Supporting Cancer Patients and Survivors
In this section, you will learn:
- In the United States, there are more than 16.9 million people living with a history of cancer.
- Each person diagnosed with cancer faces a unique set of challenges, but one in four survivors reports a poor physical quality of life and one in 10 reports poor mental health–related quality of life.
- Several strategies, including adopting health behaviors and palliative care can improve quality of life and cancer-related outcomes.
- It is vital that we identify the optimal way to provide comprehensive, coordinated care to all survivors of cancer and ensure that this care improves cancer-related outcomes and health-related quality of life for all patients.
Research is driving advances in cancer detection, diagnosis, and treatment that are helping more and more people to survive longer and lead fuller lives after a cancer diagnosis. According to the latest estimates, more than 16.9 million U.S. adults and children with a history of cancer were alive on January 1, 2019, compared with just 3 million in 1971 (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;(424).
While a person is considered a survivor from the time of cancer diagnosis through the remainder of life, not everyone identifies or agrees with this term. Each person who is diagnosed with cancer has a unique experience. These experiences range from successful treatment and living cancer free for the remainder of life, with or without adverse effects of treatment, to living with cancer and any effects of treatment for the remainder of life.
Cancer survivorship encompasses three distinct phases: the time from diagnosis to the end of initial treatment, the transition from treatment to extended survival, and long-term survival. Each phase of cancer survivorship is accompanied by a unique set of challenges (see sidebar on Life after a Cancer Diagnosis in the United States). Importantly, the issues facing each cancer survivor vary, depending on many factors, including gender, age at diagnosis, type of cancer diagnosed, general health at diagnosis, and type of treatment received.
One challenge facing patients and survivors with cancer that has emerged as increasingly important in recent years is financial hardship, or financial toxicity (425)(426)Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or Debt? National Estimates of Financial Toxicity in Persons with Newly-Diagnosed Cancer. Am J Med [Internet]. Elsevier Inc.; 2018;131:1187-1199.e5.(427)Financial Toxicity and Cancer Treatment (PDQ®)—Health Professional Version – National Cancer Institute [Internet]. [cited 2019 Jun 20].. Researchers studying financial hardship measure it in several ways: material financial hardship includes problems paying medical bills and depleting savings to pay medical bills; psychological financial hardship includes stress and worry about paying medical bills; and behavioral financial hardship includes delaying or forgoing cancer care because of cost. One recent study found that 25 percent of cancer survivors ages 18 to 64 reported material financial hardship and 34 percent reported psychological financial hardship (425). Another study showed that 42 percent of cancer survivors age 50 or older had depleted their entire life savings within two years of their cancer diagnosis (426)Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or Debt? National Estimates of Financial Toxicity in Persons with Newly-Diagnosed Cancer. Am J Med [Internet]. Elsevier Inc.; 2018;131:1187-1199.e5..
Certain U.S. population groups are more likely to report financial hardship, including racial/ethnic minorities, individuals who have lower educational attainment, individuals who have lower family income, and individuals who lack health insurance (428)Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. Medical Financial Hardship Intensity and Financial Sacrifice Associated with Cancer in the United States. Cancer Epidemiol Biomarkers Prev [Internet]. American Association for Cancer Research; 2020 [cited 2020 Jul 3];29:308–17.(429)Hastert TA, Kyko JM, Reed AR, Harper FWK, Beebe-Dimmer JL, Baird TE, et al. Financial Hardship and Quality of Life among African American and White Cancer Survivors: The Role of Limiting Care Due to Cost. Cancer Epidemiol Biomarkers Prev [Internet]. American Association for Cancer Research; 2019 [cited 2019 Dec 17];28:1202–11.(430). For example, in one study, cancer survivors who were African American were 23 percent more likely to report financial hardship than those who were white (429)Hastert TA, Kyko JM, Reed AR, Harper FWK, Beebe-Dimmer JL, Baird TE, et al. Financial Hardship and Quality of Life among African American and White Cancer Survivors: The Role of Limiting Care Due to Cost. Cancer Epidemiol Biomarkers Prev [Internet]. American Association for Cancer Research; 2019 [cited 2019 Dec 17];28:1202–11.. Adolescents and young adults, as well as long-term survivors of childhood cancer, are also more likely to report financial hardship, particularly financial hardship caused by the indirect costs of lost productivity, such as days lost from work or disability days (431)Ketterl TG, Syrjala KL, Casillas J, Jacobs LA, Palmer SC, McCabe MS, et al. Lasting effects of cancer and its treatment on employment and finances in adolescent and young adult cancer survivors. Cancer [Internet]. 2019 [cited 2019 Jun 20];125:1908–17.(432)IC H, N B, TM B, JL K, KR K, D S, et al. Determinants and Consequences of Financial Hardship Among Adult Survivors of Childhood Cancer: A Report From the St. Jude Lifetime Cohort Study. J Natl Cancer Inst [Internet]. J Natl Cancer Inst; 2019 [cited 2020 Jul 3];111..
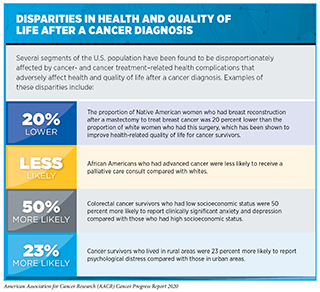
Unfortunately, financial hardship is not the only challenge posed by cancer and cancer treatment that disproportionately affects certain segments of the U.S. population. There are disparities in many of the health complications related to cancer and cancer treatment that adversely affect the health and quality of life of patients and survivors with cancer, as well as disparities in receipt of care to overcome these complications (see sidebar on Disparities in Health and Quality of Life after a Cancer Diagnosis).
Improving Quality of Life and Outcomes across the Continuum of Cancer Care
For patients and survivors with cancer, quality of life is a multidimensional concept that goes beyond the person’s cancer-related outcomes and considers their overall physical, mental, emotional, and social functioning (437)Barile JP, Reeve BB, Smith AW, Zack MM, Mitchell SA, Kobau R, et al. Monitoring population health for Healthy People 2020: evaluation of the NIH PROMIS® Global Health, CDC Healthy Days, and satisfaction with life instruments. Qual Life Res [Internet]. 2013 [cited 2019 Jun 20];22:1201–11.. As more and more people are surviving longer after a cancer diagnosis, the issue of quality of life has become increasingly important across the continuum of cancer care (438)Shapiro CL. Cancer Survivorship. Longo DL, editor. N Engl J Med [Internet]. 2018 [cited 2019 Jun 20];379:2438–50..
In recent years, some of the changes in cancer treatment are helping to reduce the short-term, long-term, and late effects of treatment. This is improving quality of life for patients and survivors, allowing many of them to continue to live their lives, as Congresswomen Lucy McBath was able to do when she was treated for breast cancer. For example, molecularly targeted therapeutics more precisely target a patient’s cancer cells compared with cytotoxic chemotherapeutics and therefore tend to cause fewer adverse effects. In addition, researchers are identifying ways to tailor surgery, radiotherapy, and cytotoxic chemotherapy to minimize their adverse effects without negatively affecting survival. The success of these approaches is highlighted by research showing that significantly fewer survivors of cancer diagnosed in childhood are experiencing and dying because of late effects of cancer treatment, such as a new cancer or heart disease, compared with three decades ago, and that this progress is expected to translate into further improvements in life expectancy for these individuals in the future (300)Armstrong GT, Chen Y, Yasui Y, Leisenring W, Gibson TM, Mertens AC, et al. Reduction in Late Mortality among 5-Year Survivors of Childhood Cancer. N Engl J Med [Internet]. NIH Public Access; 2016 [cited 2019 Jun 20];374:833–42.(439)DA M, G H, KK N, MJ E, Y Y, D D, et al. Major Cardiac Events for Adult Survivors of Childhood Cancer Diagnosed Between 1970 and 1999: Report From the Childhood Cancer Survivor Study Cohort. BMJ [Internet]. BMJ; 2020 [cited 2020 Jul 3];368.(440)Yeh JM, Ward ZJ, Chaudhry A, Liu Q, Yasui Y, Armstrong GT, et al. Life Expectancy of Adult Survivors of Childhood Cancer Over 3 Decades. JAMA Oncol [Internet]. American Medical Association; 2020 [cited 2020 Jul 3];6:350..
Despite advances in cancer treatment that are helping improve quality of life, individuals with a history of cancer consistently report lower general health and quality of life compared with people without such a history. For example, in one study, one in four survivors of cancer diagnosed in adulthood reported a poor physical quality of life and one in 10 reported a poor mental quality of life compared with one in ten and one in 16 people without a history of cancer, respectively (441)Weaver KE, Forsythe LP, Reeve BB, Alfano CM, Rodriguez JL, Sabatino SA, et al. Mental and physical health-related quality of life among U.S. cancer survivors: population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev [Internet]. NIH Public Access; 2012 [cited 2019 Jun 20];21:2108–17.. Therefore, identifying new ways to improve quality of life throughout a patient’s experience with cancer, beginning at diagnosis and continuing through treatment, follow-up, survivorship, and end-of-life care, is an area of intensive research investigation.
Improving quality of life is also important because research suggests that it is linked to cancer-related outcomes, including survivorship. In fact, several strategies, including some of those discussed below, such as outpatient specialty palliative care and exercise, have been shown to improve quality of life and survival (442)Hoerger M, Wayser GR, Schwing G, Suzuki A, Perry LM. Impact of Interdisciplinary Outpatient Specialty Palliative Care on Survival and Quality of Life in Adults With Advanced Cancer: A Meta-Analysis of Randomized Controlled Trials. Ann Behav Med [Internet]. 2019 [cited 2019 Jun 20];53:674–85.(443)MCTIERNAN A, FRIEDENREICH CM, KATZMARZYK PT, POWELL KE, MACKO R, BUCHNER D, et al. Physical Activity in Cancer Prevention and Survival. Med Sci Sport Exerc [Internet]. 2019 [cited 2019 Jun 20];51:1252–61..
Promoting Healthy Behaviors
Evidence is emerging that modifying behaviors to eliminate or avoid many of the lifestyle-related factors that increase a person’s risk of developing cancer, such as cigarette smoking, inactivity, unhealthy diet, and alcohol consumption, can improve outcomes and quality of life for cancer patients and survivors (444)Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin [Internet]. American Cancer Society; 2019 [cited 2019 Jun 19];caac.21565.(445)Blanchard CM, Courneya KS, Stein K, American Cancer Society’s SCS-II. Cancer Survivors’ Adherence to Lifestyle Behavior Recommendations and Associations With Health-Related Quality of Life: Results From the American Cancer Society’s SCS-II. J Clin Oncol [Internet]. 2008 [cited 2019 Jun 20];26:2198–204. (see Preventing Cancer: Identifying Risk Factors).
In addition to being the leading preventable cause of cancer, cigarette smoking can increase risk of death from cancer, risk of cancer recurrence, risk for developing a second cancer, risk of treatment-related toxicity, and risk of a poorer response to treatment (446). Fortunately, patients and survivors with cancer who are current smokers can improve their prognosis by quitting smoking. Quitting smoking can also reduce fear of cancer recurrence, which is an adverse long-term and late effect of cancer and cancer treatment (447)JL W, B T, C SL, S L. Smoking Versus Quitting and Fear of Cancer Recurrence 9 Years After Diagnosis in the American Cancer Society’s Longitudinal Study of Cancer Survivors-I (SCS-I). Cancer [Internet]. Cancer; 2019 [cited 2020 Jul 3];125.. Despite this knowledge, 9 percent of survivors continue to smoke years after a cancer diagnosis and young adults ages 18 to 39 who have a history of cancer are more than 50 percent more likely to have used e-cigarettes compared with their peers who have no history of cancer (448)Westmaas JL, Alcaraz KI, Berg CJ, Stein KD. Prevalence and Correlates of Smoking and Cessation-Related Behavior among Survivors of Ten Cancers: Findings from a Nationwide Survey Nine Years after Diagnosis. Cancer Epidemiol Biomarkers & Prev [Internet]. 2014;23:1783 LP – 1792.. Therefore, more research is needed to develop optimal strategies to provide patients with cancer who smoke with the best chance of quitting smoking, with recent studies suggesting that digital technology and app-based approaches may provide new avenues for promoting smoking cessation (449)(450)JB B, NL W, JL H, B S, K M, D K, et al. A Smartphone App Designed to Help Cancer Patients Stop Smoking: Results From a Pilot Randomized Trial on Feasibility, Acceptability, and Effectiveness. JMIR Form Res [Internet]. JMIR Form Res; 2020 [cited 2020 Jul 3];4.(451)JL W, J B-J, PS H, J K, LC A. Randomised Controlled Trial of Stand-Alone Tailored Emails for Smoking Cessation. Tob Control [Internet]. Tob Control; 2018 [cited 2020 Jul 3];27..
Just as exercising regularly can reduce the risk of developing certain types of cancer, it can also reduce recurrence and mortality for survivors of several types of cancer, including breast cancer, childhood cancer, colorectal cancer, and prostate cancer (443)MCTIERNAN A, FRIEDENREICH CM, KATZMARZYK PT, POWELL KE, MACKO R, BUCHNER D, et al. Physical Activity in Cancer Prevention and Survival. Med Sci Sport Exerc [Internet]. 2019 [cited 2019 Jun 20];51:1252–61.(443)MCTIERNAN A, FRIEDENREICH CM, KATZMARZYK PT, POWELL KE, MACKO R, BUCHNER D, et al. Physical Activity in Cancer Prevention and Survival. Med Sci Sport Exerc [Internet]. 2019 [cited 2019 Jun 20];51:1252–61.(453)Scott JM, Li N, Liu Q, Yasui Y, Leisenring W, Nathan PC, et al. Association of Exercise With Mortality in Adult Survivors of Childhood Cancer. JAMA Oncol [Internet]. 2018 [cited 2018 Jun 8];(454)MS F, KA K, KS C, SE M, Q W, CM F. Associations of Postdiagnosis Physical Activity and Change From Prediagnosis Physical Activity With Quality of Life in Prostate Cancer Survivors. Cancer Epidemiol Biomarkers Prev [Internet]. Cancer Epidemiol Biomarkers Prev; 2017 [cited 2020 Jul 3];26.. In addition, exercise can improve overall quality of life for patients and survivors who are undergoing treatment for cancer and for those who have completed treatment (454)MS F, KA K, KS C, SE M, Q W, CM F. Associations of Postdiagnosis Physical Activity and Change From Prediagnosis Physical Activity With Quality of Life in Prostate Cancer Survivors. Cancer Epidemiol Biomarkers Prev [Internet]. Cancer Epidemiol Biomarkers Prev; 2017 [cited 2020 Jul 3];26.(455)Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev [Internet]. 2012 [cited 2019 Jun 20];CD007566.(456)Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C. The Effectiveness of Exercise Interventions for Improving Health-Related Quality of Life From Diagnosis Through Active Cancer Treatment. Oncol Nurs Forum [Internet]. 2015 [cited 2019 Jun 20];42:E33–53.. More specifically, exercise during and after treatment is completed has been shown to alleviate many of the adverse long-term and late effects of cancer and cancer treatments, including anxiety, depression, cognitive impairment, fatigue, lymphedema, pain, peripheral neuropathy, and poor sleep quality, and to improve heart and lung function (457)Mustian KM, Alfano CM, Heckler C, Kleckner AS, Kleckner IR, Leach CR, et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue. JAMA Oncol [Internet]. 2017 [cited 2019 Jun 20];3:961.(458)Craft LL, VanIterson EH, Helenowski IB, Rademaker AW, Courneya KS. Exercise Effects on Depressive Symptoms in Cancer Survivors: A Systematic Review and Meta-Analysis. Cancer Epidemiol Biomarkers Prev [Internet]. NIH Public Access; 2012 [cited 2019 Jun 20];21:3.(459)ROGERS LQ, COURNEYA KS, OSTER RA, ANTON PM, ROBBS RS, FORERO A, et al. Physical Activity and Sleep Quality in Breast Cancer Survivors. Med Sci Sport Exerc [Internet]. 2017 [cited 2019 Jun 20];49:2009–15.(460)Irwin ML, Cartmel B, Gross CP, Ercolano E, Li F, Yao X, et al. Randomized Exercise Trial of Aromatase Inhibitor–Induced Arthralgia in Breast Cancer Survivors. J Clin Oncol [Internet]. American Society of Clinical Oncology; 2015 [cited 2019 Jun 20];33:1104.(461)Kleckner IR, Kamen C, Gewandter JS, Mohile NA, Heckler CE, Culakova E, et al. Effects of exercise during chemotherapy on chemotherapy-induced peripheral neuropathy: a multicenter, randomized controlled trial. Support Care Cancer [Internet]. 2018 [cited 2019 Jun 20];26:1019–28.(462)Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med [Internet]. BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2018 [cited 2019 Jun 20];52:154–60.(463)Scott JM, Zabor EC, Schwitzer E, Koelwyn GJ, Adams SC, Nilsen TS, et al. Efficacy of Exercise Therapy on Cardiorespiratory Fitness in Patients With Cancer: A Systematic Review and Meta-Analysis. J Clin Oncol [Internet]. 2018 [cited 2019 Jun 20];36:2297–305.. The beneficial effect of exercise on heart function among patients with cancer is particularly important because research shows that many patients with cancer are at increased risk of death from cardiovascular disease, in particular, those who have bladder cancer, breast cancer, or prostate cancer (463)Scott JM, Zabor EC, Schwitzer E, Koelwyn GJ, Adams SC, Nilsen TS, et al. Efficacy of Exercise Therapy on Cardiorespiratory Fitness in Patients With Cancer: A Systematic Review and Meta-Analysis. J Clin Oncol [Internet]. 2018 [cited 2019 Jun 20];36:2297–305.(464).
Eating a diet rich in vegetables, fruits, and whole grains, or a diet high in fiber, reduces a person’s risk of developing or dying from some types of cancer, in particular, colorectal cancer, and can improve quality of life after a cancer diagnosis (465)Van Blarigan EL, Fuchs CS, Niedzwiecki D, Zhang S, Saltz LB, Mayer RJ, et al. Association of Survival With Adherence to the American Cancer Society Nutrition and Physical Activity Guidelines for Cancer Survivors After Colon Cancer Diagnosis. JAMA Oncol [Internet]. 2018 [cited 2018 May 7];(466)(445)Blanchard CM, Courneya KS, Stein K, American Cancer Society’s SCS-II. Cancer Survivors’ Adherence to Lifestyle Behavior Recommendations and Associations With Health-Related Quality of Life: Results From the American Cancer Society’s SCS-II. J Clin Oncol [Internet]. 2008 [cited 2019 Jun 20];26:2198–204.. Conversely, consuming alcohol increases risk of death from prostate cancer after a prostate cancer diagnosis, and consuming from three to four alcoholic drinks a week increases risk of recurrence among patients and survivors with breast cancer (467)MS F, KS C, KA K, SE M, CM F. Post-diagnosis Alcohol Intake and Prostate Cancer Survival: A Population-Based Cohort Study. Int J cancer [Internet]. Int J Cancer; 2018 [cited 2020 Jul 3];143.(468)Kwan ML, Kushi LH, Weltzien E, Tam EK, Castillo A, Sweeney C, et al. Alcohol Consumption and Breast Cancer Recurrence and Survival Among Women With Early-Stage Breast Cancer: The Life After Cancer Epidemiology Study. J Clin Oncol [Internet]. American Society of Clinical Oncology; 2010 [cited 2020 Jul 3];28:4410.. Despite this knowledge, more than half of a group of 34,080 survivors of various types of cancer reported that they currently drank alcohol regularly, with 21 percent of these drinkers saying that they engaged in binge drinking (469).
The growing body of evidence that modifying lifestyle-related behaviors, such as physical inactivity, unhealthy diet, and alcohol consumption can improve outcomes and quality of life for cancer patients and survivors has led experts to recommend that cancer patients and survivors achieve and maintain a healthy body weight, participate in regular physical activity, and eat a diet rich in vegetables, fruits, and whole grains (178)Rock CL, Thomson C, Gansler T, Gapstur SM, McCullough ML, Patel A V., et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin [Internet]. American Cancer Society; 2020 [cited 2020 Jul 3];caac.21591..
Palliative Care
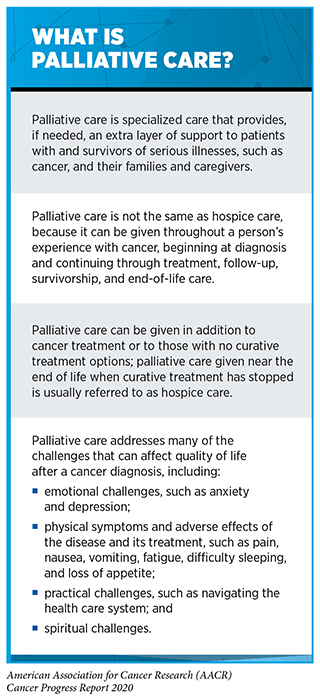
Palliative care is one approach that is being increasingly used to optimize the quality of life for patients and survivors with cancer, as well as their families and caregivers (see sidebar on What Is Palliative Care?). Palliative care can be given throughout a person’s experience with cancer, beginning at diagnosis and continuing through treatment, follow-up, survivorship, and end-of-life care. The goal is not to treat the cancer but to provide an extra layer of care that prevents or treats the symptoms and adverse effects of the disease and its treatment, as well as addresses the psychological, social, and spiritual challenges that accompany a cancer diagnosis.
Recent research shows that integrating palliative care during the early stages of cancer care can significantly improve quality of life and survival, and lower hospital costs (442)Hoerger M, Wayser GR, Schwing G, Suzuki A, Perry LM. Impact of Interdisciplinary Outpatient Specialty Palliative Care on Survival and Quality of Life in Adults With Advanced Cancer: A Meta-Analysis of Randomized Controlled Trials. Ann Behav Med [Internet]. 2019 [cited 2019 Jun 20];53:674–85.(470)(471)P M, C N, RS M. Economics of Palliative Care for Cancer: Interpreting Current Evidence, Mapping Future Priorities for Research. J Clin Oncol [Internet]. J Clin Oncol; 2020 [cited 2020 Jul 3];38.. Despite this, the only growth in palliative care infrastructure that has occurred in the past decade is in outpatient palliative care clinics at NCI‐designated cancer centers. There has been no increase in inpatient consultation teams, palliative care units, and institution‐operated hospices at either NCI‐designated cancer centers or at non–NCI‐designated cancer centers, and there has been no increase in outpatient palliative care clinics at non–NCI‐designated cancer centers (472)Hui D, De La Rosa A, Chen J, Dibaj S, Delgado Guay M, Heung Y, et al. State of palliative care services at US cancer centers: An updated national survey. Cancer [Internet]. John Wiley & Sons, Ltd; 2020 [cited 2020 Jul 3];126:2013–23..
It is imperative that we increase awareness of the important role that palliative care can play across the continuum of clinical cancer care because many patients do not receive palliative care and many patients and caregivers do not even know what palliative care is (473)Amy Compton-Phillips M&, Namita Seth Mohta M. Care Redesign Survey: The Power of Palliative Care [Internet]. [cited 2020 Jul 3].(474)Dionne-Odom JN, Ornstein KA, Kent EE. What do family caregivers know about palliative care? Results from a national survey. Palliat Support Care [Internet]. NIH Public Access; 2019 [cited 2020 Jul 3];17:643.. One study found that patients with cancer were more likely to express a preference for early outpatient palliative care after being provided a web-based, plain-language and graphical summary about palliative care as well as the results of a clinical trial which showed that palliative cancer care improved physical quality of life, depression, and survival for patients with metastatic lung cancer (475)Hoerger M, Perry LM, Gramling R, Epstein RM, Duberstein PR. Does educating patients about the Early Palliative Care Study increase preferences for outpatient palliative cancer care? Findings from Project EMPOWER. Health Psychol [Internet]. NIH Public Access; 2017 [cited 2020 Jul 3];36:538.. It will be important to determine whether such programs benefit all segments of the U.S. population because it has been reported that there are disparities in the use of palliative care among patients with cancer (434)Lee K, Gani F, Canner JK, Johnston FM. Racial Disparities in Utilization of Palliative Care Among Patients Admitted With Advanced Solid Organ Malignancies. Am J Hosp Palliat Med [Internet]. SAGE PublicationsSage CA: Los Angeles, CA; 2020 [cited 2020 Jul 3];104990912092277..
Psycho-oncology
Psycho-oncology is a field of research and branch of medicine that encompasses the work of researchers and health care providers committed to developing new approaches to addressing the behavioral, emotional, psychological, and social challenges posed by cancer (see sidebar on Helping Patients with Cancer through Psycho-oncology Research). Addressing these challenges, which include treatment-related cognitive impairment, fear of cancer recurrence, anxiety, depression, stress, posttraumatic stress disorder, and feelings of despair, is important not just for improving quality of life, but also for improving outcomes because challenges such as depression, anxiety, and low levels of social support are often associated with decreased adherence to cancer treatment and/or decreased survival (476)(477)(478)Pinquart M, Duberstein PR. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol [Internet]. NIH Public Access; 2010 [cited 2020 Aug 3];75:122–37.. Given the benefits of psycho-oncology, it is vital that all patients with cancer for whom this intervention is appropriate receive this care.
Delivering Care to Cancer Survivors
As an increasing number of people are surviving longer after a cancer diagnosis, it has become increasingly clear that the transition from initial cancer treatment to follow-up, long-term survivorship care can be complex.
Coordinating Care
Most survivors of cancer have poorer health and quality of life than other individuals of a similar age who have no history of cancer. They are also at increased risk for long-term morbidity and premature mortality due to their cancer diagnosis and treatment. Therefore, survivors have complex health care needs that are best met by a wide range of health care professionals (481)Kline RM, Arora NK, Bradley CJ, Brauer ER, Graves DL, Lunsford NB, et al. Long-Term Survivorship Care After Cancer Treatment – Summary of a 2017 National Cancer Policy Forum Workshop. JNCI J Natl Cancer Inst [Internet]. Oxford Academic; 2018 [cited 2020 Jul 3];110:1300–10..
Emerging evidence suggests that survivors of cancer receive the highest level of care if their care is well coordinated, either by an oncologist and primary care physician, by multiple specialists, or by an oncogeneralist—a primary care physician with specific expertise in caring for patients and survivors with cancer (481)Kline RM, Arora NK, Bradley CJ, Brauer ER, Graves DL, Lunsford NB, et al. Long-Term Survivorship Care After Cancer Treatment – Summary of a 2017 National Cancer Policy Forum Workshop. JNCI J Natl Cancer Inst [Internet]. Oxford Academic; 2018 [cited 2020 Jul 3];110:1300–10.(482)L N, DM O, SV H. Integrating Primary Care Providers in the Care of Cancer Survivors: Gaps in Evidence and Future Opportunities. Lancet Oncol [Internet]. Lancet Oncol; 2017 [cited 2020 Jul 3];18.(438)Shapiro CL. Cancer Survivorship. Longo DL, editor. N Engl J Med [Internet]. 2018 [cited 2019 Jun 20];379:2438–50.(438)Shapiro CL. Cancer Survivorship. Longo DL, editor. N Engl J Med [Internet]. 2018 [cited 2019 Jun 20];379:2438–50.. However, we need to identify the optimal way to provide comprehensive, coordinated care to all survivors of cancer and ensure that it benefits patients by improving cancer-related outcomes and health-related quality of life (481)Kline RM, Arora NK, Bradley CJ, Brauer ER, Graves DL, Lunsford NB, et al. Long-Term Survivorship Care After Cancer Treatment – Summary of a 2017 National Cancer Policy Forum Workshop. JNCI J Natl Cancer Inst [Internet]. Oxford Academic; 2018 [cited 2020 Jul 3];110:1300–10.(484)Alfano CM, Mayer DK, Bhatia S, Maher J, Scott JM, Nekhlyudov L, et al. Implementing personalized pathways for cancer follow‐up care in the United States: Proceedings from an American Cancer Society–American Society of Clinical Oncology summit. CA Cancer J Clin [Internet]. American Cancer Society; 2019 [cited 2019 Jul 29];69:234–47..
The Important Role of Caregivers
Caregivers provide an extension to a cancer survivor’s health care team. They play a vital role throughout a patient’s experience with cancer, from diagnosis through long-term survivorship. The population of caregivers is growing proportionally with the number of cancer survivors. One recent study of caregiving in 18 states in the United States led researchers to estimate that there are 1.1 million family caregivers of adults with cancer living in these states and that more than one in five of these people were caregiving for more than 20 hours per week (485)Kent EE, Dionne-Odom JN. Population-Based Profile of Mental Health and Support Service Need Among Family Caregivers of Adults With Cancer. J Oncol Pract [Internet]. American Society of Clinical Oncology; 2019 [cited 2019 Jun 20];15:e122–31..
It is important to note that caregivers are at risk for poor health outcomes, in particular poor mental health outcomes. However, research shows that those who are caregiving for longer hours experience worse outcomes (485)Kent EE, Dionne-Odom JN. Population-Based Profile of Mental Health and Support Service Need Among Family Caregivers of Adults With Cancer. J Oncol Pract [Internet]. American Society of Clinical Oncology; 2019 [cited 2019 Jun 20];15:e122–31.. Research such as this is bringing increasing awareness to the need for new strategies to optimize and tailor support for caregivers.