- Research: Driving Progress Against Cancer
- Spotlight: Cancer in Children, Adolescents, and Young Adults (AYA)
- Cancer: An Ongoing Challenge
- Inequities in the Burden of Cancer in the United States
- Variable Progress Against Different Types of Cancer and Stages of Diagnosis
- The Growing Population Burden of Cancer
- The Global Burden of Cancer
- Funding Cancer Research: A Vital Investment
Cancer in 2024
In this section, you will learn:
- In the United States (US), the overall cancer death rate has been steadily declining since the 1990s, with the reductions between 1991 and 2021 translating into more than 4.1 million cancer deaths avoided.
- The decline in overall US cancer death rate is attributable to reduction in smoking rates, as well as improvements in treatment and early detection of certain cancers.
- More than 18 million cancer survivors were living in the United States as of January 1, 2022.
- Progress has not been even against all cancer types or all stages of a given cancer type.
- Many segments of the US population experience stark inequities in the cancer burden; these inequities are largely driven by structural and social factors.
- It is imperative that all stakeholders work together to implement evidence-based interventions including public policies that guarantee equitable access to quality health care for all patients, regardless of their race, ethnicity, age, sexual orientation, gender identity, socioeconomic status, or geographic location.
- The economic burden of cancer on individuals and the US health care system is expected to rise in the coming decades, highlighting the urgent need for more research and increased federal support for medical science and public health to accelerate the pace of progress against cancer.
Research: Driving Progress Against Cancer
Research is the foundation of progress against the collection of diseases we call cancer. It improves survival and quality of life for people around the world because it is the driving force behind every clinical breakthrough and every public policy designed to improve human health. Discoveries across the major areas of cancer research, including basic, clinical, translational, and population science, provide the foundation for advances in cancer prevention, early detection, diagnosis, treatment, and survivorship.
Every clinical advance and every policy that spurs progress against cancer is the culmination of a complex process that requires collaboration over the course of many years among numerous stakeholders (see Sidebar 1).
The remarkable advances made against cancer—in particular, improvements in early detection, diagnosis, treatment, and risk reduction—are resulting in a steady decline in US cancer death rates year after year. In fact, the age-adjusted overall cancer death rate has fallen by 33 percent between 1991 and 2021, a reduction that translates into an estimated 4.1 million fewer deaths from cancer (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024. . The reduction in overall US cancer mortality rate can be attributed to significant reduction in smoking rates, as well as improvements in treatment and early detection of certain cancers.
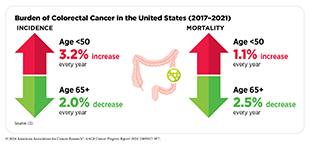
Reduction in death rates for breast cancer among females and colorectal cancer among those over age 50 since the 1990s contributed to the progress in reducing overall US cancer mortality (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024.. According to a recent analysis, US breast cancer mortality declined by 42 percent, averting greater than 490,000 deaths between 1989 and 2021, because of advances in screening mammography and treatment (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024.. The death rate for colorectal cancer, overall, has declined by 39 percent between 2000 and 2022 (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. However, mortality has been rising among those diagnosed before the age of 50 (see Cancer in Children, Adolescents, and Young Adults (AYA)).
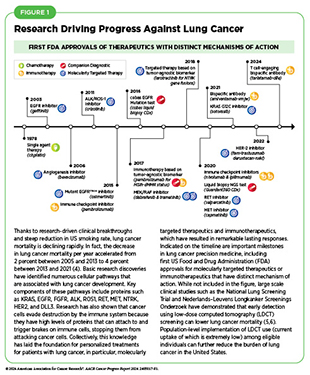
The accelerated decline in overall cancer mortality in the past decade has been driven largely by rapid decreases in US lung cancer death rates in both men and women, attributable to public health interventions to reduce smoking as well as advances in treatment (see Figure 1) and early detection (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024..
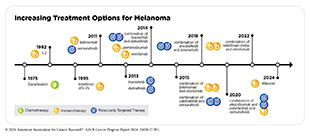
Research-driven advances in treatment have resulted in a steady decline in death rates despite increasing incidence for leukemia, melanoma, and kidney cancer (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024.. For example, groundbreaking basic research in the 1960s through 1980s that identified the mechanistic underpinnings of chronic myeloid leukemia (CML), a cancer of the blood and bone marrow, propelled the development of a cascade of new treatments that have drastically improved outcomes for patients (7)Howlader N, et al. (2023) Cancer Epidemiol Biomarkers Prev, 32: 744.. Advances in the treatment of kidney cancer, in particular, with molecularly targeted therapeutics and immunotherapeutics have transformed clinical care for these patients. In fact, in a recent study, an immunotherapeutic, pembrolizumab (Keytruda), was shown to be the first postsurgical treatment that helps patients with early-stage kidney cancer live longer (8)Choueiri TK, et al. (2024) N Engl J Med, 390: 1359. DOI: 10.1056/NEJMoa2312695..
Among the major advances made across the clinical cancer care continuum from July 1, 2023, to June 30, 2024, are 15 new anticancer therapeutics that were approved for use by the US Food and Drug Administration (FDA) (see Progress Across the Clinical Cancer Care Continuum). During this period, FDA also approved new uses for 15 previously approved anticancer therapeutics, a new imaging agent to help visualize cancerous cells during surgery, and several artificial intelligence (AI) based tools to improve early detection and diagnosis of cancers.
Collectively, advances such as these and those described in past editions of this annual report are helping to increase the number of children and adults who live longer and fuller lives after a cancer diagnosis. Indeed, the 5-year relative survival rate for all cancers combined has increased from 49 percent for those diagnosed in the mid-1970s to 69 percent among those diagnosed during 2013 to 2019 (4). As of January 1, 2022, more than 18 million individuals with a history of cancer were alive in the United States, and the number is projected to grow to 26 million by 2040 (9). Additionally, because of improved treatments, increasing numbers of individuals are now living longer despite being diagnosed with metastatic disease (10). Continued research to address the survivorship needs of the growing number of individuals living with cancer must be a priority for US medicine and public health (see Supporting Cancer Patients and Survivors).

Cancer in Children, Adolescents, and Young Adults (AYA)
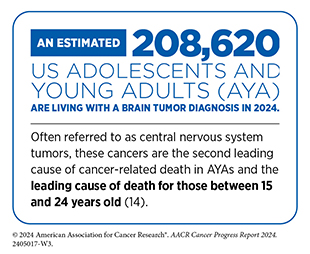
Compared to cancers in adults, cancers are rare in children, adolescents and young adults (AYA). In the United States in 2024, approximately 9,620 children (14 years and younger) and 5,290 adolescents (15 to 19 years) will be diagnosed with cancer (4)Siegel RL, et al. (2024) CA Cancer J Clin, 74: 12. DOI: 10.3322/caac.21820.. Leukemia and cancers of the nervous system, including brain tumors, are the most common cancers in children. Among adolescents, brain and nervous system tumors are the leading sites of new cancer cases, followed by lymphoma and leukemia. In contrast, young adults ages 20 to 39 years are most commonly diagnosed with solid tumors, including thyroid cancer, melanoma, and breast cancer.
Decades of research-driven advances in cancer science and medicine, including the identification and therapeutic targeting of cellular and molecular drivers of cancer (see Research-driven Progress Against Childhood and AYA Cancers), along with progress in surgical techniques and optimization of radiotherapy and chemotherapy have led to a steady decline in cancer death rates for children and adolescents. Among US children (14 years and younger) and adolescents (15 to 19 years), overall cancer death rates have declined by 70 percent and 63 percent, respectively, between 1970 and 2021 (4)Siegel RL, et al. (2024) CA Cancer J Clin, 74: 12. DOI: 10.3322/caac.21820.. Just in the past two decades, the overall cancer death rate for children and adolescents declined by 24 percent (11)Centers for Disease Control and Prevention. Declines in Cancer Death Rates Among Youth: United States, 2001–2021. Accessed: July 5, 2024..
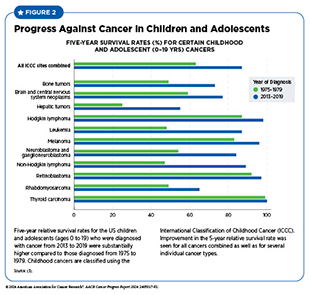
The 5-year relative survival rate for all cancers combined has improved for US children from 58 percent during the mid-1970s to 85 percent for those diagnosed between 2013 and 2019 (4)Siegel RL, et al. (2024) CA Cancer J Clin, 74: 12. DOI: 10.3322/caac.21820.. However, there are significant differences in survival rates between different cancer types (see Figure 2). Cancer survival has also improved for AYAs. Based on a recent study that evaluated survival trends across 33 common AYA cancers, those diagnosed between 2010 and 2018 had a 5-year relative survival of 86 percent (12)Keegan THM, et al. (2024) J Clin Oncol, 42: 630. DOI: 10.1200/JCO.23.01367.. Of the 33 cancer types, 25 had significant improvement in 5-year relative survival since 2000. However, AYAs had a much lower 5-year relative survival than children for four cancers, including acute lymphocytic leukemia (ALL) and Ewing sarcoma (12)Keegan THM, et al. (2024) J Clin Oncol, 42: 630. DOI: 10.1200/JCO.23.01367..
Despite the progress, cancer is the leading cause of disease-related death among US children, with around 1,040 children expected to die from the disease this year (4)Siegel RL, et al. (2024) CA Cancer J Clin, 74: 12. DOI: 10.3322/caac.21820.. Additionally, there are disparities in the burden of childhood and AYA cancers for racial and ethnic minority groups and other medically underserved populations in the United States. As one example, while the overall cancer death rate for White children and adolescents declined by 12 percent between 2011 and 2021, the rates did not change significantly for Black and Hispanic children and adolescents (11)Centers for Disease Control and Prevention. Declines in Cancer Death Rates Among Youth: United States, 2001–2021. Accessed: July 5, 2024.. Recent data also show that non-Hispanic Black AYAs experience worse survival for many cancers compared to other racial and ethnic groups (12)Keegan THM, et al. (2024) J Clin Oncol, 42: 630. DOI: 10.1200/JCO.23.01367..
Additionally, there are disparities based on socioeconomic status. For instance, children with cancer living in Alabama counties with persistent poverty during 2000–2016 were 30 percent more likely to die within 5 years of cancer diagnosis, compared to those not living in Alabama counties with persistent poverty (13)Hoppmann AL, et al. (2023) Cancer Epidemiol Biomarkers Prev, 32: 380..
Addressing the barriers that drive survival disparities in childhood and AYA cancers, such as lack of clinical trial enrollment, access to guideline-adherent treatments, and long-term survivorship care, as well as identifying biological features of these cancers is vital for continued progress.
While overall cancer incidence in the United States has stabilized in recent years, a rising concern among public health experts is the steadily increasing incidence of certain cancer types among individuals younger than 50 years, a phenomenon referred to as early-onset cancer. According to a recent report, the incidence of early-onset cancers, particularly among individuals aged 30 to 39 years, increased significantly during 2010 to 2019 (15)Koh B, et al. (2023) JAMA Netw Open, 6: e2328171. DOI: 10.1001/jamanetworkopen.2023.28171.. In 2019, most early-onset cancers were diagnosed in the breast, thyroid, colon, and rectum (15)Koh B, et al. (2023) JAMA Netw Open, 6: e2328171. DOI: 10.1001/jamanetworkopen.2023.28171.. Between 2010 and 2019 the greatest increase in early-onset cancer occurred for those arising in the gastrointestinal system. In fact, many studies have reported an increase in the incidence of early-onset colorectal cancer (16)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 233. DOI: 10.3322/caac.21772.(17)Giannakis M, et al. (2023) Science, 379: 1088. DOI: 10.1126/science.ade7114.. According to a recent report, between 2011 and 2019, colorectal cancer incidence rates increased by 1.9 percent per year in people younger than 50 years (16)Siegel RL, et al. (2023) CA Cancer J Clin, 73: 233. DOI: 10.3322/caac.21772.(18)Sinicrope FA (2022) N Engl J Med, 386: 1547. DOI: 10.1056/NEJMra2200869..
Another cancer for which the incidence rate has been rising in US young adults is cervical cancer (19)Francoeur AA, et al. (2022) Int J Gynecol Cancer, 32: 1115. DOI: 10.1136/ijgc-2022-003728.(20)Shahmoradi Z, et al. (2022) JAMA, 328: 2267. DOI: 10.1001/jama.2022.17806.. Specifically, a recent analysis revealed that cervical cancer incidence among women ages 30 to 34 years increased by 2.5 percent per year between 2012 and 2019 (20)Shahmoradi Z, et al. (2022) JAMA, 328: 2267. DOI: 10.1001/jama.2022.17806.. Considering that cervical cancers are largely preventable—most cases are caused by infection with human papillomavirus (HPV), and HPV vaccination (see Prevent and Eliminate Infection From Cancer-causing Pathogens) and cervical cancer screening are extremely effective in reducing the burden of cervical cancer—these data emphasize the critical importance of public health measures to boost cervical cancer prevention and early detection in the United States (see Screening for Early Detection).
In this regard, research has shown that in young women who were most likely to have received the HPV vaccines, cervical cancer incidence is declining rapidly. As one example, in women aged 20 to 24 years, invasive cervical cancer incidence decreased by 65 percent from 2012 to 2019 compared to only by 24 percent from 2005 to 2012 (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024..
Cancer: An Ongoing Challenge
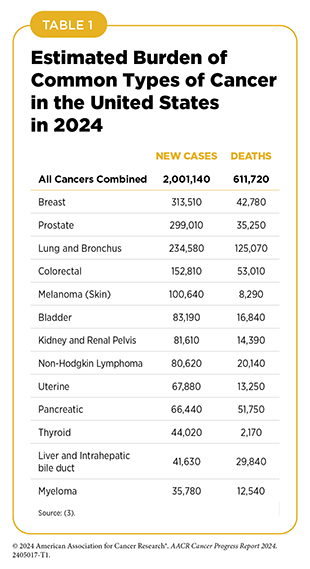
Although incredible progress has been made against cancer, it continues to be an enormous public health challenge in the United States and around the world. In the United States, an estimated 2,001,140 new cases of cancer will be diagnosed in 2024 and 611,720 people will die from the disease (see Table 1). Men have a higher incidence of many cancer types, including bladder, colon, and brain cancer, compared to women, and ongoing research is evaluating the role of a range of biological factors including genetics, epigenetics, metabolism, and immunity in mediating the sex differences in cancer burden (21)Rubin JB, et al. (2024) J Clin Invest, 134. DOI: 10.1172/JCI180071.(22)Yang W, et al. (2024) Biol Sex Differ, 15: 35. DOI: 10.1186/s13293-024-00607-1.(23)Rubin JB (2022) Trends Cancer, 8: 303. DOI: 10.1016/j.trecan.2022.01.013..
In addition, many population groups in the United States experience disproportionately high rates of cancer incidence and death that are attributable largely to structural and socioeconomic disadvantages. It should also be noted that current estimates of the cancer burden do not reflect the adverse impact of COVID-19, which caused declines in screening, early detection, new cancer diagnoses, and delays or discontinuations in cancer treatment, especially for medically underserved populations (24)American Association for Cancer Research. AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care. Accessed: June 30, 2022.(25)Berrian J, et al. (2023) Cancer Med, 12: 7381. DOI: 10.1002/cam4.5439.(26)Zhao J, et al. (2023) JCO Oncol Pract, 19: 501. DOI: 10.1200/OP.22.00522.(27)Llanos AAM, et al. (2023) JAMA Netw Open, 6: e2251165. DOI: 10.1001/jamanetworkopen.2022.51165.. Ongoing monitoring of cancer-related data at a population level is warranted to assess the long-term consequences of COVID-19 for cancer burden in the United States.
Inequities in the Burden of Cancer in the United States
While we are making unprecedented advances against cancer, these advances have not benefited everyone equally. Because of a long history of structural inequities and systemic injustices in the United States, certain segments of the population continue to shoulder a disproportionate burden of adverse health conditions, including cancer.
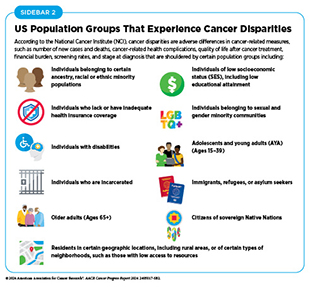
Cancer disparities are one of the most pressing public health challenges in the United States. The National Cancer Institute (NCI) defines cancer disparities as adverse differences in cancer-related measures, such as number of new cases, number of deaths, cancer-related health complications, survivorship and quality of life after cancer treatment, screening rates, and cancer stage at diagnosis, that exist among certain population groups (see Sidebar 2).
As detailed in the AACR Cancer Disparities Progress Report 2024 (29)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2024. Accessed: June 14, 2024., US racial and ethnic minority groups and other medically underserved populations shoulder a disproportionately higher burden of cancer (see Sidebar 3,). As one example, during 2017–2021, the incidence rate for all cancers combined was higher among American Indian and Alaska Native (AI/AN) people compared to non-Hispanic (NH) White people (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. During the same time, overall cancer mortality rates were higher among Black and AI/AN individuals compared to NH White individuals. Additionally, during 2014–2020, patients with cancer from all racial and ethnic minority groups had a lower 5‐year relative survival compared to NH White people (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024..
There has been progress in reducing cancer disparities in recent years. As one example, the gap in overall cancer death rates between Black and White populations has narrowed by more than 50 percent over the past two decades (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. However, Black individuals still had a 9 percent higher overall cancer death rate compared to White individuals, and the highest death rate from cancer among all US racial or ethnic groups, in 2022 (3).
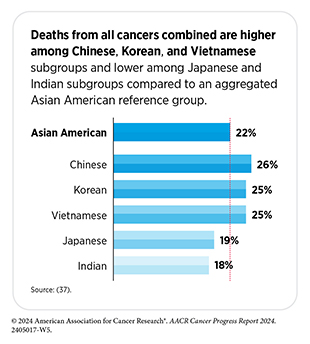
Researchers studying the science of cancer disparities are increasingly recognizing the heterogeneity in the cancer burden within each of the major racial or ethnic minority groups. As one example, striking disparities in cancer burden have been identified within Asian subpopulations and between Native Hawaiian or other Pacific Islander (NHOPI) and Asian individuals (29)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2024. Accessed: June 14, 2024.. Notably, the US Asian population has ancestry in numerous countries of origin, and the NHOPI population comprises diverse subgroups with distinct variations in historical backgrounds, languages, and cultural traditions. However, Asian and NHOPI populations continue to be grouped together in cancer epidemiologic data.
Stark differences in cancer incidence and outcomes have also been observed within the AI/AN populations when cancer data are disaggregated by geographic location. Research has shown that among AI/AN individuals, Indigenous Alaskans had the highest incidence of colorectal cancer between 2014 and 2018, compared to any other US racial population (36)Haverkamp D, et al. (2023) Int J Circumpolar Health, 82: 2184749. DOI: 10.1080/22423982.2023.2184749.. The colorectal cancer incidence among Indigenous Alaskans was in fact the highest in the world in 2018 (36)Haverkamp D, et al. (2023) Int J Circumpolar Health, 82: 2184749. DOI: 10.1080/22423982.2023.2184749.. These findings indicate that collection of disaggregated data is a vital step to fully understanding cancer disparities and developing effective strategies for achieving health equity.
In addition to racial and ethnic minority groups, many segments of the US population shoulder a disproportionate burden of cancer. These include residents in rural areas that lack access to cutting-edge cancer treatments and/or state-of-the-art health care facilities, sexual and gender minorities (SGM) who experience bias and discrimination in health care settings, and low-income households in counties with persistent poverty and limited access to healthy food and/or the needed health care. In addition, older adults, veterans, undocumented immigrants and refugees, individuals with disabilities, individuals who are incarcerated, adolescents, and young adults all are medically underserved to varying degrees and face unique challenges in the burden of cancer.
It should be noted that patients with intersectional identities, for instance, racial or ethnic minority patients from SGM communities, often experience multilevel barriers to cancer care that adversely impact screening, diagnosis, treatment, and survivorship. As another example, older adults (age 65 or older) with cancer often experience multilevel barriers to cancer care and those living in rural areas have an even greater burden—more likely to die within 1 year of cancer diagnosis— compared to those living in urban areas (38)Fowler ME, et al. (2023) J Geriatr Oncol, 14: 101505. DOI: 10.1016/j.jgo.2023.101505..
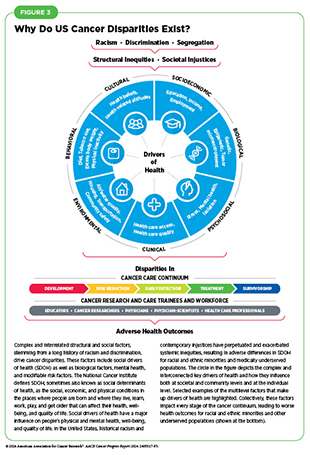
Cancer disparities are driven by complex and interrelated factors. Systemic inequities resulting from a long history of racism and contemporary injustices in the United States continue to have lasting, multigenerational adverse effects on marginalized populations in all aspects of life, including on health outcomes. Researchers use various frameworks to understand and address the influences that affect health outcomes and contribute to health disparities, including cancer disparities. These frameworks integrate influences from structural factors and include the interplay of biological factors, mental health, and modifiable risk factors (e.g., smoking and diet) with nonclinical factors called social drivers of health (SDOH) (39)Warnecke RB, et al. (2008) Am J Public Health, 98: 1608. DOI: 10.2105/AJPH.2006.102525.(40)Asare M, et al. (2017) Oncol Nurs Forum, 44: 20. DOI: 10.1188/17.ONF.20-23..
According to NCI, SDOH, sometimes also called social determinants of health, are the social, economic, and physical conditions in the places where people are born and where they live, learn, work, play, and get older that can affect their health, well-being, and quality of life. Social drivers of health include factors such as socioeconomic status; housing; transportation; and access to healthy food, clean air and water, and health care services (see Figure 3).
A major social driver of cancer disparities is inadequate access to quality health care. Health insurance is a key determinant of whether individuals receive the needed health care. In 2021, nearly 27 percent of US adults ages 18 to 64 who were uninsured delayed or did not receive needed medical care, compared to a little over 7 percent of those who had either public or private insurance (41)Islami F, et al. (2023) CA Cancer J Clin. DOI: 10.3322/caac.21812.. A substantial proportion of racial and ethnic minorities and medically underserved populations in the United States lack health care access (29)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2024. Accessed: June 14, 2024.. Individuals lacking health insurance are less likely to be up to date with recommended cancer screening and are more likely to be diagnosed with cancer at an advanced stage (29)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2024. Accessed: June 14, 2024.. Uninsured patients are also less likely to receive needed treatments and more likely to experience worse cancer outcomes compared to privately insured patients (42)Zhao J, et al. (2022) CA Cancer J Clin, 72: 542. DOI: 10.3322/caac.21732.(43)Chen SY, et al. (2023) Surgery, 174: 1323. DOI: 10.1016/j.surg.2023.09.005.(44)Bassiri A, et al. (2024) J Surg Res, 293: 248. DOI: 10.1016/j.jss.2023.09.013.(45)Samuel D, et al. (2023) Gynecol Oncol, 174: 1. DOI: 10.1016/j.ygyno.2023.04.017..
Considering that a significant proportion of the US population is affected by cancer disparities, it is important that public health experts intensify efforts designed to improve the understanding and mitigation of these inequities. Only with new insights obtained through innovative and inclusive science, such as basic research assessing the effects of chronic stress and using biospecimens from diverse populations, clinical studies involving participants from all sociodemographic backgrounds, and health care delivery and implementation research that is representative of every community, will we be able to achieve health equity for all populations.
Variable Progress Against Different Types of Cancer and Stages of Diagnosis
A significant challenge in cancer science and medicine is the uneven progress against different cancer types and different stages of a given cancer type.
This challenge is illustrated by the fact that the 5-year relative survival rates for US patients vary widely depending on both the type of cancer diagnosed and the stage at diagnosis (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. For example, the overall 5-year relative survival rates of 91 percent for patients with breast cancer and nearly 98 percent for patients with prostate cancer stand in stark contrast to the overall 5-year relative survival rates of 13 percent for those with pancreatic cancer or 8 percent for those with glioblastoma multiforme (GBM), an aggressive form of brain cancer (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024..
In addition, among women with breast cancer and men with prostate cancer, those with early-stage disease, i.e., whose cancer is confined to the breast, or to the prostate, have 5-year relative survival rates of almost 100 percent, while those whose cancer has spread to other organs the 5-year relative survival rates are 32 percent and 37 percent, respectively (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. Notably, the greater 5-year survival among individuals whose cancers were caught early through screening can be partly attributed to lead time bias, a phenomenon where early diagnosis falsely makes it appear that people are surviving longer (see Screening for Early Detection).
Variable progress against different cancer types can be accredited in part to disparities in lifesaving therapeutic options that are available for different cancer types. As an example, just in the past decade, FDA has approved 14 molecularly targeted therapeutics and two immunotherapeutics for the treatment of patients with breast cancer. As a result, patients have a deep selection of therapeutics to choose from and breast cancer mortality has been declining steadily; between 2013 and 2022 the breast cancer death rate fell by an average of 1.2 percent per year (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. In contrast, progress has been slow for patients with GBM. Since the approval of the chemotherapeutic temozolomide nearly 25 years ago, no new anticancer agents have shown promise in improving overall survival. Consequently, the 5-year relative survival rate for patients with GBM remains at a dismal 8 percent (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024..
Developing new and effective tests for the early detection of more cancer types (see Screening for Early Detection) could also help address the challenge of variable progress between types of cancer because the likelihood of a cure is much higher when cancer is diagnosed at an early stage when it is confined to its original location and has not spread to distant sites. Additionally, intensive research to uncover currently unknown biological drivers of cancer initiation and progression is needed to identify novel targets and improve therapeutic options for hard-to-treat cancers.
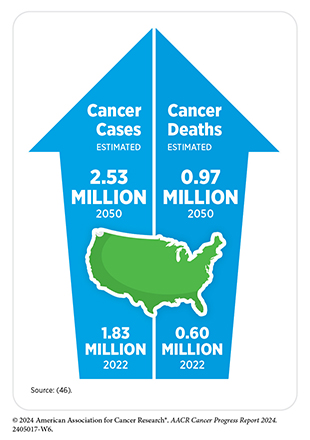
The Growing Population Burden of Cancer
The public health challenges posed by cancer are predicted to grow considerably in the coming decades unless we develop and implement more effective strategies for cancer prevention, early detection, and treatment. In the United States alone, the number of new cancer cases diagnosed each year is expected to surpass 2.5 million by 2050 (46)World Health Organization. Global Cancer Observatory: Cancer Today (version 1.1). Lyon, France: International Agency for Research on Cancer. Accessed: August 2, 2024.. This is because cancer is primarily a disease of aging; 57 percent of diagnoses occur among those 65 and older (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024., and this segment of the US population is expected to grow from 57.8 million in 2022 to more than 82 million in 2050 (47)United States Census Bureau. 2023 Population Projections for the Nation by Age, Sex, Race, Hispanic Origin and Nativity. Accessed: July 10, 2024..
Also contributing to the projected increase in the number of US cancer cases are the high rates of excess body weight, physical inactivity, and alcohol consumption (48)Islami F, et al. (2024) CA Cancer J Clin. DOI: 10.3322/caac.21858. and the continued use of cigarettes by 11.5 percent of adults (49)Cornelius ME, et al. (2023) MMWR Morb Mortal Wkly Rep, 72: 475. DOI: 10.15585/mmwr.mm7218a1. (see Reducing the Risk of Cancer Development). Furthermore, a significant proportion of lung cancers (16 percent in women and 10 percent in men) are diagnosed in individuals without a history of smoking (50)Siegel DA, et al. (2021) JAMA Oncol, 7: 302. DOI: 10.1001/jamaoncol.2020.6362. and there is an urgent need for more research to understand the increasing trends of lung cancer incidence among those without a history of smoking (51)Pelosof L, et al. (2017) J Natl Cancer Inst, 109: djw295. DOI: 10.1093/jnci/djw295.. In this regard, a recent study showed that in Asian and Pacific Islander adults who never smoked, lung cancer incidence increased by an average of 2 percent per year between 2007 and 2018, while rates were stable in other US racial and ethnic groups (52)Sakoda LC, et al. (2023) Chest, 164: 785. DOI: 10.1016/j.chest.2023.03.016.. Identification of risk factors, a deep characterization of their disease, and the development of evidence-based early detection and treatments are critical needs to lower the burden of lung cancer in this population of patients who do not have a history of smoking.
While overall cancer incidence in the United States has stabilized in recent years, the incidence of certain cancer types as well as the age- and sex-specific incidence of certain cancers is increasing. For example, the incidence of pancreatic cancer, uterine cancer, and HPV-associated oral cancers has been rising (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024.. While the overall incidence of lung cancer is declining in the United States, young and middle-aged women are being diagnosed at a higher rate than their male counterparts (53)Jemal A, et al. (2023) JAMA Oncol, 9: 1727. DOI: 10.1001/jamaoncol.2023.4415.. Based on a recent study, the decline in lung cancer incidence between 2000–2004 and 2015–2019 was greater in men ages 35 to 54, leading to a higher incidence in women ages 35 to 54 (53)Jemal A, et al. (2023) JAMA Oncol, 9: 1727. DOI: 10.1001/jamaoncol.2023.4415.. This is a reversal of the historical trend of a higher incidence among men and cannot be attributed to smoking prevalence.
Researchers predict that US individuals born between 1965 and 1980 (Generation X) will have a higher incidence of cancer as they turn 60 or older compared to prior generations born between 1908 and 1964 (54)Rosenberg PS, et al. (2024) JAMA Netw Open, 7: e2415731. DOI: 10.1001/jamanetworkopen.2024.15731.. While the reasons are unclear, researchers believe that these increases could be attributable to many factors, including increased prevalence of modifiable risk factors, such as excess body weight, physical inactivity, and environmental pollutants. Additionally, as discussed previously, an increasing concern among public health experts is the rising incidence of early-onset colorectal cancers. Many of the early-onset colorectal cancer cases are also diagnosed at an advanced stage.
Understanding the reasons behind rising cases of early-onset cancers is an area of intensive research. To reduce the burden of early-onset colorectal cancer and early-onset breast cancer, the US Preventive Services Task Force (USPSTF), an independent, volunteer panel of experts in prevention and evidence-based medicine, has updated their screening guidelines to recommend starting colorectal and breast cancer screening at an earlier age of 45 years and 40 years, respectively, instead of the previously recommended starting age of 50 years (see Screening for Early Detection). Researchers are also evaluating new and improved strategies including genetic testing and minimally invasive testing for prevention and early detection of cancers in the younger population (18)Sinicrope FA (2022) N Engl J Med, 386: 1547. DOI: 10.1056/NEJMra2200869..
The Global Burden of Cancer
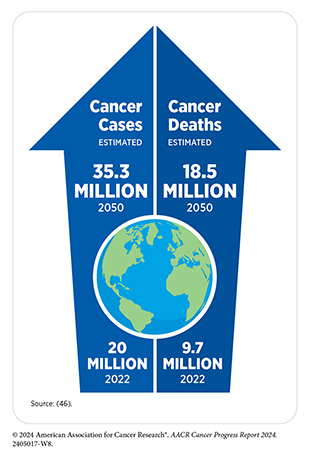
Beyond the United States, cancer is an ongoing global challenge. According to a recent analysis, there were an estimated 20 million new cancer cases and over 9.7 million deaths from cancer in 2022 (55)Bray F, et al. (2024) CA Cancer J Clin, 74: 229. DOI: 10.3322/caac.21834.. An estimated 53.5 million people were alive within 5 years following a cancer diagnosis. Cancers of the lung, breast, colon and rectum, prostate, and stomach are the five most frequently diagnosed cancers worldwide. Diseases accounting for the most cancer deaths globally are cancers of the lung, colon and rectum, liver, breast, and stomach.
There are stark disparities in the cancer burden among countries having different levels of socioeconomic development. Researchers use metrics, such as the human development index (HDI) or the sociodemographic index (SDI), to identify where countries or geographic areas fall on the spectrum of socioeconomic development. SDI quantification considers income per capita, average years of education, and total fertility rate for citizens younger than 25, whereas HDI measurement considers income per capita, average years of education, and life expectancy at birth.
A striking example of global disparities is the burden of breast cancer. In countries with a very high HDI, one in 12 women will be diagnosed with breast cancer in their lifetime and one in 71 women will die of it (55)Bray F, et al. (2024) CA Cancer J Clin, 74: 229. DOI: 10.3322/caac.21834.(56)World Health Organization. Breast Cancer. Accessed: August 7, 2024.. These statistics are significantly worse in countries with a low HDI, where although fewer women are diagnosed (one in 27 women) with breast cancer in their lifetime, there is a much higher likelihood of dying from it (one in 48 women) (55)Bray F, et al. (2024) CA Cancer J Clin, 74: 229. DOI: 10.3322/caac.21834.. One of the drivers of these disparities is the fact that more patients from lower income countries are diagnosed with breast cancer at a later stage compared to higher income countries. According to a new study, up to 30 percent of women with breast cancer in sub-Saharan African countries were diagnosed with late-stage tumors compared to less than 10 percent of women with breast cancer in North America or Europe (57)Benitez Fuentes JD, et al. (2024) JAMA Oncol, 10: 71. DOI: 10.1001/jamaoncol.2023.4837.. Another example of global disparities in cancer burden is the widespread late diagnosis of prostate cancer along with the shortage of specialist surgeons and radiotherapy facilities in lower income countries, leading to worse outcomes for these patients (58)James ND, et al. (2024) Lancet, 403: 1683. DOI: 10.1016/S0140-6736(24)00651-2..
An emerging concern among public health experts is the dramatic rise since the 1990s in the incidence of early-onset cancers, including cancers of the breast, colon, esophagus, kidney, liver, and pancreas, among others, around the world (60)Ugai T, et al. (2022) Nat Rev Clin Oncol, 19: 656. DOI: 10.1038/s41571-022-00672-8.. According to a new analysis of 29 cancer types in 204 countries, the global incidence of early-onset cancers increased by 79 percent and the number of early-onset cancer deaths increased by 28 percent between 1990 and 2019 (61)Zhao J, et al. (2023) BMJ Oncology, 2: e000049. DOI: 10.1136/bmjonc-2023-000049.. Furthermore, the incidence of and deaths from early-onset cancer are projected to increase by 31 percent and 21 percent, respectively, between 2020 and 2030.
Researchers hypothesize that early life exposures to certain cancer risk factors (see Reducing the Risk of Cancer Development) that have become more prevalent in recent decades, including diets rich in highly processed foods, alcohol, tobacco, sedentary lifestyle, obesity, environmental carcinogens, and an unfavorable microbiome, are playing a role in the increased incidence of early-onset cancers. Accordingly, it is critical for each country and region to conduct studies to understand the etiologies of early-onset cancers, and to tailor public health strategies based on the local characteristics and burden of early-onset cancers.
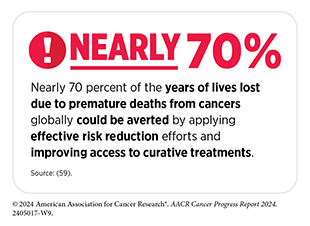
To ensure equitable progress against cancer worldwide, it is imperative that global medical research communities work together and share best practices to implement new and more effective strategies that incorporate local needs and knowledge into tailored national cancer control plans. Additionally, global cancer research funding needs to align with the distribution of cancer burden and treatment availability worldwide.
Public health experts have identified several priorities based on present and future needs of low-resource countries, including reducing the burden of advanced cancers; improving access, affordability, and outcomes of treatment; utilizing value-based care; fostering implementation research; building research capacity; and leveraging technologies to improve cancer control. Global cancer control efforts must also maximize opportunities to reduce the burden of infection-related cancers through prevention and/ or treatment. Robust investment in cancer surgery and radiotherapy research is critical as they still play key roles in curative treatments of many solid tumors (62)McIntosh SA, et al. (2023) Lancet Oncol, 24: 636. DOI: 10.1016/S1470-2045(23)00182-1..
Deploying resources to raise public awareness of cancer prevention and mobilizing key stakeholders worldwide to work with national governments to prioritize vaccination against human papillomavirus (HPV) and hepatitis B virus (HBV) and treatment for hepatitis C virus (HCV) and H pylori can accelerate the pace of progress in reducing the global cancer burden (see Reducing the Risk of Cancer Development). Investments in mitigating modifiable cancer risk factors including smoking, diet, and excess body weight can avert many future cancer diagnoses, leading to immense health and economic benefits globally. The urgent need for robust worldwide investments in cancer science and medicine is further emphasized by recent findings that estimated the cumulative global economic burden of cancer from 2020 to 2050 to be at an enormous $25.2 trillion (63)Chen S, et al. (2023) JAMA Oncol, 9: 465. DOI: 10.1001/jamaoncol.2022.7826..
Funding Cancer Research: A Vital Investment
The immense toll of cancer is felt both in the number of lives it affects each year and its economic impact. The direct medical costs of patient care are one measure of the financial impact of cancer, and in the United States alone, these costs were estimated to be nearly $209 billion in 2020 (2)American Cancer Society. Cancer Facts and Figures 2024. Accessed: July 10, 2024.. Unfortunately, these numbers stand in stark contrast to the NCI budget of $6 billion for the same year. Notably, the direct medical costs do not include the indirect costs of lost productivity due to cancer-related morbidity and mortality, which are also extremely high. As one example, the costs of lost productivity for US AYA patients diagnosed with cancer in 2019 were an estimated $18 billion over their lifetime (64)Parsons SK, et al. (2023) J Clin Oncol, 41: 3260. DOI: 10.1200/JCO.22.01985..
Patients with cancer shoulder a large amount of the economic burden associated with cancer care. In 2019, in the United States, patients with cancer lost nearly $5 billion due to time costs—the value of time that patients spend traveling to and from health care, waiting for care, and receiving care—and paid an estimated $16.2 billion in out-of-pocket costs for cancer care (65)Kuehn BM (2021) JAMA, 326: 2251. DOI: 10.1001/jama.2021.21119..
With the number of cancer cases projected to increase in the coming decades, it is likely that both direct and indirect costs will escalate. According to a recent report, the economic burden of cancer in the United States will reach $5.3 trillion over the next three decades (63)Chen S, et al. (2023) JAMA Oncol, 9: 465. DOI: 10.1001/jamaoncol.2022.7826.. The rising personal and economic burden of cancer underscores the urgent need for more research that will accelerate the pace of progress and curb the increasing burden of cancer.
Recent advances in cancer prevention, detection, and treatment, many of which are highlighted in this report and the 13 prior editions, were made as a direct result of the cumulative efforts of researchers from across the spectrum of cancer science and medicine. Much of their work, as well as that of FDA and CDC, is supported by funds from the federal government. Public sector funding from NIH and NCI contributes significantly to the development of novel anticancer drugs (66)Nayak RK, et al. (2021) JAMA Intern Med, 181: 1522. DOI: 10.1001/jamainternmed.2021.3720.(67)Galkina Cleary E, et al. (2023) JAMA Health Forum, 4: e230511. DOI: 10.1001/jamahealthforum.2023.0511.. The rapid pace of approval of cutting-edge precision cancer medicine, many of which were evaluated in NCI-funded clinical trials, has transformed the treatment landscape and dramatically improved patient outcomes. Researchers estimate that over the past 40 years, patients with cancer in the United States have gained 14 million years of additional life because of NCI-funded clinical trials (68)Unger JM, et al. (2023) J Clin Oncol, 41: 2020. DOI: 10.1200/Jco.22.01826.. Therefore, the vital importance of federal investments in medical research in driving progress against cancer and saving lives cannot be overstated.
The consecutive increases in the NIH budget over the past decade have helped maintain the momentum of progress against cancer and other diseases. Additionally, NIH research grants help sustain the US economy. In fiscal year (FY) 2023, the $37.81 billion awarded to researchers in the 50 US states and the District of Columbia supported 412,041 new jobs and yielded $92.89 billion in economic activity (see Investments in Research for a Healthier Future). Furthermore, robust funding for NIH helps ensure that the United States continues to be a global leader in medical research and innovation.
The decline in NIH funding in FY 2024 compared to FY 2023 and the uncertainty of the current budgetary environment as the FY 2025 appropriations unfold is therefore of grave concern to the medical research community. A lack of funding may deter early-stage scientists and those from racial or ethnic minority and other underrepresented population groups from choosing academic research as their career paths, which will impede progress against cancer.
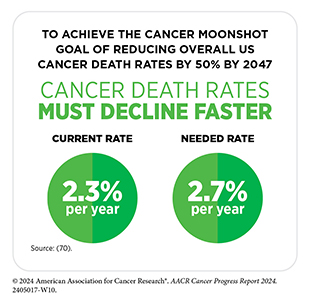
It is imperative that in the years ahead, Congress continues to provide sustained, robust, and predictable increases in investments in the federal agencies that fuel progress against cancer, in particular, NIH, NCI, FDA, and CDC (see AACR Call to Action). Such investments will help the medical and public health research community sustain the momentum of scientific and technological innovation and will accelerate the pace of progress against cancer to achieve the President’s Cancer Moonshot goal of reducing US cancer death rates by at least 50 percent by the year 2047, supported by policymakers like The Honorable Jamie Raskin.
Next Section: Understanding the Path to Cancer Development Previous Section: Snapshot of a Year in Progress