Supporting Cancer Patients and Survivors
In this section, you will learn:
- As of January 2022, the most recent year for which such data are available, there were more than 18 million people living in the U.S. with a history of a cancer diagnosis and this number is expected to rise to 26 million by 2040.
- A cancer diagnosis has a lasting impact on survivors that brings a host of challenges including numerous short- and long-term side effects related to cancer and its treatments.
- Children, adolescents and young adults, and older adults who have survived cancer face unique and/or exacerbated challenges.
- Physical activity, a healthy diet, and smoking cessation are all proven ways to improve survival and quality of life.
- Patient navigators, clinical care coordinators, and patient advocates can enhance patient outcomes by improving a cancer survivor’s mental and physical health.
According to NCI, a person is considered a cancer survivor from the time of cancer diagnosis through the balance of his or her life. Each person diagnosed with cancer has a unique experience ranging from successful treatment and living cancer free for the remainder of life to experiencing varying degrees of side effects and/or a subsequent cancer diagnosis with the same or a different type of cancer.
Unprecedented advances in cancer treatments over the past decade have led to more patients living longer and fuller lives after a cancer diagnosis. As of 2022, the most recent year for which such data are available, there are 18.1 million people living with a history of a cancer diagnosis, which equates to about five percent of the U.S. population (7)Miller KD, et al. (2022) CA Cancer J Clin, 0: 1. [LINK NOT AVAILABLE]. This is a significant improvement from 50 years ago when cancer survivors constituted only 1.4 percent of the U.S. population. The number of survivors is expected to grow to 26 million by 2040. Understanding and addressing the short- and long-term challenges faced by cancer survivors, supporting their quality of life, and ensuring that care is accessible and equitable are important priorities in cancer survivorship research (7)Miller KD, et al. (2022) CA Cancer J Clin, 0: 1. [LINK NOT AVAILABLE].
A cancer diagnosis also impacts friends, family members, and caregivers, who are often the main support network for the survivor. This necessitates widening the focus of research, support, and care beyond the cancer patient and survivor to include individuals who make up the support structure.
The following section highlights the challenges faced by cancer survivors and their support network, strategies to improve quality of life, and approaches that have been shown to deliver care most effectively.
Challenges Faced by Cancer Survivors
Cancer survivors often face physical, psychosocial, and financial challenges throughout their survivorship journey. The number of cancer survivors living with a functional limitation, defined as difficulty performing any of 12 routine physical or social activities without assistance (e.g., sitting for more than two hours or participating in social activities) more than doubled from 3.6 million in 1999 to 8.2 million in 2018 (558)Patel VR, et al. (2023) JAMA Oncol, 9: 1001. [LINK NOT AVAILABLE]. The functional limitations can vary based on the type of cancer diagnosed and were highest among survivors of pancreatic cancer (80.3 percent) and lung cancer (76.5 percent) and lowest for those who had melanoma (62.2 percent), or cancers of breast (61.8 percent) and prostate (59.5 percent) (558)Patel VR, et al. (2023) JAMA Oncol, 9: 1001. [LINK NOT AVAILABLE].
While cancer researchers and physicians have learned a lot about these challenges over the years, implementation of groundbreaking new treatments, such as immunotherapies, presents unique short- and long-term challenges that are only beginning to be understood (see Immunotherapy: Pushing the Frontier of Cancer Medicine). A greater understanding of these challenges and ways to address them is urgently required to support cancer survivors.
Physical Challenges
Survivors can experience a wide range of short- and long-term symptoms caused by cancer or its treatments. Short-term effects include hair loss, pain, nausea, vomiting, and loss of smell and appetite with varying severity of symptoms depending on the person, cancer type, and treatment. As cancer survivors are living longer due to better therapies, the development of long-term side effects such as heart damage (cardiotoxicity), lung damage, loss of bone density, and cognitive decline is becoming more common and demands a greater understanding to reduce or manage these conditions (see Sidebar 42).
Cachexia is the loss of body weight and muscle mass, and weakness that may occur in patients with cancer or other chronic diseases. Cachexia is estimated to occur in up to 80 percent of patients with advanced cancer. For instance, cachexia occurs in 87 percent of patients with pancreatic and gastric cancers, and in 61 percent of patients with NHL or with cancers of the colon and rectum, lung, and prostate. The development of cachexia indicates poor prognosis and accounts for 20 to 30 percent of all cancer-related deaths. Loss of muscle, especially heart and skeletal muscle, leads to widespread disturbances in biological functions (559)Ni J, et al. (2020) Cancer Manag Res, 12: 5597. [LINK NOT AVAILABLE]. In patients with metastatic cancer, who are at the highest risk for cachexia, reduced nutrient intake coupled with high energy demand caused by cancer and its side effects results in a negative energy balance. In some instances, pain management can help to increase appetite, which can slow the advancement of cachexia (560)Law ML (2022) Front Pain Res (Lausanne), 3: 971295. [LINK NOT AVAILABLE]. Understanding the biological underpinnings and addressing cancer-related cachexia are areas of ongoing basic and clinical investigation (561)National Cancer Institute. Treating Cancer Cachexia: Progress Looks Possible. Accessed: July 5, 2023. .
Chemotherapy-related cognitive impairment, often termed as “chemo brain,” has been reported by many cancer survivors to describe thinking and memory problems before, during, and after cancer treatment. Accumulating evidence from brain imaging studies shows the biological effects of cancer therapeutics on the brain, including changes in glucose consumption, blood flow, and expression of certain proteins (562)Chiaravalloti A, et al. (2023) J Nucl Med, 64: 508. [LINK NOT AVAILABLE], all of which may contribute to cognitive impairment. Many survivors report having increased cognitive impairment even after a year following the completion of cancer treatment, indicating these effects can be long-standing (563)Lange M, et al. (2023) J Natl Cancer Inst, 115: 322. [LINK NOT AVAILABLE].
Cardiotoxicity from certain types of anticancer therapeutics has been reported in many studies and increases the risk of clinical hypertension, coronary artery disease, heart failure, and atrial fibrillation, among others. Research has also shown that cancer survivors have an “excess heart age”—a measure of cardiovascular damage and risk of a heart attack—compared to individuals who have never received a cancer diagnosis. Studies of cancer survivors have shown an excess heart age of eight and a half years in men and six and a half years in women (564)Scott LC, et al. (2021) MMWR Morb Mortal Wkly Rep, 70: 1. [LINK NOT AVAILABLE]. Furthermore, there are disparities in severity of adverse cardiac events among cancer survivors. Non-Hispanic Black cancer survivors had higher rates of cardiovascular disease-related mortality compared to Hispanic, non-Hispanic Asian/Pacific Islander, and White patients (565)Zhu C, et al. (2023) JACC CardioOncol, 5: 55. [LINK NOT AVAILABLE].
Immunotherapies, including immune checkpoint inhibitors and adoptive cell therapies, are still a relatively new class of treatment compared to other types of cancer therapies. Their long- and late-term side effects are being studied as successful treatment with these therapeutics has led to many more people living longer (see Immunotherapy: Pushing the Frontier of Cancer Medicine, p. 99).
Psychosocial Challenges
A diagnosis of cancer can pose serious challenges to a person’s mental and emotional health. Based on recent data, one in six patients with cancer has pre-existing psychiatric conditions, which can lead to longer hospital stays, higher rates of readmission, and increased risk of suicidal thoughts after the treatment ends in patients undergoing surgery for their cancer (567)Bryan CJ, et al. (2023) JAMA Oncol, 9: 303. [LINK NOT AVAILABLE]. Many survivors experience anxiety (7 to 21 percent of patients), depression (8 to 24 percent of patients), and distress (25 to 41 percent of patients) following the completion of cancer treatment (13,568-570). A study that examined 26 different cancer types found that 98 percent of patients with testicular cancer, 78 percent of patients with cervical cancer, and 69 percent of patients with Hodgkin lymphoma experienced a depressive event (570)Chang WH, et al. (2022) Nat Med, 28: 860. [LINK NOT AVAILABLE]. Psychological distress is more prevalent among those who are AYA or belong to a racial and ethnic minority (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2023. (568)Rincones O, et al. (2021) Cancer Manag Res, 13: 3803. [LINK NOT AVAILABLE](569)Papini C, et al. (2023) Cancer, 129: 1117. [LINK NOT AVAILABLE](570)Chang WH, et al. (2022) Nat Med, 28: 860. [LINK NOT AVAILABLE]. Those who belong to sexual and gender minority populations are also at a greater risk of having lower psychological well-being, which is exacerbated in cancer patients living with HIV (571)Chan ASW, et al. (2022) Front Public Health, 10: 912980. [LINK NOT AVAILABLE].
Controlling depression can improve survival, with a recent study showing that 1-year survival in patients with cancer whose depression symptoms improved was 64 percent versus only 42 percent for those whose symptoms worsened (573)Andersen BL, et al. (2022) Psychosom Med, 84: 215. [LINK NOT AVAILABLE]. Emerging evidence suggests that the level of depression directly correlates with the degree of systemic inflammation in patients with cancer as measured by immune system markers, such as levels of cytokine or certain immune cells (574)Andersen BL, et al. (2023) PLoS One, 18: e0282206. [LINK NOT AVAILABLE](575)Breitbart W, et al. (2014) Psychooncology, 23: 339. [LINK NOT AVAILABLE](576)McFarland DC, et al. (2022) Cancer, 128: 2504. [LINK NOT AVAILABLE]. For example, patients with lung cancer with moderate to severe depression were two to three times more likely to have inflammation levels that predict poor survival rates. Immune system dysregulation may also lead to a poor response of these patients to immunotherapies, which rely on a functional immune system to be effective.
Financial Challenges
Financial toxicity refers to the financial hardship associated with cancer treatment and management. Evidence indicates that cancer survivors who experience financial toxicity such as difficulty paying for prescriptions, mental health care, and other health services, and/or who delay medical care due to cost, are also at greater risk of mortality, regardless of insurance status (578)Yabroff KR, et al. (2022) J Natl Cancer Inst, 114: 863. [LINK NOT AVAILABLE].
Financial toxicity is pervasive and is, in part, exacerbated by the rising cost of cancer care (480)Jenkins RW, et al. (2018) Br J Cancer, 118: 9. [LINK NOT AVAILABLE]. For instance, between 2009 and 2016, the average cost of treatment increased 29 percent for breast cancer, 11 percent for lung cancer, and four percent for prostate cancer. In addition, out-of-pocket costs have also increased by 15 percent for all patients with cancer (579)Shih YT, et al. (2022) J Natl Cancer Inst, 114: 1392. [LINK NOT AVAILABLE].
Survivors can face challenges maintaining a job or going back to a previous job after the conclusion of treatment. Cancer survivors between the ages of 50 and 64 years were more likely to have a work-limiting disability and less likely to be employed, equating to 505,768 fewer employed individuals between 2010 and 2016 (580)Grabowski DC, et al. (2023) JAMA Netw Open, 6: e2315823. [LINK NOT AVAILABLE].
Apart from direct financial costs, it is also common for cancer survivors to have housing, food, and transportation insecurity. As a result of these challenges, patients may forgo, miss, delay, alter, and/or prematurely terminate necessary care (582)Graboyes EM, et al. (2022) J Natl Cancer Inst, 114: 1593. [LINK NOT AVAILABLE](583)Fan Q, et al. (2022) J Natl Cancer Inst, 114: 1584. [LINK NOT AVAILABLE](584)Raber M, et al. (2022) J Natl Cancer Inst, 114: 1577. [LINK NOT AVAILABLE]. Food insecurity is pervasive among people navigating a cancer diagnosis, with anywhere between 17 and 55 percent of patients with cancer facing food insecurity (584)Raber M, et al. (2022) J Natl Cancer Inst, 114: 1577. [LINK NOT AVAILABLE]. This may explain why cancer survivors are more likely to be on supplemental nutrition assistance programs (SNAP) than the general population (580)Grabowski DC, et al. (2023) JAMA Netw Open, 6: e2315823. [LINK NOT AVAILABLE].
Caregivers of patients with cancer are also susceptible to many of the same challenges faced by the patients. Lost income due to taking time off or leaving their employment can increase susceptibility to financial toxicity. For instance, 68.1 percent of partners of those diagnosed with colorectal cancer reported adverse financial outcomes following diagnosis, which led to worsening of health-related quality of life for these caregivers (585)Ghazal LV, et al. (2023) JAMA Netw Open, 6: e235897. [LINK NOT AVAILABLE]. Another study found that cancer caregivers from lower socioeconomic backgrounds were more likely to increase debt and incur work loss compared to noncancer caregivers in similar households (586)Bradley CJ, et al. (2023) J Clin Oncol, 41: 2939. [LINK NOT AVAILABLE].
Unique Challenges Faced by Vulnerable Patient Populations
Children
Pediatric or childhood cancers are those diagnosed from birth until the age of 14 years. In the United States in 2023, an estimated 9,910 new cases of cancer will be diagnosed among children. Thanks to major treatment advances, 85 percent of children are expected to live five years or more after a cancer diagnosis. This is a marked improvement compared to the mid-1970s, when only 42 percent of children lived beyond five years after a cancer diagnosis (587)Siegel RL, et al. (2021) CA Cancer J Clin, 71: 7. [LINK NOT AVAILABLE]. Because childhood cancer survivors are diagnosed at a young age, they will be living longer postdiagnosis than an adult who has been diagnosed with cancer.
The degree and type of late-stage side effects childhood cancer survivors develop depend on a variety of reasons, including the type and stage of cancer at the time of diagnosis, the type and dose of treatment, and the age and general health of the patient at the time of treatment. Reports indicate that 60 to 90 percent of childhood survivors develop one or more chronic health conditions following their cancer diagnosis (588)Armstrong GT, et al. (2014) J Clin Oncol, 32: 1218. [LINK NOT AVAILABLE](589)Hudson MM, et al. (2013) JAMA, 309: 2371. [LINK NOT AVAILABLE].
Pediatric patients who receive chemotherapeutics are at an increased risk of developing hearing loss, also called ototoxicity. One study found that 75 percent of children under five and 48 percent of children over five who were treated with cisplatin had hearing loss related to their treatment (590)Meijer AJM, et al. (2022) Cancer, 128: 169. [LINK NOT AVAILABLE]. In September 2022, FDA approved sodium thiosulfate to reduce the risk of hearing loss associated with the chemotherapeutic cisplatin in pediatric patients one month and older. Sodium thiosulfate reduced the risk of cisplatin-associated hearing loss by almost 60 percent compared to those who did not receive the drug ((591)Schulte F, et al. (2022) JAMA Netw Open, 5: e2227225. [LINK NOT AVAILABLE]. By preventing ototoxicity, this approval will help many pediatric cancer survivors experience a better quality of life.
Pediatric cancer survivors are also more susceptible to premature aging. According to one study, daily functional limitations, psychosocial symptoms, and health conditions of a 30-year-old cancer survivor are similar to those of a 63-year-old healthy individual (593)Williams AM, et al. (2023) J Natl Cancer Inst, 115: 200. [LINK NOT AVAILABLE].
While premature aging and cancer is an emerging research area, new evidence implicates changes in the epigenome that occur after treatment with cancer therapies as a contributing factor. In one study that evaluated changes in the epigenome of adult survivors of childhood cancers, researchers identified epigenetic patterns that are normally found in much older individuals. These changes were directly associated with the development of early-onset obesity, chronic health conditions, and higher risk of dying within 5 years (594)Plonski NM, et al. (2023) JAMA Netw Open, 6: e2310325. [LINK NOT AVAILABLE].
The quality of mental health among survivors of childhood cancers is also concerning. When compared to their healthy siblings, young adult survivors of childhood cancers reported increased loneliness that subsequently increased anxiety, depression, and the likelihood of smoking. Long-term follow-up with these patients found higher levels of suicidal thoughts, and heavy/risky alcohol consumption (569)Papini C, et al. (2023) Cancer, 129: 1117. [LINK NOT AVAILABLE]. This population is also more susceptible to major mental health illnesses, including autism, attention deficit disorder, bipolar disorder, major depressive disorder, obsessive-compulsive disorder, and posttraumatic stress disorder, with the greatest number of mental health illnesses experienced by survivors of brain and lymphatic/ hematopoietic tissue cancers (595)Hsu TW, et al. (2023) J Clin Oncol, 41: 2054. [LINK NOT AVAILABLE].
Adolescents and Young Adults
Adolescent and young adult (AYA) cancer survivors are those diagnosed between the ages of 15 and 39. Based on estimates of new cancer cases in 2023, 4.4 percent of all new cases will be in AYA and 85.8 percent of AYAs diagnosed with cancer will live 5 years or more after their diagnosis (596)National Cancer Institute. Cancer Among Adolescents and Young Adults (AYAs). Accessed: Jul 5, 2023. . This population group faces unique personal, social, and emotional challenges.
Many AYA survivors experience long-term side effects and are at a two- to three-fold higher risk of premature ovarian failure, chronic liver disease, renal failure and cardiovascular disease compared to those with no diagnosis of cancer (597)Chao C, et al. (2020) J Clin Oncol, 38: 3161. [LINK NOT AVAILABLE].
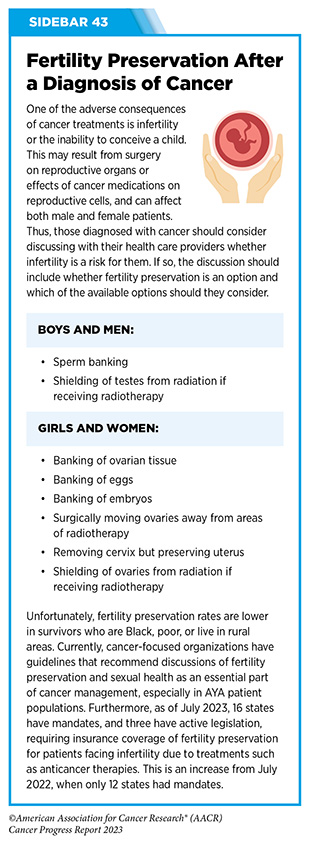
Between 44 and 86 percent of AYA survivors have concerns regarding how treatments for cancer, including surgery, radiotherapy, and cytotoxic chemotherapy, may lead to infertility, which is the inability to conceive a child (598)Xie J, et al. (2022) Cancer Med, 11: 3508. [LINK NOT AVAILABLE]. The possibility of impaired reproductive abilities may lead some patients to store reproductive material through the process of fertility preservation (see Sidebar 43). Participation in fertility preservation and the type of preservation should be decided by the individual after discussions with his or her health care providers.
Receiving a diagnosis of cancer during pregnancy, which may occur for AYAs, raises questions about how cancer treatment may affect both the mother and the developing embryo or fetus; about one in 2,000 pregnancies is complicated by cancer according to estimates (600)Stensheim H, et al. (2009) J Clin Oncol, 27: 45. [LINK NOT AVAILABLE]. The risk to mother or offspring from cancer or the treatment of cancer is mixed and is dependent on a multitude of factors such as age, cancer type, stage of cancer, the trimester at diagnosis, and therapy type received (601)Jorgensen K, et al. (2022) Obstet Gynecol, 140: 939. [LINK NOT AVAILABLE](602)Betts AC, et al. (2023) J Natl Cancer Inst, 115: 619. [LINK NOT AVAILABLE](603)Anderson C, et al. (2017) JAMA Oncol, 3: 1078. [LINK NOT AVAILABLE].
AYAs also have worse mental health outcomes compared to those without a diagnosis of cancer. AYA cancer survivors had an 80 percent increased risk of hospitalizations for mental health illnesses and were 4.5 times more likely to purchase antidepressants compared to their siblings (605)Ryder-Burbidge C, et al. (2021) Cancers (Basel), 13. [LINK NOT AVAILABLE]. Furthermore, a subset of AYA survivors is at risk for early death, with those diagnosed with hematologic malignancies facing the highest risk (606)Berkman AM, et al. (2023) J Natl Cancer Inst, 115: 447. [LINK NOT AVAILABLE].
Financial toxicity among AYA cancer survivors is also higher compared to those with no diagnosis of cancer. One study reported that the costs associated with a diagnosis of cancer are substantial, reaching an average of $259,324 per person over their lifetime. One reason is that a cancer diagnosis often affects these individuals when they are just beginning higher levels of education or starting careers, potentially impacting productivity and well-being (54)Parsons SK, et al. (2023) J Clin Oncol, 41: 3260. [LINK NOT AVAILABLE].
The Affordable Care Act (ACA) resulted in improved insurance coverage. Evidence is emerging that states which expanded Medicaid under the ACA had improved overall survival among young adults with cancer, specifically among racial or ethnic minorities when compared to states that did not expand Medicaid benefits (608)Ji X, et al. (2023) J Clin Oncol, 41: 1909. [LINK NOT AVAILABLE].
Older Adults
Older adults are defined as those age 65 and over, representing 64 percent of cancer survivors in the United States. This population is also the fastest growing and is projected to increase to 73 percent of cancer survivors by 2040 (609)Mohile SG, et al. (2016) Cancer, 122: 2459. [LINK NOT AVAILABLE].
Cachexia is common among older cancer survivors, especially among those with gastrointestinal cancers; an estimated 52 to 65 percent of older cancer survivors develop cachexia (610)Poisson J, et al. (2021) J Cachexia Sarcopenia Muscle, 12: 1477. [LINK NOT AVAILABLE](611)Dunne RF, et al. (2019) J Geriatr Oncol, 10: 415. [LINK NOT AVAILABLE]. Specifically, loss of muscle mass and strength, called sarcopenia, occurs in 12.5 to 57.7 percent of adult cancer survivors (612)Cruz-Jentoft AJ, et al. (2019) Age Ageing, 48: 16. [LINK NOT AVAILABLE](613)Fukuda Y, et al. (2016) Gastric Cancer, 19: 986. [LINK NOT AVAILABLE](614)Wang SL, et al. (2016) Ann Surg Oncol, 23: 556. [LINK NOT AVAILABLE](615)Tegels JJ, et al. (2015) J Surg Oncol, 112: 403. [LINK NOT AVAILABLE].
Fracture risk due to bone density loss (osteoporosis) is becoming another increasing concern in this demographic. In one study of older adults with a mean age of 69 years, researchers found that cancer survivors diagnosed within the last five years had two times the risk of bone fracture compared to those with no history of cancer. It is important to note that higher fracture risk was positively associated with current smoking status (616)Rees-Punia E, et al. (2023) JAMA Oncol, 9: 79. [LINK NOT AVAILABLE]. Older adults may benefit from programs, such as physical therapy and smoking cessation, that are shown to reduce the risk of fracture (617)Campbell KL, et al. (2022) JCO Oncol Pract, 18: e697. [LINK NOT AVAILABLE].
Research into older cancer survivors and their unique risks is important as the U.S. population ages, life expectancy increases, and cancer survivorship rises.
Improving Health-related Quality of Life and Outcomes
Promoting Healthy Behaviors
Healthy behaviors, such as physical activity, a healthy diet, reduced alcohol consumption, and smoking cessation, can significantly improve both health outcomes and health-related quality of life (HRQOL) for cancer survivors. In fact, it is increasingly appreciated that adopting healthy behaviors after a diagnosis of cancer but prior to beginning cancer treatment, called prehabilitation or “prehab” can significantly improve outcomes for patients. A patient who is healthy at the start of treatment can undergo higher doses of drug, is less susceptible to certain side effects, and has an immune system that is primed to fight cancer better.
Physical activity has been shown to increase survival and lower recurrence of cancers (618)Brown JC, et al. (2023) Br J Sports Med, 57: 965. [LINK NOT AVAILABLE]. Physical activity changes how organs and tissues function to resist both cancer progression and/or metastasis. Because the body requires energy (in the form of carbohydrates, such as glucose), increasing physical activity levels increases the demand for energy from organs. One study found that by increasing physical activity levels, the amount of energy that was available to tumors was reduced because it was needed by the rest of the body during physical activity. Participants who were more active had lower rates of metastatic progression compared to those who were not active (175)Sheinboim D, et al. (2022) Cancer Res, 82: 4164. [LINK NOT AVAILABLE].
Physical activity can also improve treatment outcomes. A meta-analysis of breast cancer survivors who underwent curative treatment found that frequent physical activity improved HRQOL, cardiorespiratory fitness, and body composition (619)Joaquim A, et al. (2022) Front Oncol, 12: 955505. [LINK NOT AVAILABLE]. A second study showed that in a group of patients who underwent radiotherapy for breast cancer, biweekly aerobic exercise sessions of 30 to 40 minutes each significantly improved cancer-related fatigue and HRQOL (620)Mavropalias G, et al. (2023) Breast Cancer, 30: 139. [LINK NOT AVAILABLE].
Research has shown that sustaining a healthy diet that consists of whole grains, fruits, and vegetables can increase survival from cancer and reduce the risk of cancer recurrence (622)Morice P, et al. (2012) Lancet, 379: 558. [LINK NOT AVAILABLE]. Cancer survivors who adhere to a high-quality, balanced diet have better quality of life, mental well-being, and survival (623)Deshmukh AA, et al. (2018) JNCI Cancer Spectr, 2: pky022. [LINK NOT AVAILABLE](624)Schwedhelm C, et al. (2016) Nutr Rev, 74: 737. [LINK NOT AVAILABLE](625)Castro-Espin C, et al. (2022) Nutrients, 14. [LINK NOT AVAILABLE](626)Liu ZY, et al. (2022) J Transl Med, 20: 376. [LINK NOT AVAILABLE]. Diet is also important for maintaining a healthy gut microbiome, which is the collection of organisms that occupy the intestines and aid in digestion (see Targeting the Microbiome in Cancer Treatment).
Smoking among cancer survivors is associated with poor outcomes and greater treatment-related complications, higher risk of secondary cancers, and greater mortality (123)The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA)2014. [LINK NOT AVAILABLE]. Smoking cessation is a crucial intervention that can improve clinical outcomes during and after the completion of cancer treatment (627)Wang X, et al. (2023) JAMA Netw Open, 6: e2311966. [LINK NOT AVAILABLE]. Many cancer-focused professional organizations strongly recommend smoking cessation after a cancer diagnosis. Evidence demonstrates that the most successful methods include involving a trained tobacco specialist who can screen patients and assist them in achieving abstinence; improving clinician education on how to deal with and refer patients appropriately; and building relationships with implementation stakeholders (628)Young AL, et al. (2023) JAMA Oncol, 9: 981. [LINK NOT AVAILABLE].
Integrating Palliative Care
Palliative care is an approach to prevent or treat the symptoms and side effects of any disease, including cancer, by addressing the physical, psychosocial, financial, and spiritual needs that arise from the disease and treatments (see Sidebar 44). Palliative care is facilitated by multidisciplinary teams of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers and has been shown to improve quality of life for patients, families, and caregivers.
Studies show that integration of palliative care through consultation with a palliative care team early on after cancer diagnosis is most effective in improving HRQOL, increasing satisfaction with care, and mitigating depression (629)Bakitas M, et al. (2009) JAMA, 302: 741. [LINK NOT AVAILABLE](630)Zimmermann C, et al. (2014) Lancet, 383: 1721. [LINK NOT AVAILABLE](631)Temel JS, et al. (2010) N Engl J Med, 363: 733. [LINK NOT AVAILABLE]. For patients with advanced cancers, including those with solid and blood cancers, ongoing consultation with a palliative care specialist throughout treatment led to improved communication between patients, caregivers, and the clinical care team leading to an overall increase in life expectancy (632)Bigi S, et al. (2023) Front Public Health, 11: 1092145. [LINK NOT AVAILABLE].
Palliative therapy, which aims to relieve symptoms of cancer through surgical or therapeutic intervention, can also improve quality of life for patients. As one example, patients with gastric cancers, who develop complications in advanced stages of the disease, can benefit from gastric resection, gastrojejunostomy, stenting, chemotherapy, and radiotherapy, which reduce gastric obstruction and bleeding, and improve patient quality of life (633)Luo XF, et al. (2023) Front Oncol, 13: 1104447. [LINK NOT AVAILABLE].
Improving Mental Health
The psychological challenges faced by survivors of cancer necessitate approaches that improve the mental well-being of this population (see Challenges Faced by Cancer Survivors). Psycho-oncology is an interdisciplinary subspeciality within the cancer care continuum that aims to address the physical, behavioral, emotional, and psychosocial distress that arises for cancer survivors and their caregivers. Experts who are trained in psycho-oncology apply a holistic approach to destigmatize and address behavioral and psychosocial distress that is often caused by a cancer diagnosis and treatments (see Sidebar 45).
With the increased use of telehealth in oncology care (see Sidebar 29), researchers are studying the effectiveness of bringing psycho-oncology practices like cognitive behavioral therapy and mindfulness stress reduction, as well as other interventions to survivors at their homes. In one clinical trial, researchers developed a smartphone app for breast cancer survivors to help reduce anxiety surrounding cancer recurrence. The group who had access to the smartphone app saw reduced recurrence-related anxiety after eight weeks compared to those who did not have access to the app (636)Akechi T, et al. (2023) J Clin Oncol, 41: 1069. [LINK NOT AVAILABLE]. These types of technologies offer effective ways to help bring psycho-oncology care to patients, especially because currently there are a limited number of psychotherapists available for the growing number of cancer survivors.
Researchers are also trying to understand how survivors of cancer experience posttraumatic growth, which describes positive life changes that can develop because of traumatic and stressful events, such as a diagnosis of cancer (see Sidebar 46). Posttraumatic growth may lead to perceptions of new possibilities, closer relationships with family and friends, development of personal strength, spiritual development, and a greater appreciation for life (637)Fu X, et al. (2022) Front Public Health, 10: 927370. [LINK NOT AVAILABLE]. Although the concept of posttraumatic growth is not new, its potential is just beginning to be appreciated within the cancer care community. The most influential factors that affect posttraumatic growth include the level of social support and the use of various coping strategies among survivors of cancer.
Delivering Care to Cancer Survivors
Coordinating Care
The multifaced approach to treating cancer necessitates providing survivors with appropriate care to address their many needs including transitioning from active treatment, coordinating follow-up appointments, addressing financial needs, and gaining access to other survivorship resources. While these resources are often available, understanding how or where to gain access to them can be challenging. Coordination of care is critically important to help patients identify and gain access to such resources.
Coordinating cancer care is most effective when a designated individual or a team of people helps a cancer patient or survivor to gain access to the resources they need. A systemic review of over 30 years of studies found that coordination approaches led to improvements among 81 percent of survivors across multiple facets of cancer care, including screening, patient experience, and quality of end-of-life care (642)Gorin SS, et al. (2017) Ann Behav Med, 51: 532. [LINK NOT AVAILABLE].
Patient navigators and clinical care coordinators are individuals who help cancer patients and survivors access resources more effectively (see Sidebar 47). Furthermore, patient advocates, who are often cancer survivors themselves, are uniquely positioned to bridge critical gaps between patients, survivors, and the health care system.
Financial navigators can help reduce financial toxicity among survivors and their caregivers. These navigators can screen patients to determine if they are at an increased risk of financial toxicity and can provide assistance and resources. One study that implemented financial navigators for patients with hematologic cancer and their caregivers found that the program secured an average of $2,500 in financial benefits for each participant (643)Edward JS, et al. (2023) JCO Oncol Pract, 19: e696. [LINK NOT AVAILABLE].
Patient reported outcomes (PROs), which are reports given by patients on their status that have not been interpreted by a clinician or anyone else, are being used in connection with the patient experience, particularly among those participating in clinical trials (see Sidebar 48). Incorporating the patient’s perspective to understand treatment tolerability and efficacy is increasingly implemented in clinical trials and will improve the cancer treatment experience for patients in the real world (649)Basch E, et al. (2023) J Clin Oncol, 41: 3724. [LINK NOT AVAILABLE]. PROs are collected through questionnaires, which alert clinicians to the status of the patient regarding health-related quality of life, symptoms, and health-related behaviors (e.g., smoking, diet, physical activity) (650)Friends of Cancer Research. Broadening the Definition of Tolerability in Cancer Clinical Trials to Better Measure the Patient Experience. Accessed: July 31, 2023. . Patients engaged in monitoring their symptoms may have improved clinical outcomes and reduced risk of emergency room and hospital visits compared to those who do not complete these questionnaires (651)Natori A, et al. (2023) J Clin Oncol, 41: 285. [LINK NOT AVAILABLE](652)Thanarajasingam G, et al. (2022) Lancet Haematol, 9: e374. [LINK NOT AVAILABLE]. Integration of real-world electronic health records with PRO assessments that provide automated alerts to clinicians will help improve patient outcomes.
Technologies that improve access to care, such as telemedicine (see Sidebar 29) and smartphone apps, have become essential tools used by physicians, care teams, and patients. Increasingly, phone apps are being utilized by health care systems to assist with oncology support, treatment adherence, and follow-up care. Clinical trials of these apps are ongoing; however, preliminary evidence shows that they are utilized by patients and help improve the survivorship experience during and after treatment (653)Temple-Oberle C, et al. (2023) JAMA Surg, 158: 693. [LINK NOT AVAILABLE](654)Graetz I, et al. (2023) Cancer Med, 12: 6190. [LINK NOT AVAILABLE](655)Villanueva-Bueno C, et al. (2022) Front Public Health, 10: 978783. [LINK NOT AVAILABLE].
Supporting Caregivers
Caregivers comprise family members or friends who help patients with long-term chronic illness and manage any and all aspects of their care. One in five U.S. adults (ages 18 to 64), accounting for over 53 million people, provided care for another person in 2020, a significant increase from 43.5 million in 2015 (656)National Partnership for Women and Families. Paid leave could keep more than 6 million caregivers connected to the labor force by 2030. Accessed: June 30, 2023. . It is further estimated that four million of these caregivers are caring for an adult cancer patient. More evidence of the challenges faced by caregivers is becoming clear, and there are many opportunities to assist this vulnerable population.
Survivors require many resources that are often provided by their caregivers including arranging transportation, helping with day-to-day activities such as doctor visits, providing medical care or other clinical tasks, coordinating care, and giving emotional support. This often leads to caregivers deferring their own health care. One report shows that caregivers who are actively taking care of a family member were less likely to seek medical care including physician and emergency room visits (657)Hess LM, et al. (2021) BMC Health Serv Res, 21: 894. [LINK NOT AVAILABLE]. This is especially concerning among Black and Hispanic caregivers who spend more time caregiving compared to their White counterparts, potentially exacerbating health care disparities in these communities (658)Fenton A, et al. (2022) Support Care Cancer, 30: 9625. [LINK NOT AVAILABLE].
While patients with cancer are susceptible to adverse mental health events, their caregivers may also experience higher levels of mental illness compared to the general population (662)Hu K, et al. (2023) JAMA Netw Open, 6: e2249560. [LINK NOT AVAILABLE]. It is vital that evidence-based resources be made available to help improve services and ensure optimal health for cancer caregivers.
The use of smartphone apps specifically for caregivers to help manage their loved ones’ care is being tested and utilized by hospital systems. For instance, apps that allow a caregiver to report symptoms and subsequently provide resources for self and patient care can help reduce burden and relieve anxiety experienced by the caregiver (659)Oakley-Girvan I, et al. (2023) PLOS Digit Health, 2: e0000173. [LINK NOT AVAILABLE](660)Ozluk P, et al. (2022) J Med Internet Res, 24: e28504. [LINK NOT AVAILABLE]. While these apps have been utilized for many other chronic conditions, their increasing use and effectiveness among caregivers of cancer patients and survivors will need to be continually evaluated (661)Guessi Margarido M, et al. (2022) NPJ Digit Med, 5: 33. [LINK NOT AVAILABLE].
Next Section: Envisioning the Future of Cancer Science and Medicine Previous Section: Immunotherapy— Pushing the Frontier of Cancer Medicine