Supporting Cancer Patients and Survivors
In this section, you will learn:
- As of January 2022, there are more than 18 million cancer survivors in the United States with 67 percent age 65 or older. The number of survivors is expected to grow to 26 million by 2040 with 74 percent expected to be 65 or older.
- Survivors of cancer face unique challenges associated with their diagnosis. These challenges can continue after completion of treatment and include side effects from medications, financial toxicity, reduced health-related quality of life, increased risk of new primary cancers, and increased psychosocial challenges.
- Exercise, a healthy diet, and smoking cessation are all ways to improve the survivorship experience.
- Successful survivorship relies on the use of patient navigators to coordinate cancer care, support for family caregivers, and equitable access to telehealth.
According to NCI, a person is considered a cancer survivor from the time of cancer diagnosis through the balance of his or her life. Each person diagnosed with cancer has a unique experience ranging from successful treatment and living cancer free for the remainder of life; to experiencing varying degrees of side effects; and/or experiencing a subsequent cancer diagnosis with the same or a different type of cancer.
Advances in treatments through dedicated efforts of researchers across the health care spectrum have led to more survivors living longer and fuller lives after a cancer diagnosis. As of 2022, more than five percent of the U.S. population is living with a history of a cancer diagnosis, equating to more than 18 million people (2)Miller KD, et al. Cancer Treatment and Survivorship Statistics, 2022. CA Cancer J Clin 2022;0:1-28. [LINK NOT AVAILABLE]; three out of four U.S. families have at least one member who has experienced a cancer diagnosis (395)Oh H, et al. The risk of psychological stress on cancer recurrence: A systematic review. Cancers (Basel) 2021;13:5816. [LINK NOT AVAILABLE]. This is in stark contrast to 50 years ago, when cancer survivors constituted only 1.4 percent of the U.S. population. By 2040, there are expected to be 26 million survivors in the U.S. population (2)Miller KD, et al. Cancer Treatment and Survivorship Statistics, 2022. CA Cancer J Clin 2022;0:1-28. [LINK NOT AVAILABLE], necessitating increased understanding of their challenges, how to improve the quality of their lives, and how to make sure their care is accessible and equitable.
In recent years, there has been a growing appreciation of the impact of a cancer diagnosis on friends, family, and caregivers, necessitating increased focus on the need to support patients along with their support structure to improve the survivorship experience.
The following section highlights the challenges faced by cancer survivors and their caregivers with a special emphasis on adolescents and young adults (AYAs), older adults, and the medically underserved. Later sections identify progress that has been made in improving the survivorship experience.
Challenges Faced by Cancer Survivors
Cancer survivors often face physical, psychosocial, and financial challenges that are attributable to the cancer itself and the treatments. Furthermore, a survivor’s support network including friends, family, and caregivers also experiences challenges related to caring for the survivor. Although research is ongoing, a greater understanding of these challenges and the ways to address them is required to support this vulnerable population.
Physical Challenges
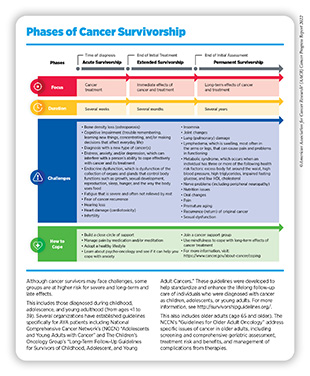
Short- and long-term symptoms experienced by cancer survivors can be debilitating. These include hair loss, pain, swelling of arms and legs (lymphedema), joint pain (arthralgia), insomnia, nausea, vomiting, and loss of smell and appetite. Long-term effects of cancer and cancer treatment include heart damage (cardiotoxicity), lung (pulmonary) damage, loss of bone density (osteoporosis), excess body fat, nerve issues (peripheral neuropathy), cognitive decline, infertility, and sexual dysfunction as well as development of secondary cancers (see sidebar on Phases of Cancer Survivorship).
One important area of ongoing research is to determine how certain cancer therapies lead to premature aging (396)Hurria A, et al. Cancer Treatment as an Accelerated Aging Process: Assessment, Biomarkers, and Interventions. Am Soc Clin Oncol Educ Book 2016;35:e516-22. [LINK NOT AVAILABLE]. Research has shown that cancer survivors have an “excess heart age”—a measure of cardiovascular damage and risk for a heart attack—of eight and a half years in men and six and half years in women compared to those individuals who have never received a cancer diagnosis (397)Scott LC, et al. Predicted Heart Age Among Cancer Survivors – United States, 2013-2017. MMWR Morb Mortal Wkly Rep 2021;70:1-6. [LINK NOT AVAILABLE]. Notably, average excess heart age was shown to be higher in cancer patients who are NHB, less educated, and have lower income.
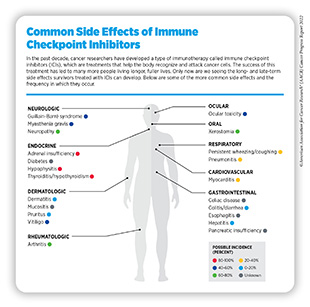
The increased use of precision medicine approaches including molecularly targeted therapeutics and immunotherapeutics has led to immense progress in treating cancer. Immune checkpoint inhibitors (ICIs) are a type of immunotherapy that is being used increasingly for the treatment of a wide array of cancers. Currently, there are nine ICIs approved by FDA to treat 18 different types of cancer, with some patients achieving highly durable responses. However, their widespread use has also led to concerns about the unique side effects that can result from these treatments. Because these inhibitors attempt to re-establish control of cells of the immune system, frequently observed side effects are autoimmune disorders, such as dermatitis, arthritis, and/or celiac disease (see sidebar on Common Side Effects of Immune Checkpoint Inhibitors). Furthermore, certain side effects including endocrinopathies (such as hypothyroidism), arthritis, dry mouth, neurotoxicity, and ocular-related effects are more likely to become long-term side effects (398)Johnson DB, et al. Immune-checkpoint inhibitors: long-term implications of toxicity. Nat Rev Clin Oncol 2022;19:254-67. [LINK NOT AVAILABLE]. With the increased use of these drugs resulting in long-term survival, an understanding of their long-term and late effects is necessary.
Psychosocial Challenges
Being faced with a diagnosis of cancer can pose a serious challenge to a person’s mental and emotional health. Cancer survivors can experience anxiety (7-21 percent), depression (5-7 percent), and distress (25-41 percent) with higher prevalence among those who are AYA, or belong to racial and ethnic minority and sexual and gender minority populations (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2022.[cited 2020 Jul 15].(399)Rincones O, et al. An updated systematic review of quantitative studies assessing anxiety, depression, fear of cancer recurrence or psychological distress in testicular cancer survivors. Cancer Manag Res 2021;13:3803-16. [LINK NOT AVAILABLE]. It is also concerning that the stress associated with a cancer diagnosis may lead to biological changes that increase cancer progression and recurrence (395)Oh H, et al. The risk of psychological stress on cancer recurrence: A systematic review. Cancers (Basel) 2021;13:5816. [LINK NOT AVAILABLE](400)Perego M, et al. Reactivation of dormant tumor cells by modified lipids derived from stress-activated neutrophils. Sci Transl Med 2020;12:eabb5817. [LINK NOT AVAILABLE](401)Manigault AW, et al. Vulnerability to inflammation-related depressive symptoms: Moderation by stress in women with breast cancer. Brain Behav Immun 2021;94:71-8. [LINK NOT AVAILABLE].
Even after successful cancer treatment, anxiety of cancer returning, or the development of new cancers, can lead to distress and/or depression. For instance, in one study that looked at long-term cancer survivors, survivors had higher levels of depression and anxiety after five or more years compared to just after their initial diagnosis (402)Breidenbach C, et al. Prevalence and determinants of anxiety and depression in long-term breast cancer survivors. BMC Psychiatry 2022;22:101. [LINK NOT AVAILABLE]. Meta-analysis of nurse-led interventions for anxiety management of cancer survivors demonstrate that one-on-one (versus group) approaches over an average of six months for no more than 60 minutes at a time are among the most effective way to help survivors deal with anxiety (403)Huynh NTT, et al. Nurse-led educational interventions for anxiety management in cancer survivors: a systematic review and meta-analysis. Support Care Cancer 2022;30:6699-744. [LINK NOT AVAILABLE].
A major concern among health care providers is the high risk of suicide in individuals who receive a cancer diagnosis (404)Heinrich M, et al. Suicide risk and mortality among patients with cancer. Nat Med 2022;28:852-9. [LINK NOT AVAILABLE]. Those who receive a poor cancer prognosis (i.e., low 5-year survival) have the greatest risk of self-harm. The risk of mortality from self-harm was highest within 12 months of diagnosis (405)Chang WH, et al. Cumulative burden of psychiatric disorders and self-harm across 26 adult cancers. Nat Med 2022;28:860-70. [LINK NOT AVAILABLE]. Proven intervention strategies include the use of psychotherapy (see Improving Mental Health); both nursing and caregiver interventions; and mindful activities including exercise, yoga, and music therapy (406)Bulotiene G, et al. Interventions for reducing suicide risk in cancer patients: A literature review. Eur J Psychol 2019;15:637-49. [LINK NOT AVAILABLE].
Survivors of cancer who are living longer with advanced and metastatic disease are particularly vulnerable to negative psychological challenges. Uncertainty about their prognosis can contribute to apprehension, anxiety, and distress especially during routine follow-up scans; this well-documented phenomenon has led to the term “scanxiety” (407)Mollica MA, et al. Survivorship for individuals living with advanced and metastatic cancers: National Cancer Institute Meeting Report. J Natl Cancer Inst 2022;114:489-95. [LINK NOT AVAILABLE]. Currently, there are several NCI-supported studies that are looking at survivorship in individuals living with advanced and metastatic cancers, which will help to identify the best way to support this population (408)Mollica MA, et al. Current state of funded National Institutes of Health grants focused on individuals living with advanced and metastatic cancers: a portfolio analysis. J Cancer Surviv 2021;15:370-4. [LINK NOT AVAILABLE].
It should be noted that caregivers of cancer survivors often experience burnout due to providing medical and social support for long periods of time. Increasing patient- and caregiver-centric support through psychosocial services, use of accurate prognostic tools, and further research to improve the unique experiences of survivors and their caregivers can help to overcome the challenges faced by these populations.
Financial Challenges
Financial toxicity refers to the financial hardship associated with cancer treatment and management. Accruing evidence indicates that cancer survivors who experience financial toxicity such as difficulty paying for prescriptions, mental health care, and dental care, and/or who delay medical care due to cost, are also at greater risk of mortality, regardless of insurance status (409)Yabroff KR, et al. Association of medical financial hardship and mortality among cancer survivors in the United States. J Natl Cancer Inst 2022;114:863-70. [LINK NOT AVAILABLE].
Financial toxicity is pervasive among patients with cancer. As one example, a recent study that looked at patients with colorectal cancer found that 71 percent experienced a major financial hardship at 12 months after diagnosis (410)Shankaran V, et al. S1417CD: A prospective multicenter cooperative group-led study of financial hardship in metastatic colorectal cancer patients. J Natl Cancer Inst 2022;114:372-80. [LINK NOT AVAILABLE]. Financial toxicity poses challenges not only to the mental and emotional health of those diagnosed with cancer, but also to immediate family members who may depend on the patient for their livelihood.
As of 2019, cancer is the second most expensive chronic health condition in the United States, with patients’ out-of-pocket costs and lost work hours totaling $21 billion a year (38)Yabroff KR, et al. Annual Report to the Nation on the Status of Cancer, part 2: Patient economic burden associated with cancer care. J Natl Cancer Inst 2021;113:1670-82. [LINK NOT AVAILABLE]. While much of the out-of-pocket costs associated with medical treatment can be covered by health insurance, patients who are enrolled in high-deductible insurance plans face increased expenses compared to those with either traditional plans or with no history of cancer.
One study that compared out-of-pocket costs of individuals on a high-deductible health plan found that those with a history of breast, colorectal, or lung cancer paid an additional $1,683, $1,450, and $467 respectively, compared to those with no history of cancer (411)Fu SJ, et al. Out-of-pocket costs among patients with a new cancer diagnosis enrolled in high-deductible health plans vs traditional insurance. JAMA Netw Open 2021;4:e2134282. [LINK NOT AVAILABLE]. This is especially concerning because of the estimates that 50 percent of all U.S. adults would have difficulty paying a $400 emergency expense, with 19 percent not being able to pay it at all (412)Federal Reserve Board. Survey of household economics and decisionmaking. Accessed: June 30, 2022.[cited 2020 Jul 15].. Patients with other types of cancer are also more likely to miss credit-card payments and to experience other adverse financial events because of missed debt payments (413)Shankaran V, et al. Risk of adverse financial events in patients with cancer: Evidence from a novel linkage between cancer registry and credit records. J Clin Oncol 2022;40:884-91. [LINK NOT AVAILABLE].
The inability to afford treatments often leads to coping behaviors such as skipping drug doses or not filling prescriptions; increased anxiety, stress, and depression; and forgoing spending on essentials such as food and clothing (414)Hussaini SMQ, et al. Financial toxicity of cancer treatment. JAMA Oncol 2022;8:788. [LINK NOT AVAILABLE]. However, one study looking at lung cancer patients after six months of receiving treatment found that while 28 percent had to make financial sacrifices, only five percent refused medical care based on cost (415)Friedes C, et al. Longitudinal trends of financial toxicity in patients with lung cancer: A prospective cohort study. JCO Oncol Pract 2021;17:e1094-e109. [LINK NOT AVAILABLE]. While this number is low, cost of treatment should never be a factor that prevents someone from receiving lifesaving care. Solutions to help those who are unable to afford treatment need to be explored to bring equitable access for all.
Those experiencing financial toxicity are also less likely to enroll in clinical trials, reducing access to potentially lifesaving treatments (416)Winkfield KM, et al. Addressing financial barriers to patient participation in clinical trials: ASCO policy statement. J Clin Oncol 2018:JCO1801132. [LINK NOT AVAILABLE](417)Unger JM, et al. The role of clinical trial participation in cancer research: Barriers, evidence, and strategies. Am Soc Clin Oncol Educ Book 2016;35:185-98. [LINK NOT AVAILABLE](418)Unger JM, et al. Patient income level and cancer clinical trial participation: A prospective survey study. JAMA Oncol 2016;2:137-9. [LINK NOT AVAILABLE]. To reduce the financial impact and help those cancer patients who have low household incomes, direct reimbursement of costs associated with clinical trials was found to significantly improve patient well-being, decrease vulnerability, and help protect right to equal treatment (419)Bex A, et al. A phase III, randomized, placebo-controlled trial of nivolumab or nivolumab plus ipilimumab in patients with localized renal cell carcinoma at high-risk of relapse after radical or partial nephrectomy (CheckMate 914). Journal of Clinical Oncology 2020;38:TPS5099-TPS. [LINK NOT AVAILABLE].
Recently, time toxicity, which is the amount of time a patient must devote to treatment, has been highlighted as an increasing challenge faced by survivors. This includes things like traveling to and from a treatment center, clinical and physical assessments, tumor assessments, infusions, and patient-reported assessments. In a study of nine clinical trials, researchers found that patients on active treatment spent a median of 16 hours distributed over 4-5 days on trial-related activities every month (420)Prasad V, et al. Estimation of time cost of anti-cancer drugs approved based on comparisons to best supportive care: a cross sectional analysis. medRxiv 2022:2022.06.22.22276763. [LINK NOT AVAILABLE].
Unique Challenges Faced by Vulnerable Populations
Adolescents and Young Adults
Adolescent and young adult (AYA) cancer survivors include those diagnosed between the ages of 15 and 39 and can face unique personal, social, and emotional challenges. Eighty-five and a half percent of AYA survivors are alive at least five years after diagnosis in 2018, compared to only 68 percent of adolescent survivors 40 years ago (421)National Cancer Institute. Cancer in children and adolescents. Accessed: April 22, 2022.[cited 2020 Jul 15]..
AYA populations are more vulnerable to certain side effects including stroke, neurodegenerative disorders, cardiovascular disease, diabetes, and other pulmonary diseases compared to their peers who have not had a cancer diagnosis (422)Gibson TM, et al. Temporal patterns in the risk of chronic health conditions in survivors of childhood cancer diagnosed 1970-99: a report from the Childhood Cancer Survivor Study cohort. Lancet Oncol 2018;19:1590-601. [LINK NOT AVAILABLE](423)Hudson MM, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 2013;309:2371-81. [LINK NOT AVAILABLE](424)Bhakta N, et al. Cumulative burden of cardiovascular morbidity in paediatric, adolescent, and young adult survivors of Hodgkin’s lymphoma: an analysis from the St Jude Lifetime Cohort Study. Lancet Oncol 2016;17:1325-34. [LINK NOT AVAILABLE]. Compared to the general population, AYA cancer survivors are nearly twice as likely to die from a subsequent primary cancer, stressing the importance of increased surveillance in this population (18)Sung H, et al. Subsequent primary cancer risk among five-year survivors of adolescent and young adult cancers. J Natl Cancer Inst 2022. [LINK NOT AVAILABLE].
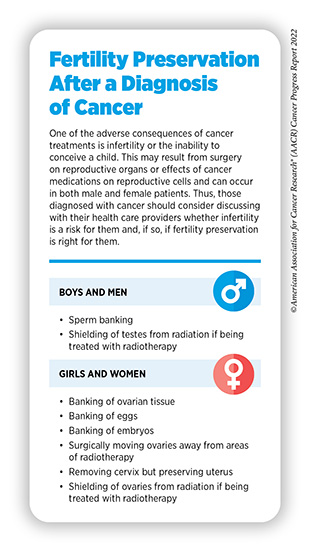
Many treatments for cancer, including surgery, radiotherapy, and cytotoxic chemotherapy, can cause male and female infertility, which is the inability to conceive a child. Loss of fertility is a significant concern among AYA cancer survivors and their caregivers, and can affect their psychological well-being, choice of treatments, and treatment adherence. According to a meta-analysis, between 44 and 86 percent of AYA survivors had moderate concerns about how cancer treatment would affect their fertility, while 28 to 44 percent had severe concerns (425)Xie J, et al. Reproductive concerns among adolescent and young adult cancer survivors: A scoping review of current research situations. Cancer Med 2022. [LINK NOT AVAILABLE].
The possibility of impaired reproductive abilities may lead some patients to store reproductive material through the process of fertility preservation (see sidebar on Fertility Preservation After a Diagnosis of Cancer). Rates of fertility preservation vary based on a patient’s age, sex, type of cancer, and treating institution. Participation in fertility preservation and what type of preservation should be sought are to be decided by the individual after discussions with the health care providers.
Unfortunately, fertility preservation rates are lower in survivors who are Black, poor, or live in rural areas. Currently, cancer-focused organizations have guidelines that recommend discussions of fertility preservation and sexual health as an essential part of cancer management, especially in AYA patient populations. Furthermore, as of June 2022, 12 states have mandates, and three have active legislation, requiring insurance coverage of fertility preservation for patients facing infertility due to treatments such as anticancer therapies (426)Alliance for Fertility Preservation. State laws & legislation. Accessed: July 14, 2022.[cited 2020 Jul 15]..
The Supreme Court’s decision on the Dobbs v. Jackson Women’s Health Organization case in June 2022 has led to serious concerns about how states may regulate embryonic material, which may affect access to fertility preservation services such as sperm and egg banking, banking of embryos, and in vitro fertilization by patients with cancer. For patients who may wish to become pregnant, conversations about fertility preservation and family planning are an essential early step to treatment and require careful, unrestricted conversations between patient and health care providers.
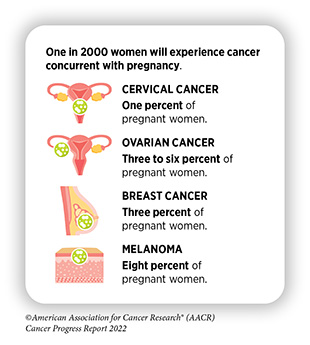
A recent population-based study of more than 42,000 women ages 16 to 49 indicates that about one in 2,000 pregnancies is complicated by cancer (427)Stensheim H, et al. Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: a registry-based cohort study. J Clin Oncol 2009;27:45-51. [LINK NOT AVAILABLE]. It has been well documented that some cancer treatments, such as chemotherapy, radiation therapy, and targeted therapies have varying risks to both mother and the developing embryo or fetus, with some preclinical and clinical evidence indicating high risk of fetal malformation or spontaneous abortion depending on the stage of pregnancy, type of therapy, and type of cancer (see sidebar Pregnancy and Cancer).
With the recent Supreme Court decision to overturn Roe v. Wade, which ends the constitutional right to an abortion, there is uncertainty surrounding how a particular cancer treatment may lead to the termination of a pregnancy. Such uncertainty may prohibit some physicians from prescribing a drug or performing other health services in a timely manner due to the potential legal consequences for both physician and mother. AACR as well as many other cancer advocacy organizations is extremely concerned about the ramifications of the Dobbs v. Jackson Women’s Health Organization decision and the effect it could have on access to equitable quality health care. A reluctance or delay in starting treatment could lead to cancer progressing to an advanced stage, thus making the cancer more difficult to treat. Understanding the effects of limited options for health care interventions for pregnant women with cancer needs to be prioritized to provide the best care for this population.
Apart from physical side effects, the disruptive nature of a cancer diagnosis also impacts social development, psychological health, and career development. Together, these result in poorer health-related quality of life (HRQOL) and a greater psychological distress among AYA cancer survivors compared to those who have never received a cancer diagnosis (446)Dixon SB, et al. Racial and ethnic disparities in neurocognitive, emotional, and quality-of-life outcomes in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer 2019;125:3666-77. [LINK NOT AVAILABLE](447)Abdelhadi OA, et al. Psychological distress and associated additional medical expenditures in adolescent and young adult cancer survivors. Cancer 2022;128:1523-31. [LINK NOT AVAILABLE].
Also contributing to poorer HRQOL is financial toxicity, with AYA cancer survivors at a greater risk of experiencing financial toxicity compared to older survivors (448)Ghazal LV, et al. Financial toxicity in adolescents and young adults with cancer: A concept analysis. Cancer Nurs 2021;44:E636-E51. [LINK NOT AVAILABLE](449)Meernik C, et al. Material and psychological financial hardship related to employment disruption among female adolescent and young adult cancer survivors. Cancer 2020;127:137-48. [LINK NOT AVAILABLE]. AYA survivors who live at or below the federal poverty threshold have decreased survival compared to those above (450)Murphy CC, et al. Disparities in cancer survival among adolescents and young adults: A population-based study of 88 000 patients. J Natl Cancer Inst 2021;113:1074-83. [LINK NOT AVAILABLE]. AYA survivors who are diagnosed with a psychological disorder are more likely to have increased medical expenses compared to their peers who did not experience a psychological episode (447)Abdelhadi OA, et al. Psychological distress and associated additional medical expenditures in adolescent and young adult cancer survivors. Cancer 2022;128:1523-31. [LINK NOT AVAILABLE].
After conclusion of treatment, AYA patients often have trouble with follow-up care, which can impact future screening for recurrent or new cancers and management of side effects. For some, getting transportation to follow-up care can be difficult. Promisingly, new evidence reveals that the implementation of telehealth strategies that were necessitated by the COVID-19 pandemic has helped mitigate transportation challenges and improve follow-up care specifically among AYA cancer survivors (451)Linendoll N, et al. Adolescent and young adult survivorship care: Emerging from the COVID-19 pandemic stronger through teleoncology. J Adolesc Young Adult Oncol 2022;0:null. [LINK NOT AVAILABLE].
Current guidelines during end-of-life care favor focusing on HRQOL over intense treatment interventions, which can be aggressive, invasive, and expensive. Unfortunately, one study that looked specifically at treatment intensity found that AYA cancer patients received increased frequency of intense interventions, such as the use of mechanical ventilation or admittance to intensive care units (452)Coltin H, et al. Locus-of-care disparities in end-of-life care intensity among adolescents and young adults with cancer: A population-based study using the IMPACT cohort. Cancer 2022;128:326-34. [LINK NOT AVAILABLE].
Older Adults
Older adults are defined as those age 65 and over and represent 64 percent of cancer survivors in the United States. This population is also the fastest growing and is projected to increase to 73 percent of cancer survivors by 2040 (453)Mohile SG, et al. Improving the quality of survivorship for older adults with cancer. Cancer 2016;122:2459-568. [LINK NOT AVAILABLE]. However, studies of this population of cancer survivors are rare (454)Outlaw D, et al. Is the lack of evidence in older adults with cancer compromising safety? Expert Opin Drug Saf 2020;19:1059-61. [LINK NOT AVAILABLE]. More attention and resources are needed to understand the unique challenges faced by older adults.
Cancer and its treatments can lead to side effects that are experienced differently in older adults when compared to those younger than age 65 (455)Siddique A, et al. Functional decline among older cancer survivors in the Baltimore longitudinal study of aging. J Am Geriatr Soc 2021;69:3124-33. [LINK NOT AVAILABLE]. Evidence shows that 25 percent of older adults with cancer have five or more comorbid conditions (e.g., arthritis, diabetes, or mental health) (456)Fitch MI, et al. Main challenges in survivorship transitions: Perspectives of older adults with cancer. J Geriatr Oncol 2021;12:632-40. [LINK NOT AVAILABLE]. Older adults may also be prescribed multiple medications to treat other conditions with 22.4 percent of U.S. adults using at least five prescription drugs at a time (457)Centers for Disease Control and Prevention. Prescription drug use among adults aged 40–79 in the United States and Canada. Accessed: July 28, 2022.[cited 2020 Jul 15]., which leads to safety concerns of adverse drug effects, harmful drug interactions, and drug-disease interactions, in which a medication prescribed to treat one condition worsens another or causes a new one.
Cognitive decline is greater in older adults following treatment, with this group more likely to see declines in executive function and verbal memory. In a recent study, it was found that despite showing high levels of cognitive function at diagnosis, older adults were more likely to experience cognitive decline post-treatment than those younger than age 65 (459)Fitch MI, et al. Challenges of survivorship for older adults diagnosed with cancer. Curr Oncol Rep 2022;24:763-73. [LINK NOT AVAILABLE].
Older adult survivors also experience poorer HRQOL compared to those under the age of 65 with variations depending on the type of cancer, side effects, frailty, fatigue, and health status. Psychosocial variables such as depression, reduced optimism, chronic stress, and lack of emotional support also influence HRQOL in older adult cancer survivors compared to adult survivors. HRQOL is also worse in groups who are of low socioeconomic status (459)Fitch MI, et al. Challenges of survivorship for older adults diagnosed with cancer. Curr Oncol Rep 2022;24:763-73. [LINK NOT AVAILABLE]
There is emerging evidence that a comprehensive geriatric assessment of patients at the time of diagnosis can help in planning appropriate interventions by evaluating their functional ability, physical health, cognition and mental health, and socio-environmental circumstances (460)Nishijima TF, et al. A 10-item frailty index based on a comprehensive geriatric assessment (FI-CGA-10) in older adults with cancer: Development and construct validation. Oncologist 2021;26:e1751-e60. [LINK NOT AVAILABLE]. Comprehensive geriatric assessments are not widely utilized because they are often taxing and time-consuming for both patients and providers (458)Fitch MI, et al. Measuring quality of life in older people with cancer. Curr Opin Support Palliat Care 2021;15:39-47. [LINK NOT AVAILABLE]. Therefore, increased support through support staff and a multidisciplinary team are essential for successful implementation of comprehensive geriatric assessments (461)Overcash J, et al. Comprehensive geriatric assessment as a versatile tool to enhance the care of the older person diagnosed with cancer. Geriatrics 2019;4:39. [LINK NOT AVAILABLE].
Racial and Ethnic Minorities and Other Underserved Populations
Individuals from racial and ethnic minority groups and other underserved populations have been found to experience side effects at higher rates than those who are White. The adverse physical effects, coupled with worsened functional, psychological, social, and financial challenges, contribute to poorer HRQOL. As one example, the development of breast cancer-related lymphedema, which occurs after damage to the lymphatic system during surgery, occurs 3.85 times more often in Black women and 1.47 times more often in Hispanic women (462)Kwan ML, et al. Race/ethnicity, genetic ancestry, and breast cancer-related lymphedema in the Pathways Study. Breast Cancer Res Treat 2016;159:119-29. [LINK NOT AVAILABLE]. Lymphedemas are often painful and require the use of special equipment to manage symptoms. These types of challenges lead to lower overall HRQOL in cancer survivors compared to individuals who have never had a cancer diagnosis, especially in medically underserved groups.
Financial toxicity is more prevalent in individuals from disadvantaged groups such as those of low socioeconomic status, further exacerbating their economic hardship. As one example, Black and Hispanic patients with cancer experience adverse financial events twice as often as White patients, leading to increased use of financial coping behaviors, such as skipping medications (463)Jagsi R, et al. Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol 2014;32:1269-76. [LINK NOT AVAILABLE].
Consequences of financial toxicity including food insecurity, which is a lack of access to enough food for an active and healthy life, and unequal access to safe and adequate housing and are prevalent in low-income, racial and ethnic minority, and immigrant survivors of cancer.
Understanding the challenges faced by these groups will help inform cancer care strategies and personalized recommendations to support those who are more vulnerable, and may lead to better HRQOL. The release of the AACR Cancer Disparities Progress Report 2022 summarizes the inequities in survivorship experiences among these population groups and outlines concrete steps to charting a path forward (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2022.[cited 2020 Jul 15]..
Improving Health-related Quality of Life and Outcomes
Promoting Healthy Behaviors
Certain lifestyle changes can significantly improve both cancer outcomes and HRQOL for cancer survivors. These include eliminating tobacco use, adopting a healthy diet, increasing physical activity, and reducing alcohol consumption.
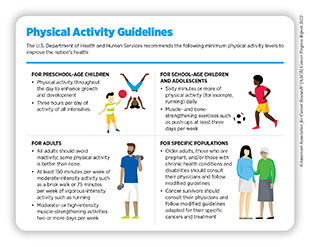
Cancer survivors who incorporate routine exercise into their life (see sidebar on Physical Activity Guidelines) can significantly improve survival from several types of cancer including breast, colon, and prostate (464)Printz C. An expanded role for exercise in cancer treatment and survivorship: Backed by a trove of studies regarding the benefits of physical activity for patients with cancer and cancer survivors, researchers have updated exercise guidelines for these groups. Cancer 2020;126:2731-2. [LINK NOT AVAILABLE](465)Langlais CS, et al. Post-diagnostic dietary and lifestyle factors and prostate cancer recurrence, progression, and mortality. Curr Oncol Rep 2021;23:37. [LINK NOT AVAILABLE], while a sedentary lifestyle is associated with an elevated risk of cancer-related mortality (466)Cao C, et al. Association of daily sitting time and leisure-time physical activity with survival among US cancer survivors. JAMA Oncol 2022;8:395-403. [LINK NOT AVAILABLE]. Studies also demonstrate that
incorporation of physical activity can reduce cancer recurrence by half compared to those who do not participate in exercise (467)Morishita S, et al. Effect of Exercise on Mortality and Recurrence in Patients With Cancer: A Systematic Review and Meta-Analysis. Integr Cancer Ther 2020;19:1534735420917462. [LINK NOT AVAILABLE](468)Cannioto RA, et al. Physical Activity Before, During, and After Chemotherapy for High-Risk Breast Cancer: Relationships With Survival. J Natl Cancer Inst 2021;113:54-63. [LINK NOT AVAILABLE].
Physical activity may also alleviate certain adverse side effects experienced by cancer survivors. For instance, one study from the United Kingdom found that breast cancer survivors who participated in regimented physiotherapy over three months had reduced upper limb disability after one year compared to those who did not receive structured exercise therapy (469)Bruce J, et al. Exercise versus usual care after non-reconstructive breast cancer surgery (UK PROSPER): multicentre randomised controlled trial and economic evaluation. BMJ 2021;375:e066542. [LINK NOT AVAILABLE]. Studies also demonstrate that exercise can improve bone and spine health in patients with cancer (470)Rose GL, et al. The effects of exercise on the bone health of people with cancer: a systematic review and meta-analysis. Osteoporosis International 2022;33:327-38. [LINK NOT AVAILABLE](471)American College of Sports Medicine. Does physical activity mitigate the risk of frailty-related bone fractures among cancer survivors? Accessed: June 30, 2022.[cited 2020 Jul 15].. Furthermore, moderate exercise can reduce cardiovascular risk factors by up to 33 percent, as reported in a study of long-term breast cancer survivors (472)Naaktgeboren WR, et al. Physical activity and cardiac function in long-term breast cancer survivors: A cross-sectional study. JACC CardioOncol 2022;4:183-91. [LINK NOT AVAILABLE]. This is especially relevant because cardiovascular disease is the primary cause of non-cancer-related deaths in breast cancer survivors, accounting for mortality in 35 percent of breast cancer survivors age 50 or older (473)Coughlin SS, et al. Cardiovascular disease among breast cancer survivors. Cardiovasc Disord Med 2020;2. [LINK NOT AVAILABLE].
Initiatives such as the Get Up, Get Moving program from the Oncology Nursing Society, which provided at-home, personalized physical activity coaching and electronic activity trackers to cancer patients, can promote increases in physical activity and help reduce common side effects such as nausea from cancer treatments (474)Forner JK, et al. Quality of life: A nurse-led physical activity coaching program to improve the quality of life of patients with cancer during the COVID-19 pandemic. Clin J Oncol Nurs 2021;25:571-7. [LINK NOT AVAILABLE].
Preliminary studies in animal models show that exercise during active treatment with cancer immunotherapy can reduce disease progression and mortality (475)Kurz E, et al. Exercise-induced engagement of the IL-15/IL-15Ralpha axis promotes anti-tumor immunity in pancreatic cancer. Cancer Cell 2022;40:720-37 e5. [LINK NOT AVAILABLE]. In the Preoperative Rehabilitation During Neoadjuvant Therapy for Pancreatic Cancer clinical trial, pancreatic cancer patients who exercised prior to surgery had more immune cells which were associated with tumor elimination. The trial, which began in 2017, has also shown that there is a 50 percent higher five-year survival rate for those who exercise compared to those who do not (476)Drugs.Com. Exercise amplifies immune attack on pancreatic cancer. Accessed: July 6, 2022.[cited 2020 Jul 15].(477)ClinicalTrials.Gov. Preoperative rehabilitation during neoadjuvant therapy for pancreatic cancer. Accessed: July 14, 2022.[cited 2020 Jul 15]..
Sustaining a healthy diet that consists of whole grains, fruits, and vegetables can increase survival from cancer and reduce the risk of cancer recurrence (478)Rock CL, et al. American Cancer Society nutrition and physical activity guideline for cancer survivors. CA: A Cancer Journal for Clinicians 2022;72:230-62. [LINK NOT AVAILABLE]. Multiple population-based studies with evidence collected over the past 20 years from survivors of prostate cancer show that in addition to smoking and diets with high saturated fats, consumption of greater than four servings per week of whole milk and/or high-fat dairy products following a diagnosis of prostate cancer was associated with higher risk of prostate cancer recurrence and mortality (465)Langlais CS, et al. Post-diagnostic dietary and lifestyle factors and prostate cancer recurrence, progression, and mortality. Curr Oncol Rep 2021;23:37. [LINK NOT AVAILABLE].
Poor diet, which can contribute to other chronic health conditions such as diabetes, can negatively impact survival from cancer. In one study of long-term survivors of metastatic breast cancer, 10 years after diagnosis, those who had diabetes had 20 percent lower rate of survival compared to those who did not have diabetes. Furthermore, of those with diabetes, those with better management of blood sugar levels had 20 percent higher rates of survival compared to those who did not manage their blood sugar levels (479)The ASCO Post Staff. Study links diabetes and worse outcomes in long-term survivors of metastatic breast cancer. Accessed: July 14, 2022.[cited 2020 Jul 15]..
As discussed in earlier sections, maintaining a healthy diet can often be a challenge for cancer survivors, particularly those from low-income, immigrant, and other vulnerable populations, because of food insecurity. One clinical trial that provided food voucher programs in combination with access to a food pantry improved outcomes for food-insecure cancer patients with 95 percent completing their prescribed cancer treatment. This outcome was compared to those who only had access to a food delivery service and food pantry or to just the pantry alone, with an 83 percent or 78 percent treatment completion rate, respectively (480)Gany F, et al. Food to overcome outcomes disparities: A randomized controlled trial of food insecurity interventions to improve cancer outcomes. J Clin Oncol 2022:JCO2102400. [LINK NOT AVAILABLE]. It is imperative that survivorship interventions screen for food insecurity and provide cancer patients and survivors with necessary services which increase treatment completion and improve HRQOL.
Decades of evidence indicate that smoking cessation after a cancer diagnosis can improve clinical outcomes by increasing survival, reducing drug interactions, and improving quality of life after treatment. All major cancer-focused professional organizations recommend smoking cessation after a cancer diagnosis (481)Fox JL, et al. The effect of smoking status on survival following radiation therapy for non-small cell lung cancer. Lung Cancer 2004;44:287-93. [LINK NOT AVAILABLE](482)Gritz ER, et al. Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Cancer Epidemiol Biomarkers Prev 2005;14:2287-93. [LINK NOT AVAILABLE](483)Jensen K, et al. Smoking has a negative impact upon health related quality of life after treatment for head and neck cancer. Oral Oncol 2007;43:187-92. [LINK NOT AVAILABLE](484)Videtic GM, et al. Continued cigarette smoking by patients receiving concurrent chemoradiotherapy for limited-stage small-cell lung cancer is associated with decreased survival. J Clin Oncol 2003;21:1544-9. [LINK NOT AVAILABLE].
Although smoking cessation can be difficult for some patients, intensive programs that provide counseling and FDA-approved medication are both cost effective and highly effective in smoking cessation (486)Levy DE, et al. Cost-effectiveness of implementing smoking cessation interventions for patients with cancer. JAMA Netw Open 2022;5:e2216362. [LINK NOT AVAILABLE].
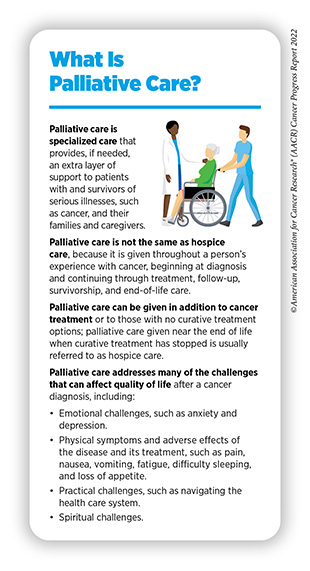
Integrating Palliative Care
Palliative care is an approach to prevent or treat the symptoms and side effects of any disease, including cancer, by addressing the physical, psychological, financial, social, and spiritual needs that arise from the disease and the treatments (see sidebar on What Is Palliative Care?). Palliative care is facilitated by a multidisciplinary team of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers and has been shown to improve quality of life for patients, families, and caregivers (487)Radbruch L, et al. Redefining palliative care-A new consensus-based definition. J Pain Symptom Manage 2020;60:754-64. [LINK NOT AVAILABLE].
Integration of palliative care during the early stage of a person’s cancer experience can significantly improve HRQOL. Multiple studies have reported that palliative care leads to improved management of symptoms resulting from cancer and/or its treatment, decreases depression and anxiety, reduces financial toxicity, improves HRQOL for both cancer survivors and their caregivers, and results in longer survival (488)Chung V, et al. Improving palliative care and quality of life in pancreatic cancer patients. J Palliat Med 2022;25:720-7. [LINK NOT AVAILABLE](489)Sedhom R, et al. How palliative care teams can mitigate financial toxicity in cancer care. Support Care Cancer 2021;29:6175-7. [LINK NOT AVAILABLE](490)Ferrell B, et al. A palliative care intervention for patients on phase 1 studies. J Palliat Med 2021;24:846-56. [LINK NOT AVAILABLE](491)Nelson AM, et al. Palliative care and coping in patients with acute myeloid leukemia: Mediation analysis of data from a randomized clinical trial. Cancer 2021;127:4702-10. [LINK NOT AVAILABLE].
In one clinical trial of patients with acute myeloid leukemia it was found that the use of a palliative care team early on in treatment with intensive chemotherapy led to increased practice of coping strategies among patients. These coping strategies led to a reduction in depression and anxiety symptoms and better HRQOL in this group compared to those who did not receive palliative care (491)Nelson AM, et al. Palliative care and coping in patients with acute myeloid leukemia: Mediation analysis of data from a randomized clinical trial. Cancer 2021;127:4702-10. [LINK NOT AVAILABLE].
Due to the increased risk of financial toxicity among cancer patients and survivors, interventions to alleviate this risk must be explored. Despite the prevalence of financial toxicity, oncologists are often not prepared to engage in these conversations necessitating increased training or alternative strategies (492)Henrikson NB, et al. Patient and oncologist discussions about cancer care costs. Support Care Cancer 2014;22:961-7. [LINK NOT AVAILABLE](493)Kelly RJ, et al. Patients and physicians can discuss costs of cancer treatment in the clinic. J Oncol Pract 2015;11:308-12. [LINK NOT AVAILABLE]. For instance, one study found that palliative care teams could help screen for financial hardship early on in care (494)Yabroff KR, et al. Improving the process of screening for medical financial hardship in oncology practice. Cancer Epidemiol Biomarkers Prev 2021;30:593-6. [LINK NOT AVAILABLE]. Interviews with patients have revealed that these discussions, held with trusted individuals who provide emotional support and understanding, can help alleviate anxiety about the financial challenges of cancer treatment and survivorship (495)Pisu M, et al. How, when, and with whom should cost of care conversations occur? Preferences of two distinct cancer survivor groups. JCO Oncol Pract 2020;16:e912-e21. [LINK NOT AVAILABLE].
Improving Mental Health
The psychological challenges faced by survivors of cancer necessitate approaches that improve the mental well-being of this population (see Challenges Faced by Cancer Survivors). One promising area is psycho-oncology, an interdisciplinary subspeciality within the cancer care continuum that aims to address the physical, behavioral, emotional, and psychosocial distress that arises for cancer survivors and their caregivers (496)Lang-Rollin I, et al. Psycho-oncology. Dialogues Clin Neurosci 2018;20:13-22. [LINK NOT AVAILABLE]. Experts who are trained in psycho-oncology apply a holistic approach to destigmatize and address behavioral and psychosocial distress that is often caused by cancer diagnosis and treatment (see sidebar on Helping Patients with Cancer Through Psycho-oncology Research).
Participating in face-to-face or online group positive psychotherapy, an approach that focuses on increasing resilience and a sense of well-being for cancer survivors, significantly reduced symptoms of emotional distress and improved mental well-being among cancer patients (499)Lleras de Frutos M, et al. Video conference vs face-to-face group psychotherapy for distressed cancer survivors: A randomized controlled trial. Psychooncology 2020;29:1995-2003. [LINK NOT AVAILABLE].
Researchers are also trying to understand how survivors of cancer experience post traumatic growth, which describes the positive life changes that can develop out of traumatic, stressful events such as a diagnosis of cancer. This type of growth includes perceptions of new possibilities, closer relationships with family and friends, development of personal strength, spiritual development, and a greater appreciation for life (500)Fu X, et al. Research progress on influencing factors and intervention measures of post-traumatic growth in breast cancer patients. Front Public Health 2022;10:927370. [LINK NOT AVAILABLE]. Although the concept of post-traumatic growth is not new, it is just beginning to be appreciated within the cancer community to understand how to foster these positive outlooks in survivors and improve mental health. The most influential factors that affect post-traumatic growth include the level of social support and the use of various coping strategies among survivors of cancer (see sidebar on Coping With Post-Traumatic Stress After a Cancer Diagnosis).
Delivering Care to Cancer Survivors
Coordinating Care
The multifaceted approach to treating cancer means providing survivors with care to address their many needs including transition from active treatment; coordinating follow-up appointments; addressing financial needs; and access to other survivorship resources. While these resources are often available, understanding how or where to gain access to them can be challenging (505)Fong AJ, et al. Survivorship transition care experiences and preparedness for survivorship among a diverse population of cancer survivors in New Jersey. Eur J Cancer Care (Engl) 2022;31:e13553. [LINK NOT AVAILABLE]; this necessitates the coordination of care for patients to help them identify and gain access to such resources.
Coordinated cancer care is most effective when a designated care coordinator, an individual or a team of people such as patient navigators, helps a patient with cancer or a survivor of cancer in getting access to the resources they need. A meta-analysis looking at 30 years of empirical evidence of coordinated cancer care, often through patient navigation,
showed there was an 81 percent improvement in outcomes for patients and reduced costs associated with care (506)Gorin SS, et al. Cancer care coordination: A systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med 2017;51:532-46. [LINK NOT AVAILABLE].
Clinical follow-up programs are an important first step to help coordinate care for survivors of cancer. These include active surveillance programs, standardization of protocols among stakeholders, and follow-up through telehealth methods. In an analysis of colorectal cancer patients, implementation of the previously mentioned strategies reduced readmissions at 30 days by 32 percent and significantly reduced the time spent in the hospital by one and a half days (507)Trindade LF, et al. Effectiveness of care transition strategies for colorectal cancer patients: a systematic review and meta-analysis. Support Care Cancer 2022;30:6251-61. [LINK NOT AVAILABLE].
Supporting Caregivers
Caregivers comprise family members or friends who help patients with long-term, chronic illness manage all aspects of their care. One in five U.S. adults (ages 18 to 64), which is over 43 million people, provided care for another person in 2020 (509)National Partnership for Women and Families. Paid leave could keep more than 6 million caregivers connected to the labor force by 2030. Accessed: June 30, 2022.[cited 2020 Jul 15].. It is estimated that four million of these caregivers are caring for an adult cancer patient. More evidence surrounding the challenges faced by this population is becoming clear and there are many opportunities to assist this vulnerable group.
Of the 43.5 million caregivers, only 60 percent had been employed in the previous 12 months (509)National Partnership for Women and Families. Paid leave could keep more than 6 million caregivers connected to the labor force by 2030. Accessed: June 30, 2022.[cited 2020 Jul 15].. Nearly half of employed caregivers reported challenges with maintaining normal job hours, with 24 percent reporting reduced work hours and 11 percent retiring early (510)Longacre ML, et al. Cancer caregiving while employed: Caregiving roles, employment adjustments, employer assistance, and preferences for support. J Cancer Educ 2021;36:920-32. [LINK NOT AVAILABLE].
Paid leave can allow caregivers to help family with long-term illnesses such as cancer. Unfortunately, 77 percent of U.S. workers do not have access to paid leave, forcing workers to take unpaid leave, which results in lost income that can be detrimental to a family’s financial health, potentially leading to financial toxicity (511)Bradley CJ. Economic burden associated with cancer caregiving. Semin Oncol Nurs 2019;35:333-6. [LINK NOT AVAILABLE]. Financial toxicity among caregivers leads to higher rates of nonadherence to cancer care, increased lifestyle-altering behaviors, and worse quality of life in both patients and caregivers (507)Trindade LF, et al. Effectiveness of care transition strategies for colorectal cancer patients: a systematic review and meta-analysis. Support Care Cancer 2022;30:6251-61. [LINK NOT AVAILABLE].
Evidence indicates that implementation of paid leave reduces household income volatility, facilitates reemployment, and leads to more workers reentering the labor force (513)Washington Center for Equitable Growth. Paid medical leave research – equitable growth. Accessed: June 30, 2022.[cited 2020 Jul 15].. Currently, there is no federal paid leave plan and only 12 U.S. states have or will implement programs by 2026 (514)AARP. What states offer paid family leave for caregivers? Accessed: June 30, 2022.[cited 2020 Jul 15].. By 2030, the number of caregivers is expected to increase by 9.3 million. To preserve the U.S. labor force and ensure optimal health for cancer patients and their caregivers, it is vital that better paid leave policies are implemented.
Implementing Telehealth
The COVID-19 pandemic led to a meteoric rise in the use of telehealth for all aspects of patient care (see sidebar on What Is Telemedicine?). The use of telemedicine by older adults and patients with cancer has already had a widespread positive effect on the delivery of oncology services during the pandemic and has allowed patients to continue receiving cancer care, even when they are unable to visit a health care facility in person (8)American Association for Cancer Research. AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care. Accessed: June 30, 2022.[cited 2020 Jul 15].. Current data indicate that there is overwhelming support by both cancer survivors and providers for the delivery of various types of survivorship care services with telehealth. These services include laboratory results or imaging, management and treatment of cancer symptoms, nutrition counseling, and patient navigation support (516)Arem H, et al. Cancer provider and survivor experiences with telehealth during the COVID-19 pandemic. JCO Oncol Pract 2022;18:e452-e61. [LINK NOT AVAILABLE]. Use of telehealth also led to increases in quality of life compared to usual care methods (517)Larson JL, et al. The effect of telehealth interventions on quality of life of cancer survivors: A systematic review and meta-analysis. Health Informatics J 2020;26:1060-78. [LINK NOT AVAILABLE].
Next Section: Looking to the Future of Cancer Science and Medicine Previous Section: Decoding Cancer Complexity. Integrating Science. Transforming Patient Outcomes.