduction of cancer risk in both white and African American women (246)A B, N S, BA R, SS T, SJ J, HA R, et al. Association Between Breastfeeding and Ovarian Cancer Risk. JAMA Oncol [Internet]. JAMA Oncol; 2020 [cited 2020 Jul 1];6.(247)Moorman PG, Alberg AJ, Bandera E V, Barnholtz-Sloan J, Bondy M, Cote ML, et al. Reproductive factors and ovarian cancer risk in African-American women. Ann Epidemiol [Internet]. NIH Public Access; 2016 [cited 2020 Jul 28];26:654–62.. Increasing awareness of this information among African American women may be particularly important because African American women have a disproportionately high incidence of triple-negative breast cancer and a lower prevalence of breastfeeding compared with all other U.S. racial and ethnic groups (248)Beauregard JL, Hamner HC, Chen J, Avila-Rodriguez W, Elam-Evans LD, Perrine CG. Racial Disparities in Breastfeeding Initiation and Duration Among U.S. Infants Born in 2015. Morb Mortal Wkly Rep [Internet]. Centers for Disease Control and Prevention; 2019 [cited 2020 Jul 1];68:745..
Hormone replacement therapy
Hormone replacement therapy (HRT) refers to treatments that aim to relieve the common symptoms of menopause and the long-term biological changes, such as bone loss, that occur after menopause due to declining levels of the hormones estrogen and progesterone in a woman’s body. HRT usually involves treatment with estrogen alone or estrogen in combination with progestin, a synthetic hormone like progesterone. Women who have a uterus are prescribed estrogen plus progestin. This is because estrogen alone, but not in combination with progestin, is associated with an increased risk of endometrial cancer, a type of cancer that forms in the tissue lining the uterus. Estrogen alone is used only in women who have had their uteruses removed.
The most comprehensive evidence about the health effects of HRT was obtained from clinical trials conducted by the NIH as part of the Women’s Health Initiative. The data indicated that women who use estrogen plus progestin have an increased risk of developing breast cancer (249)Chlebowski RT, Anderson G, Pettinger M, Lane D, Langer RD, Gilligan MA, et al. Estrogen Plus Progestin and Breast Cancer Detection by Means of Mammography and Breast Biopsy. Arch Intern Med [Internet]. 2008 [cited 2019 Jun 19];168:370.(250)Chlebowski RT, Anderson GL, Aragaki AK, Manson JE, Stefanick ML, Pan K, et al. Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women’s Health Initiative Randomized Clinical Trials. JAMA [Internet]. American Medical Association; 2020 [cited 2020 Aug 2];324:369.. The risk is greater with longer duration of use (251)Chlebowski RT, Kuller LH, Prentice RL, Stefanick ML, Manson JE, Gass M, et al. Breast Cancer after Use of Estrogen plus Progestin in Postmenopausal Women. N Engl J Med [Internet]. 2009 [cited 2019 Jun 19];360:573–87.(252)Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet [Internet]. Elsevier; 2019 [cited 2020 Jul 1];394:1159–68.. Women who are no longer using HRT have a lower risk than current users but remain at an elevated risk for more than a decade after they have stopped taking the drugs (252)Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet [Internet]. Elsevier; 2019 [cited 2020 Jul 1];394:1159–68.. Notably, the increased risks have been observed both for white and Black women (253)Ellingjord-Dale M, Vos L, Tretli S, Hofvind S, Dos-Santos-Silva I, Ursin G. Parity, hormones and breast cancer subtypes – results from a large nested case-control study in a national screening program. Breast Cancer Res [Internet]. 2017 [cited 2019 Jun 19];19:10.(254)Rosenberg L, Bethea TN, Viscidi E, Hong C-C, Troester MA, Bandera E V, et al. Postmenopausal Female Hormone Use and Estrogen Receptor-Positive and -Negative Breast Cancer in African American Women. J Natl Cancer Inst [Internet]. 2016 [cited 2019 Jun 19];108:djv361.. Therefore, all individuals who are seeking relief from menopausal symptoms should discuss with their health care providers the advantages and possible risks of using HRT before deciding what is right for them.
Limit Exposure to Environmental Carcinogens
Environmental exposures to pollutants and certain occupational agents can increase a person’s risk of cancer. For example, radon, a naturally occurring radioactive gas that comes from the breakdown of uranium in soil, rock, and water, is the second leading cause of lung cancer in the United States (129)Cancer Trends Progress Report National Cancer Institute, NIH, DHHS, Bethesda, MD, March 2020, https://progressreport.cancer.gov. [Internet]. [cited 2020 Jun 30].. Other examples of environmental carcinogens include arsenic, asbestos, lead, radiation, and benzene. According to the World Health Organization (WHO), environmental risk factors account for nearly 20 percent of all cancers globally, most of which occur in low- and middle-income countries.
It is often difficult for people to avoid or reduce their exposure to environmental carcinogens, and not every exposure will lead to cancer. The intensity and duration of exposure, combined with an individual’s biological characteristics, including genetic makeup, determine each person’s chances of developing cancer over his or her lifetime. In addition, when studying environmental cancer risk factors, it is important to consider that exposure to several environmental cancer risk factors may occur simultaneously. Growing knowledge of the environmental pollutants to which different segments of the U.S. population are exposed highlights new opportunities for education and policy initiatives to improve public health.
One environmental pollutant that was classified by the International Agency for Research on Cancer (IARC), an affiliate of the WHO, as having the ability to cause cancer in humans, is outdoor air pollution (255)Loomis D, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, et al. The carcinogenicity of outdoor air pollution. Lancet Oncol [Internet]. 2013 [cited 2019 Jun 19];14:1262–3.. Two types of air pollution are most common in the United States, ozone and particle pollution. Particle pollution refers to a mix of tiny solid and liquid particles that are in the air we breathe, and in 2013, IARC concluded that particle pollution may cause lung cancer (256). Therefore, it is concerning that between 2016 and 2018, more than 21 million people in the United States were exposed year-round to unhealthy levels of particle pollution (256). New policy efforts to reduce the release of pollutants into the atmosphere are urgently needed to combat the adverse health effects of air pollution.
Involuntary exposures to environmental pollutants usually occur in subgroups of the population, such as workers in certain industries who may be exposed to carcinogens on the job or individuals living in low-income neighborhoods. Similarly, there are disparities in the burden of cancers caused by environmental exposures based on geographic locations and socioeconomic status (257)Tristan Baurick, Lylla Younes joan meiners. Welcome to “Cancer Alley,” Where Toxic Air Is About to Get Worse. propublica [Internet]. 2019 [cited 2020 Jul 1];63:507–20.. As we learn more about environmental and occupational cancer risk factors and identify those segments of the U.S. population who are exposed to these factors, we need to develop and implement new and/or more effective policies that benefit everyone, including the most vulnerable and underserved populations.
Emerging Evidence on Cancer Risk Factors
In addition to epidemiological data on increasing incidence or death from cancers, emerging mechanistic studies indicate how cancer risk factors such as obesity, smoking, and reproductive factors can influence disease subtype, aggressiveness, and outcomes through their effects on cancer cells and/or the tumor microenvironment including immune cells (258)Fortner RT, Poole EM, Wentzensen NA, Trabert B, White E, Arslan AA, et al. Ovarian cancer risk factors by tumor aggressiveness: An analysis from the Ovarian Cancer Cohort Consortium. Int J Cancer [Internet]. John Wiley & Sons, Ltd; 2019 [cited 2020 Jul 1];145:58–69.(259)Yarmolinsky J, Relton CL, Lophatananon A, Muir K, Menon U, Gentry-Maharaj A, et al. Appraising the role of previously reported risk factors in epithelial ovarian cancer risk: A Mendelian randomization analysis. Minelli C, editor. PLOS Med [Internet]. Public Library of Science; 2019 [cited 2020 Jul 1];16:e1002893.(260)H K, T H, M S, L L, Y C, JA N, et al. Physical Activity and Colorectal Cancer Prognosis According to Tumor-Infiltrating T Cells. JNCI cancer Spectr [Internet]. JNCI Cancer Spectr; 2018 [cited 2020 Jul 1];2.(261). Further research is needed to harness this knowledge for advancing cancer prevention and/or clinical management of disease. There is also accumulating evidence that suggest that beyond the well-established cancer risk factors, discussed above, there are several behavioral, social, as well as biological influences that may contribute to cancer development.
Psychosocial Stress
Stress-related social and behavioral factors have been considered as possible cancer risk factors. For example, it has been suggested that having a stress-prone personality and poor coping skills, as well as trauma-induced distress can affect incidence, mortality, and survival for various types of cancer (262)Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol [Internet]. 2008 [cited 2019 Dec 16];5:466–75.(263)Roberts AL, Huang T, Koenen KC, Kim Y, Kubzansky LD, Tworoger SS. Posttraumatic stress disorder (PTSD) is associated with increased risk of ovarian cancer: a prospective and retrospective longitudinal cohort study. Cancer Res [Internet]. American Association for Cancer Research; 2019 [cited 2020 Jul 1];(264)Moreno-Smith M, Lutgendorf SK, Sood AK. Impact of stress on cancer metastasis. Futur Oncol [Internet]. Future Medicine Ltd London, UK ; 2010 [cited 2020 Jul 1];6:1863–81.. It is not clear whether the effects of stress-related psychological factors on cancer are due to an increase in risk-enhancing lifestyles, such as smoking, alcohol consumption, poor diet, and physical inactivity, or due to direct effects on our physiological systems. There is some evidence that stress can directly affect hormones and/or cellular processes including those that regulate our immune function, which in turn may contribute to cancer incidence or outcomes (262)Chida Y, Hamer M, Wardle J, Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol [Internet]. 2008 [cited 2019 Dec 16];5:466–75.(265)CB C-E, R L-C, AN A-A, GN A-P. Neuroendocrine Regulation of Tumor-Associated Immune Cells. Front Oncol [Internet]. Front Oncol; 2019 [cited 2020 Jul 1];9.(266)Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer [Internet]. John Wiley & Sons, Ltd; 2019 [cited 2020 Jul 1];125:1417–31.(267)Vick AD, Burris HH. Epigenetics and Health Disparities. Curr Epidemiol reports [Internet]. 2017 [cited 2019 Dec 17];4:31–7.. One area of intensive research investigation is understanding the contribution of the allostatic load, which describes the combined influences of stresses, lifestyle, and environmental exposures, on the lifetime risk of cancer and other diseases (269)Shiels PG, Buchanan S, Selman C, Stenvinkel P. Allostatic load and ageing: linking the microbiome and nutrition with age-related health. Biochem Soc Trans [Internet]. 2019 [cited 2020 Jan 22];47:1165–72..
Metabolomics
The small molecules that are produced when our bodies break down food, drugs, chemicals, or our own tissue are known as metabolites. The process of breakdown, referred to as metabolism, produces the energy and materials that cells need to grow, reproduce, get rid of toxic substances, and stay healthy. Cancer development is associated with changes in the normal cellular metabolism, which provides the energy needed for uncontrolled cellular growth and division (270)Hanahan D, Weinberg RA. Hallmarks of Cancer: The Next Generation. Cell [Internet]. Elsevier; 2011 [cited 2020 Jul 1];144:646–74.. Metabolomics is the study of metabolites in an individual’s cells and tissues and is a measure of the “markers” of how well cells are functioning. Metabolites can be detected in the blood, urine, and other biospecimens. An individual’s genetic makeup, lifestyle and environmental exposures such as diet and medications determine which metabolites are made and used in the body. Notably, emerging evidence suggests that certain metabolites may be associated with cancer development (271)Zeleznik OA, Eliassen AH, Kraft P, Poole EM, Rosner BA, Jeanfavre S, et al. A prospective analysis of circulating plasma metabolites associated with ovarian cancer risk. Cancer Res [Internet]. American Association for Cancer Research; 2020 [cited 2020 Jul 1];(272)Zhao H, Shen J, Moore SC, Ye Y, Wu X, Esteva FJ, et al. Breast cancer risk in relation to plasma metabolites among Hispanic and African American women. Breast Cancer Res Treat [Internet]. Springer; 2019 [cited 2020 Jul 1];176:687–96.(273)X S, YB X, N R, D Y, HL L, G Y, et al. Prospective Study of Blood Metabolites Associated With Colorectal Cancer Risk. Int J cancer [Internet]. Int J Cancer; 2018 [cited 2020 Jul 1];143.(274)Zeleznik OA, Clish CB, Kraft P, Avila-Pacheco J, Eliassen AH, Tworoger SS. Circulating Lysophosphatidylcholines, Phosphatidylcholines, Ceramides, and Sphingomyelins and Ovarian Cancer Risk: A 23-Year Prospective Study. J Natl Cancer Inst [Internet]. J Natl Cancer Inst; 2020 [cited 2020 Jul 28];112:628–36.(275)Mayers JR, Wu C, Clish CB, Kraft P, Torrence ME, Fiske BP, et al. Elevation of circulating branched-chain amino acids is an early event in human pancreatic adenocarcinoma development. Nat Med [Internet]. Nat Med; 2014 [cited 2020 Jul 28];20:1193–8.(276)Dickerman BA, Ebot EM, Healy BC, Wilson KM, Eliassen AH, Ascherio A, et al. A Metabolomics Analysis of Adiposity and Advanced Prostate Cancer Risk in the Health Professionals Follow-Up Study. Metabolites [Internet]. Metabolites; 2020 [cited 2020 Jul 28];10.. However, more research is needed to evaluate whether the metabolite itself contributes to cancer development as opposed to factors that influence the metabolite levels (e.g., medication, environmental, or lifestyle factors). Definitive evidence on whether and which metabolites are associated with cancer risk will lead to more opportunities to develop preventive and/or therapeutic interventions against cancers.