- Challenges Faced by Cancer Survivors
- Physical Challenges
- Psychosocial Challenges
- Financial Challenges
- Unique Challenges Faced by Children, Adolescents, and Young Adults with Cancer
- Challenges Faced by Racial and Ethnic Minorities and Other Underserved Populations
- Improving Quality of Life and Outcomes for Cancer Survivors Across the Continuum of Cancer Care
- Delivering Care to Cancer Survivors
Supporting Cancer Patients and Survivors
In this section, you will learn:
- As of 2019, more than five percent of the U.S. population is living with a history of cancer.
- Each person diagnosed with cancer faces a unique set of challenges; 25 percent of cancer survivors report poor physical health and 10 percent report poor mental health, both adversely affecting quality of life.
- Researchers are exploring ways to utilize healthy behaviors, palliative care, psycho-oncology, and other evidence-based strategies to improve survival and quality of life for patients with cancer.
- Additional research is pivotal to tailor new technologies and intervention strategies for coordinated care that improves the quality of life and meets the personalized needs of cancer survivors and caregivers from different age groups.
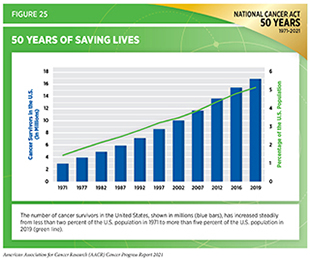
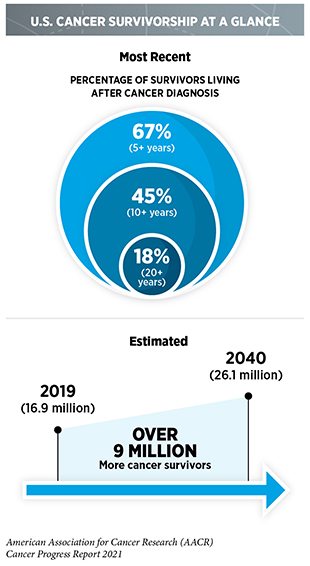
Discovery science-driven clinical breakthroughs across the continuum of cancer care are saving lives and helping individuals live longer and fuller lives after a cancer diagnosis. In 2019, the most recent year for which such data are available, cancer survivors accounted for more than five percent of the entire U.S. population, a remarkable improvement since 1971, when cancer survivors made up only 1.4 percent of the U.S. population (Figure 25). Thanks to the dedication of countless individuals across all sectors of health care and policy, cancer survivors are projected to account for nearly seven percent of the U.S. population by 2040.
According to the National Cancer Institute (NCI), a person is considered a cancer survivor from the time of cancer diagnosis through the balance of his or her life. While a person is considered a survivor from the time of cancer diagnosis through the remainder of life, not everyone identifies or agrees with this term. Each person who is diagnosed with cancer has a unique experience. These experiences range from successful treatment and living cancer free for the remainder of life, with or without adverse effects of treatment, to living with cancer and any effects of treatment for the remainder of life. Furthermore, as our understanding of cancer survivorship increases, there is a growing appreciation of its multifaceted impact on family members, friends, and caregivers of those diagnosed with cancer (523)National Coalition for Cancer Surviorship. Defining cancer survivorship. 2014 Jul 24..
Challenges Faced by Cancer Survivors
Depending on the type and stage of cancer, as well as the age at which an individual is diagnosed, cancer survivorship can encompass a wide range of unique experiences of living with, through, and beyond cancer (see sidebar on Phases of Cancer Survivorship).
Physical, psychosocial, and financial stresses can deprive individuals diagnosed with cancer of meaningful life experiences regardless of which phase of survivorship the individual is experiencing. These challenges can also disrupt the lives of family members, friends, and other caregivers. It is important to note that the challenges discussed here are interrelated and may collectively contribute to the burden of cancer faced by cancer patients and survivors. For example, limited physical mobility because of cancer treatment and/or financial difficulties of paying for medical bills can lead to distress and/or depression.
Physical Challenges
Individuals diagnosed with cancer can face both acute and chronic symptoms from the cancer itself, as well as from the treatment. Both short- and long-term symptoms experienced by cancer survivors can be debilitating. Before and during cancer treatment, individuals may experience a variety of symptoms, including hair loss, pain, swelling of arms and legs (lymphedema), joint pain (arthritis), loss of sleep, nausea, vomiting, and loss of appetite. Long-term effects of cancer and cancer treatment include heart damage (cardiotoxicity), lung (pulmonary) damage, loss of bone density (osteoporosis), excess body fat, nerve issues (peripheral neuropathy), cognitive decline, premature aging, infertility, and sexual dysfunction as well as development of secondary cancers (see sidebar on Phases of Cancer Survivorship). For example, among more than 1.5 million adults who were diagnosed with cancer between 1992 and 2011 and survived five years or more, male and female survivors were at a 45 and 33 percent higher risk, respectively, of dying from a new type of cancer (182)Sung H, Hyun N, Leach CR, Yabroff KR, Jemal A. Association of first primary cancer with risk of subsequent primary cancer among survivors of adult-onset cancers in the United States. JAMA – J Am Med Assoc. 2020;324(24).. Ongoing research is aimed at understanding the risk factors that make patients susceptible to these late effects and ways to prevent them. Emerging evidence suggests that an active and healthy lifestyle can play an important role in coping with deleterious effects of cancer treatment, such as cardiopulmonary dysfunction (see Promoting Healthy Behaviors). Furthermore, palliative care—a specialized type of care that provides an additional level of support for cancer survivors throughout their experience with cancer—can significantly improve quality of life (see Palliative Care).
Psychosocial Challenges
Cancer diagnosis and treatment pose serious challenges to a person’s mental and emotional health. Anxiety of cancer returning or concern of being diagnosed with a new type of cancer even after successful cancer treatment can lead to distress and/or depression. A recent study found that survivors of stomach cancer had anxiety that was associated with fear of cancer recurrence (524)J S, DW S, J L, et al. Fear of Cancer Recurrence in Stomach Cancer Survivors: Exploring Socio-Demographic, Physical, Psychological and Quality of Life-Related Factors. Published online April 2021.. Similarly, individuals who are under active surveillance after diagnosis of early-stage cancer that does not require therapy also face the anxiety and distress of cancer eventually progressing. For example, patients diagnosed with an early-stage prostate cancer who were under active surveillance often reported feeling anxious, depressed, uncertain and/or hopeless (525)Biddle S. The psychological impact of active surveillance in men with prostate cancer: Implications for nursing care. Br J Nurs. 2021;30(10).. Impairment of cognitive skills due to cancer treatment, such as loss of memory, decline in the ability to learn new things, trouble concentrating, and/or indecisive attitude, can affect everyday life. Studies have shown that an estimated 10-30 percent of cancer patients exhibit detectable cognitive impairment even before cancer treatment, likely due to the distress and anxiety caused by the cancer diagnosis. Approximately 15-35 percent of cancer patients reported diminished cognitive functions several months after completion of cancer treatment (526)Hutterer M, Oberndorfer S. Cognitive impairment in cancer patients and survivors—clinical presentation, pathophysiology, diagnosis and management. Memo – Mag Eur Med Oncol. 2021;14(2).. Late effects of cancer diagnosis and treatment are yet another source of anxiety and distress among long-term survivors of cancer. A recent study found that many survivors of prostate cancer reported a feeling of abandonment and lack of psychosocial and informational support to address persisting treatment-induced side effects (527)Mazariego CG, Laidsaar-Powell R, Smith DP, Juraskova I. Avoiding the ‘survivorship abyss’: Qualitative insights from 15-year prostate cancer survivors. Psychooncology. Published online 2021.. Increased understanding of the far-reaching impact of cancer on a person’s life has spurred the field of psycho-oncology, an interdisciplinary approach to providing support for cancer patients confronting numerous behavioral, emotional, psychological, and social challenges throughout the different stages of survivorship (see Psycho-oncology).
Financial Challenges
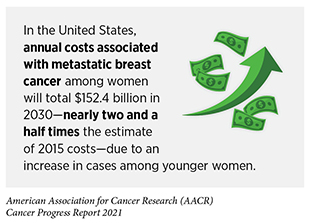
Financial hardship, or financial toxicity, associated with cancer treatment and management poses a key challenge to the mental and emotional health of the individual diagnosed with cancer, as well as that of immediate family members who may depend on the cancer survivor for their livelihood. Accruing evidence points to the many ways by which financial hardship affects cancer survivors and their dependents. In one recent survey of patients with gynecologic cancers, nearly half of the participants reported that they faced moderate (such as borrowing money) to severe (such as unable to pay for prescription medication) financial hardship because of cancer treatment and management (528)Esselen KMK, Gompers A, Hacker MR, et al. Evaluating meaningful levels of financial toxicity in gynecologic cancers. Int J Gynecol Cancer. 2021;31(6).. Another study examining the financial impact on survivors 70 years or older who had advanced-stage cancer found that 18 percent of the participants experienced financial toxicity and higher levels of depression, anxiety, and distress (529)Arastu A, Patel A, Mohile SG, et al. Assessment of Financial Toxicity Among Older Adults With Advanced Cancer. JAMA Netw open. 2020;3(12):e2025810.. Cancer diagnosis can also adversely affect employment, further exacerbating financial hardship. According to one study, financial hardship was twice as likely among women who had to stop working completely or reduce work hours because of a breast cancer diagnosis (530)Meernik C, Sandler DP, Peipins LA, et al. Breast Cancer–Related Employment Disruption and Financial Hardship in the Sister Study. JNCI Cancer Spectr. 2021;5(3)..
Unique Challenges Faced by Children, Adolescents, and Young Adults with Cancer
Coping with the adverse effects of cancer is even more challenging for those diagnosed during childhood, adolescence, and young adulthood (i.e., individuals from ages less than one year to 39 years)(532)Erdmann F, Frederiksen LE, Bonaventure A, et al. Childhood cancer: Survival, treatment modalities, late effects and improvements over time. Cancer Epidemiol. 2021;71.. This period in life is associated with major changes at personal, social, and emotional levels. Many young adults are only starting their journey to professional careers. A cancer diagnosis during this phase of life can irrevocably change their personal and occupational trajectories (533)Ghazal LV, Merriman J, Santacroce SJ, Dickson VV. Survivors’ Dilemma: Young Adult Cancer Survivors’ Perspectives of Work-Related Goals. Work Heal Saf. Published online 2021.. Cancer survivors in this group are at a greater risk of developing additional medical conditions, such as stroke, secondary cancers, and neurodegenerative defects, compared to the general population. This risk can increase further depending upon the type of treatment they received. A recent study performed a 10-year follow-up of nearly 7,000 AYA, who had survived two years or more after cancer diagnosis, for the presence of medical conditions, including cardiovascular issues, hypertension, diabetes, and pulmonary diseases. Researchers found that 40 percent of AYA who were cancer survivors had two or more comorbidities compared to those without cancer (534)Chao C, Bhatia S, Xu L, et al. Chronic comorbidities among survivors of adolescent and young adult cancer. J Clin Oncol. 2020;38(27).. According to a recent study, 32 percent of AYA women experienced disruption in their employment status (left or lost job or had to reduce their work hours) after they were diagnosed with cancer (535)Meernik C, Kirchhoff AC, Anderson C, et al. Material and psychological financial hardship related to employment disruption among female adolescent and young adult cancer survivors. Cancer. 2020;127(1).. Because of the unique challenges faced by younger individuals who are diagnosed with cancer, the Children’s Oncology Group has developed guidelines to help standardize and improve the lifelong follow-up care of these individuals (536)Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. Version 5.0 – October 2018. [cited 2021 Jul 10]..
Challenges Faced by Racial and Ethnic Minorities and Other Underserved Populations
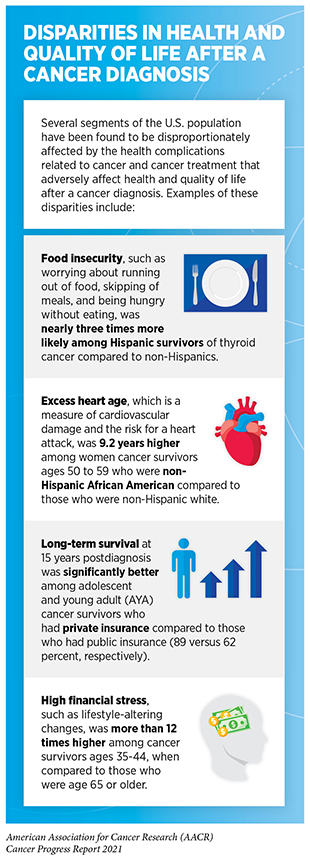
Cancer survivors who belong to certain underserved segments of the U.S. population face additional challenges while coping with the cancer burden, a collective term to describe varied needs of a cancer survivor throughout the cancer experience. Numerous disparities, stemming largely from systemic and structural racism and discrimination, disproportionately and adversely affect the health and quality of life of cancer survivors from underserved population groups. As an example, African American women diagnosed with breast cancer were less likely to receive a timely surveillance mammogram compared to whites (537)Advani P, Advani S, Nayak P, et al. Racial/ethnic disparities in use of surveillance mammogram among breast cancer survivors: a systematic review. J Cancer Surviv. Published online 2021.(see sidebar on Disparities in Health and Quality of Life After a Cancer Diagnosis).
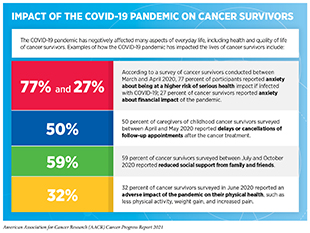
The COVID-19 pandemic has further exacerbated the numerous challenges faced by cancer survivors (see sidebar on Impact of the COVID-19 Pandemic on Cancer Survivors). Although long-term effects of the pandemic on cancer survivors will be clearer with time, preliminary indications point to the impacts of the pandemic that range from worsening of physical, psychosocial, and financial well-being to exploration of new opportunities such as adapting to technology-based means of health care delivery.
Improving Quality of Life and Outcomes for Cancer Survivors Across the Continuum of Cancer Care
The NCI defines quality of life as the overall enjoyment of life measured by aspects of an individual’s sense of well-being and ability to carry out activities of daily living. Because the impact of cancer diagnosis and treatment on a person is multifaceted and far-reaching (see Challenges Faced by Cancer Survivors), the notion of quality of life throughout cancer survivorship (see sidebar on Stages of Cancer Survivorship) is also multidimensional and includes physical, psychosocial, emotional, and financial well-being. As more cancer survivors are living longer, the concept of quality of life has become an integral part of the cancer care continuum as well as a focus of intense research.
Advances in treating cancer based on specific genetic mutations or biomarkers are improving long-term survival of cancer patients (546)Kato S, Kim KH, Lim HJ, et al. Real-world data from a molecular tumor board demonstrates improved outcomes with a precision N-of-One strategy. Nat Commun. 2020;11(1).(547)Tsimberidou AM, Hong DS, Wheler JJ, et al. Long-term overall survival and prognostic score predicting survival: The IMPACT study in precision medicine. J Hematol Oncol. 2019;12(1).. Today, many cancer survivors are experiencing improved quality of life and living their lives as active members of society. This success is reflected in the cancer experience of Zach Witt, now a 16-year-old high school student, who was treated with a molecularly targeted therapeutic when he was diagnosed with a certain type of lymphoma as a 9-year-old.
Longer survival among cancer patients following treatment with molecularly targeted therapeutics and immunotherapeutics also comes with the possibility of long-term or late effects from these treatments (548)Zhang Q, Fu Q, Bai X, Liang T. Molecular Profiling–Based Precision Medicine in Cancer: A Review of Current Evidence and Challenges. Front Oncol. 2020;10.. For example, according to a recent report, poly ADP-ribose polymerase (PARP) inhibitors, a class of molecular therapeutics that target the DNA repair pathway in cancer cells, more than doubled the risk of myelodysplastic syndrome and acute myeloid leukemia among recipients when compared to the placebo treatment (549)Morice P-M, Leary A, Dolladille C, et al. Myelodysplastic syndrome and acute myeloid leukaemia in patients treated with PARP inhibitors: a safety meta-analysis of randomised controlled trials and a retrospective study of the WHO pharmacovigilance database. Another recent study showed that 43 percent of melanoma patients who were treated with immunotherapeutics developed long-term immune-related side effects (511)Patrinely JR, Johnson R, Lawless AR, et al. Chronic immune-related adverse events following adjuvant anti-PD-1 therapy for high-risk resected melanoma. JAMA Oncol. 2021;7(5).. These findings emphasize the need to carefully monitor the adverse side effects of newer treatments such as targeted therapeutics and immunotherapeutics and to identify ways to help cancer survivors cope with short-term, long-term, and late effects of their treatments. Researchers are exploring various strategies to improve the survival and quality of life of cancer survivors. Some of these approaches are discussed below.
Promoting Healthy Behaviors
Certain lifestyle changes can significantly improve quality of life for cancer survivors. These include eliminating tobacco use, adopting a healthy diet, increasing physical activity, and reducing alcohol consumption. Accruing evidence suggests that continued adherence to unhealthy lifestyle behaviors increases the risk of secondary cancers and overall mortality and decreases overall health and quality of life among cancer survivors (550)Hirschey R, Nyrop KA, Mayer DK. Healthy behaviors: Prevalence of uptake among cancer survivors. Clin J Oncol Nurs. 2020;24(5)..
Tobacco use is causally linked to significantly increased risk of developing at least 18 different types of cancer (see Preventing Cancer: Identifying Risk Factors). Smoking tobacco is also associated with worse outcomes after a cancer diagnosis (551)Jassem J. Tobacco smoking after diagnosis of cancer: Clinical aspects. Transl Lung Cancer Res. 2019;8.. A recent study found that smoking cessation among cancer survivors decreased their risk of dying because of cancer by 25 percent (552)Sheikh M, Mukeriya A, Shangina O, Brennan P, Zaridze D. Postdiagnosis Smoking Cessation and Reduced Risk for Lung Cancer Progression and Mortality. Ann Intern Med. Published online 2021.. Among cancer survivors diagnosed between 2000 and 2017, more than 24 percent were smokers at the time of first cancer diagnosis. Encouragingly, the likelihood of cigarette smoking cessation among cancer survivors increased with the year of cancer diagnosis from 2000 to 2017 (553)Talluri R, Fokom Domgue J, Gritz ER, Shete S. Assessment of Trends in Cigarette Smoking Cessation After Cancer Diagnosis Among US Adults, 2000 to 2017. JAMA Netw open. 2020;3(8).. Another study found that successful cessation of cigarette smoking among survivors of bladder cancer was more frequent around the time of initial diagnosis (554)Bassett JC, Matulewicz RS, Kwan L, McCarthy WJ, Gore JL, Saigal CS. Prevalence and Correlates of Successful Smoking Cessation in Bladder Cancer Survivors. Urology. Published online 2021.. These promising findings underscore the opportunity to educate cancer survivors about how cigarette smoking can negatively impact cancer treatment and survival. There is also an opportunity to develop new and innovative strategies such as those based on digital health, e.g., internet and smartphone applications, that promote smoking cessation among cancer survivors. There is preliminary evidence that using smartphone applications among cancer survivors for cessation of smoking can be effective (555)Vinci C. Cognitive Behavioral and Mindfulness-Based Interventions for Smoking Cessation: a Review of the Recent Literature. Curr Oncol Rep. 2020;22(6).. Additional research is underway to develop evidence-based approaches that use a range of modern means of communication to encourage smoking cessation among cancer survivors (556)Asfar T, Koru-Sengul T, Annane D, et al. Reach versus effectiveness: The design and protocol of randomized clinical trial testing a smartphone application versus in-person mindfulness-based smoking cessation intervention among young cancer survivors. Cont.
An active lifestyle that includes exercising regularly and participating in outdoor activities is beneficial to everyone (see Preventing Cancer: Identifying Risk Factors). An active lifestyle is especially valuable for cancer survivors because it can help mitigate numerous physical and psychosocial challenges they experience. As an example, prostate cancer survivors who participated in an exercise program reported significant improvements in their physical, mental, and emotional health (557)Mardani A, Pedram Razi S, Mazaheri R, Haghani S, Vaismoradi M. Effect of the exercise programme on the quality of life of prostate cancer survivors: A randomized controlled trial. Int J Nurs Pract. 2021;27(2).. Similarly, breast cancer patients who maintained an active lifestyle after cancer diagnosis and through the course of treatment had reduced recurrence of cancer, decreased mortality, and improved overall survival (558)Cannioto RA, Hutson A, Dighe S, et al. Physical Activity Before, During, and After Chemotherapy for High-Risk Breast Cancer: Relationships With Survival. J Natl Cancer Inst. 2021;113(1):54-63.(559)Li Q, Lesseur C, Santella RM, Parada H, Teitelbaum S, Chen J. The Associations Of Healthy Lifestyle Index With Breast Cancer Incidence And Mortality In A Population-Based Study. Published online June 2021.. Maintaining a healthy lifestyle is also associated with reducing the risk of cardiovascular disease and improving bone health among cancer survivors (560)Kwan ML, Lo JC, Laurent CA, et al. A prospective study of lifestyle factors and bone health in breast cancer patients who received aromatase inhibitors in an integrated healthcare setting. J Cancer Surviv. Published online 2021.(561)Kim KH, Choi S, Kim K, et al. Association between physical activity and subsequent cardiovascular disease among 5-year breast cancer survivors. Breast Cancer Res Treat. 2021;188(1).. Researchers are examining additional ways to encourage cancer survivors to maintain an active lifestyle after diagnosis. One study found that cancer survivors exercise at a higher intensity during outdoor compared to indoor exercise sessions (562)Miller JM, Sadak KT, Shahriar AA, et al. Cancer survivors exercise at higher intensity in outdoor settings: The GECCOS trial. Pediatr Blood Cancer. 2021;68(5).. The popularity of fitness trackers has given health care providers additional tools to implement innovative strategies that capitalize on the benefits of an active lifestyle for cancer survivors. Early studies have shown that the use of fitness trackers can reduce sedentary behavior and increase moderate-to-vigorous-intensity physical activity, which is associated with improved mental health and performance (563)Blount DS, McDonough DJ, Gao Z. Effect of Wearable Technology-Based Physical Activity Interventions on Breast Cancer Survivors’ Physiological, Cognitive, and Emotional Outcomes: A Systematic Review. J Clin Med. 2021;10(9).. Use of digital health approaches is especially effective among AYA, a population group that is already adept in applying technology-based solutions across various aspects of their lives. In one recent study, cancer patients ages 15 to 29 were offered a wearable fitness tracker and a tablet at the time of cancer diagnosis to track their physical activity. Those who participated in the study showed increased physical activity and improvements across multiple measures of quality of life (564)Yurkiewicz IR, Simon P, Liedtke M, Dahl G, Dunn T. Effect of fitbit and ipad wearable technology in health-related quality of life in adolescent and young adult cancer patients. J Adolesc Young Adult Oncol. 2018;7(5).. Ongoing studies are further investigating the benefit of such approaches for improving management of short-term, long-term, and late effects of living with cancer (565)Phillips S, Solk P, Welch W, et al. A technology-based physical activity intervention for patients with metastatic breast cancer (Fit2ThriveMB): Protocol for a randomized controlled trial. JMIR Res Protoc. 2021;10(4)..
Eating a balanced diet that includes the major food groups—vegetables, whole grains, fruits, and protein—is central to developing and maintaining a well-rounded healthy lifestyle. Healthy eating habits improve quality of life for cancer survivors. One study found that adherence to a healthy diet was associated with reduced risk of cancer recurrence or death among long-term breast cancer survivors (566)Wang F, Cai H, Gu K, et al. Adherence to dietary recommendations among long-term breast cancer survivors and cancer outcome associations. Cancer Epidemiol Biomarkers Prev. 2020;29(2).. Unfortunately, there are concerning reports that indicate a lack of adherence to dietary recommendations among cancer survivors (567)Entwistle MR, Schweizer D, Cisneros R. Adherence to dietary patterns among cancer survivors in the United States. J Public Heal. Published online 2021.(568)Krok-Schoen JL, Pisegna J, Arthur E, Ridgway E, Stephens C, Rosko AE. Prevalence of lifestyle behaviors and associations with health-related quality of life among older female cancer survivors. Support Care Cancer. 2021;29(6).. A recent study found that alcohol consumption, which is linked with elevated risk for several cancer types, was increased among survivors of head and neck cancer within two years of diagnosis (569)Teckie S, Wotman M, Marziliano A, et al. Patterns of alcohol use among early head and neck cancer survivors: A cross-sectional survey study using the alcohol use disorders identification test (AUDIT). Oral Oncol. 2021;119.. Notably, the lack of easily understandable information on healthy eating and absence of support for changing dietary behaviors have been reported as two major barriers to adopting a healthy diet among cancer survivors (570)Johnston EA, van der Pols JC, Ekberg S. Needs, preferences, and experiences of adult cancer survivors in accessing dietary information post-treatment: A scoping review. Eur J Cancer Care (Engl). 2021;30(2).. These findings highlight the urgent need to effectively communicate and promote healthy dietary behaviors among individuals with a history of cancer. Researchers are using fitness trackers, smartphone applications, and other innovative approaches to inform and encourage cancer survivors about the long-term advantages of a healthy diet for an enhanced quality of life (571)Allicock M, Kendzor D, Sedory A, et al. A Pilot and Feasibility Mobile Health Intervention to Support Healthy Behaviors in African American Breast Cancer Survivors. J Racial Ethn Heal Disparities. 2021;8(1)..
The positive impact of maintaining healthy behaviors has prompted many health-related federal agencies and cancer-focused professional societies to offer comprehensive guidelines that help cancer survivors adopt a long-lasting healthy lifestyle (572)American Society of Clinical Oncology. Cancer.Net; healthy living. [cited 2021 Jul 10].(573)Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):243-274.(574)Centers for Disease Control and Prevention. Cancer survirors: guides to healthy living. [updated 2020 Dec 10; cited 2021 Jul 10].(575)National Comprehensive Cancer Network. NCCN guidelines for patients: survivorship care for healthy living, 2020..
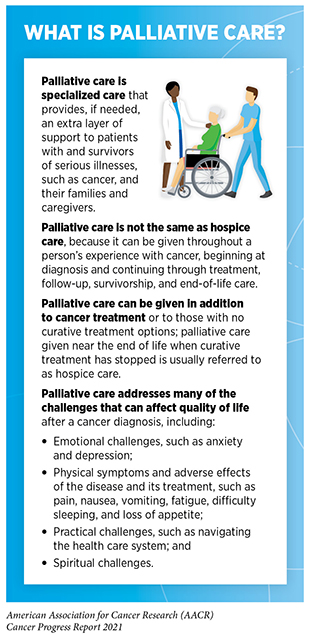
Palliative Care
Palliative care is a multidisciplinary approach to providing optimized quality of life for people with cancer, as well as their families and caregivers (see sidebar on What Is Palliative Care?). Palliative care aims to alleviate the adverse effects of cancer diagnosis and treatment and addresses the psychological, social, and spiritual challenges faced by cancer survivors. Individuals with cancer can receive palliative care throughout their experience with cancer, beginning at diagnosis and continuing through treatment, follow-up, survivorship, and end-of-life decisions.
Integration of palliative care during the early stage of a person’s cancer experience can significantly improve quality of life. Multiple studies have shown that palliative care leads to a better management of symptoms resulting from cancer and/or its treatment, decreases depression and anxiety, improves quality of life for both cancer survivors and their caregivers, and results in longer survival (576)Rocque GB, Cleary JF. Palliative care reduces morbidity and mortality in cancer. Nat Rev Clin Oncol. 2013;10(2).(577)Howie L, Peppercorn J. Early palliative care in cancer treatment: Rationale, evidence and clinical implications. Ther Adv Med Oncol. 2013;5(6).(578)Hausner D, Tricou C, Mathews J, et al. Timing of Palliative Care Referral Before and After Evidence from Trials Supporting Early Palliative Care. Oncologist. 2021;26(4).(579)Ferrell BR, Chung V, Koczywas M, Smith TJ. Dissemination and implementation of palliative care in oncology. J Clin Oncol. 2020;38(9).. Ongoing studies are further investigating different methods to help cancer survivors cope with various adverse effects of cancer diagnosis and treatment. In an ongoing clinical trial that included cancer survivors with chronic musculoskeletal pain, electroacupuncture—a form of acupuncture where a small electric current is passed between pairs of acupuncture needles—reduced the pain twice as much as usual care in the 12-week period spanning the treatment (580)Mao JJ, Liou KT, Baser RE, et al. Effectiveness of electroacupuncture or auricular acupuncture vs usual care for chronic musculoskeletal pain among cancer survivors the PEACE randomized clinical trial. JAMA Oncol. 2021;7(5).. Findings from another ongoing clinical trial showed that high-dose radiation therapy, called stereotactic body radiation therapy, or SBRT, was highly effective in relieving the pain experienced by some patients with painful spinal metastases from advanced cancer (581)Sahgal A, Myrehaug SD, Siva S, et al. CCTG SC.24/TROG 17.06: A Randomized Phase II/III Study Comparing 24Gy in 2 Stereotactic Body Radiotherapy (SBRT) Fractions Versus 20Gy in 5 Conventional Palliative Radiotherapy (CRT) Fractions for Patients with Painfu. About a third of cancer patients in the study who received radiation therapy for spinal metastases did not experience pain up to six months after treatment, compared to only about 15 percent of people who received conventional external beam radiation therapy to treat the pain (581)Sahgal A, Myrehaug SD, Siva S, et al. CCTG SC.24/TROG 17.06: A Randomized Phase II/III Study Comparing 24Gy in 2 Stereotactic Body Radiotherapy (SBRT) Fractions Versus 20Gy in 5 Conventional Palliative Radiotherapy (CRT) Fractions for Patients with Painfu. These findings are highlighting the importance of integrating palliative care throughout the continuum of clinical cancer care. As of 2018, 95 percent of the NCI-designated cancer centers had outpatient palliative care clinics. In contrast, only 40 percent of non-NCI-designated cancer centers had outpatient palliative care clinics (582)Hui D, De La Rosa A, Chen J, et al. State of palliative care services at US cancer centers: An updated national survey. Cancer. 2020;126(9).. NCI-designated cancer centers were also more likely that non-NCI-designated cancer centers to have fellowships in palliative care for medical trainees (87 vs 30 percent) and research programs focused on palliative care (58 vs 15 percent) (583)Hui D, De La Rosa A, Chen J, et al. Palliative care education and research at US cancer centers: A national survey. Cancer. 2021;127(12).. These findings highlight the opportunities to further improve palliative care programs that can effectively assist cancer survivors and caregivers at any stage during their experience with cancer (584)Mathews J, Zimmermann C. Palliative care services at cancer centres — room for improvement. Nat Rev Clin Oncol. 2020;17(6)..
In addition to the investments in institutional infrastructure for palliative care delivery, it is equally important to raise awareness of the numerous benefits of palliative care among cancer survivors and their caregivers. According to recent findings, 66 percent of cancer survivors had never heard of palliative care, and only 17 percent knew enough about palliative care to explain it to someone else (585)Stal J, Nelson MB, Mobley EM, et al. Palliative care among adult cancer survivors: Knowledge, attitudes, and correlates. Palliat Support Care. Published online 2021.. In a pilot study, knowledge of palliative care increased by 83 percent among cancer patients when they received a multimedia intervention providing knowledge and reassurance about the purpose and nature of palliative care. Researchers also found that patients’ perception of what palliative care was improved by nearly 19 points (586)Perry LM, Sartor O, Malhotra S, et al. Increasing Readiness for Early Integrated Palliative Oncology Care: Development and Initial Evaluation of the EMPOWER 2 Intervention. J Pain Symptom Manage. Published online 2021.. As researchers develop additional strategies to improve the uptake of palliative care, it would be vital to ensure equitable access to any such approaches for all patient populations.
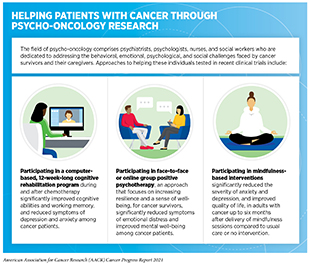
Psycho-oncology
Psycho-oncology is an interdisciplinary subspeciality within the cancer care continuum that aims to address the physical, behavioral, emotional, and psychosocial distress that arises for cancer survivors and their caregivers (587)Lang-Rollin I, Berberich G. Psycho-oncology. Dialogues Clin Neurosci 2018;20:13–22.. These challenges adversely affect treatment and management of cancer and, when not addressed in an effective and timely manner, can lead to long-term morbidity and premature mortality (see Challenges Faced by Cancer Survivors). Experts who are trained in psycho-oncology approaches apply a holistic approach to destigmatize and address behavioral and psychosocial distress that is often caused by cancer diagnosis and treatment (see sidebar on Helping Patients with Cancer Through Psycho-oncology Research). Mindfulness—the skill of bringing one’s attention to whatever is happening in the present moment in a thoughtful and nonjudgmental manner—is one approach by which psycho-oncology helps alleviate physical distress, while simultaneously focusing on mental well-being (588)Kingston T, Collie S, Hevey D, et al. Mindfulness-based cognitive therapy for psycho-oncology patients: An exploratory study. Ir J Psychol Med. 2015;32(3).. Ongoing research is focused on better understanding the impact of these approaches in improving quality of life for cancer survivors (589)Shaw JM, Sekelja N, Frasca D, Dhillon HM, Price MA. Being mindful of mindfulness interventions in cancer: A systematic review of intervention reporting and study methodology. Psychooncology. 2018;27(4).. Cancer survivors and their caregivers should discuss with health care providers whether psycho-oncology-based interventions will be beneficial to them.
Delivering Care to Cancer Survivors
Over the past five decades, the number of cancer survivors has steadily increased, thanks to advances in cancer etiology, prevention, screening, and treatment (see Figure 25). Furthermore, cancer survivors are living longer and fuller lives. These improvements highlight the need to develop a strong and equitable care system to support long-term survivorship.
Coordinating Care
Deteriorated overall health, increased financial burden, and reduced quality of life are only a few of the numerous challenges cancer survivors face compared to healthy individuals. The multifaceted impact of cancer diagnosis and treatment results in complex health care needs. These needs can only be met by a comprehensive and coordinated approach that ensures efficient and equitable delivery of care to all cancer survivors.
A well-coordinated care plan has the potential to deliver maximum benefit to patients by decreasing their risk of long-term morbidity and premature mortality and by improving their quality of life. Optimal coordinated care recognizes that cancer is a complex disease which requires multiple appointments with health care providers and rounds of treatments, as well as support and follow-up care in multiple aspects of life from specially trained health care providers (593)Weaver SJ, Jacobsen PB. Cancer care coordination: Opportunities for healthcare delivery research. Transl Behav Med. 2018;8(3).. Eighty-six percent of participants in a webinar on the needs for a well-developed coordinated care plan emphasized the importance of identifying key outcomes and measures—tailored for the unique and different needs of different cancer survivors—as well as using digital health approaches to implement and assess quality care coordination (594)Gallicchio L, Tonorezos E, de Moor JS, et al. Evidence Gaps in Cancer Survivorship Care: A Report from the 2019 National Cancer Institute Cancer Survivorship Workshop. JNCI J Natl Cancer Inst. Published online 2021..
Researchers are also investigating how innovative digital health strategies such as telehealth can help cancer survivors relieve adverse effects of their cancer experience. Telehealth, also called telemedicine, is the distribution of health-related services and information using telecommunication technologies, such as the internet and smartphone applications (407)Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract. 2021;17(2).. A recent study found that telehealth-based interventions significantly improved quality of life among cancer survivors when compared to usual care (595)Larson JL, Rosen AB, Wilson FA. The effect of telehealth interventions on quality of life of cancer survivors: A systematic review and meta-analysis. Health Informatics J. 2020;26(2).. The COVID-19 pandemic has further uncovered the potential of telehealth in providing care for cancer survivors. A recent survey found that 95 percent of childhood cancer survivors, whose long-term in-person follow-ups had to be conducted virtually by videoconference during the peaks of the COVID-19 pandemic from April to June 2020, expressed complete or high satisfaction with the experience. Importantly, 66 percent of the survivors considered virtual visits as helpful or nearly as helpful as in-person visits, and 82 percent preferred that these visits remain an option after the pandemic (596)Kenney LB, Vrooman LM, Lind ED, et al. Virtual visits as long-term follow-up care for childhood cancer survivors: Patient and provider satisfaction during the COVID-19 pandemic. Pediatr Blood Cancer. 2021;68(6)..
Frequent communication between cancer patients and their care team is central to making shared health care-related decisions. According to a recent analysis of web-based surveys of clinicians and patients, 98 percent of patients and 70 percent of clinicians found that electronic access to records that included notes from clinic visits and information on diagnosis and treatment was valuable for developing and coordinating an effective care plan (597)Salmi L, Dong ZJ, Yuh B, Walker J, DesRoches CM. Open Notes in Oncology: Patient versus Oncology Clinician Views. Cancer Cell. 2020;38(6).. Information gleaned from such studies provides the basis to develop evidence-based approaches to coordinated care that increases the well-being of cancer survivors throughout their experience with cancer.
The Important Role of Caregivers
Caregivers play a central role in any coordinated care team for a cancer survivor from the time of diagnosis through the entire cancer experience. As the number of cancer survivors increases, the number of trained caregivers (for example, health care professionals) as well as informal caregivers (for example, spouses) is also on the rise. Nearly three million Americans care for an individual who has been diagnosed with cancer (597)Salmi L, Dong ZJ, Yuh B, Walker J, DesRoches CM. Open Notes in Oncology: Patient versus Oncology Clinician Views. Cancer Cell. 2020;38(6)., and the majority are informal caregivers. According to a recent study, more than 55 percent of cancer survivors reported having an informal caregiver during or after their cancer treatment (599)Borsky AE, Zuvekas SH, Kent EE, de Moor JS, Ngo-Metzger Q, Soni A. Understanding the characteristics of US cancer survivors with informal caregivers. Cancer. Published online 2021..
As the health care needs of cancer survivors range widely depending on many factors such as the age at which a person was diagnosed with cancer and the type of treatment received, both trained and informal caregivers face mental and emotional challenges when taking care of a cancer survivor (600)Given BA, Given CW, Sherwood PR. Family and Caregiver Needs over the Course of the Cancer Trajectory. J Support Oncol. 2012;10(2).. However, adverse effects of cancer are felt at a deeper level by informal caregivers, who often struggle with the dual burden of providing complex clinical care and managing personal emotional distress (601)Harrison R, Raman M, Walpola RL, Chauhan A, Sansom-Daly UM. Preparing for partnerships in cancer care: an explorative analysis of the role of family-based caregivers. BMC Heal Serv Res 2021 211. 2021;21(1):1-10.. The COVID-19 pandemic has further added to the stress associated with caring for cancer survivors. According to one study, 60 to 70 percent of parents who were caring for an AYA with brain tumor during the pandemic reported worsened mood and increased anxiety during this time (602)Fisher AP, Patronick J, Gerhardt CA, Radonovich K, Salloum R, Wade SL. Impact of COVID-19 on adolescent and emerging adult brain tumor survivors and their parents. Pediatr Blood Cancer. Published online 2021.. Researchers are investigating ways to develop approaches that can help cancer caregivers cope with the stress of caring for an individual with cancer. As one example, researchers have found that family caregivers who received emotion regulation therapy, an evidence-based approach to counter distress (603)Renna ME, Quintero JM, Fresco DM, Mennin DS. Emotion regulation therapy: A mechanism-targeted treatment for disorders of distress. Front Psychol. 2017;8(FEB).), reported significant reductions in psychological distress and worries (604)O’Toole MS, Mennin DS, Applebaum A, et al. A randomized controlled trial of emotion regulation therapy for psychologically distressed caregivers of cancer patients. JNCI Cancer Spectr. 2020;4(1).. Increased focus on and awareness of the unmet needs of cancer caregivers underscore the potential of a well-developed in-home care system—that includes caring for the well-being of caregivers—for improving clinical outcomes and quality of life for cancer survivors.