Preventing Cancer: Identifying Risk Factors
In this section you will learn:
- In the United States, four out of 10 cancer cases are associated with preventable risk factors.
- Not using tobacco is one of the most effective ways a person can prevent cancer from developing.
- Nearly 20 percent of U.S. cancer diagnoses are related to excess body weight, alcohol intake, poor diet, and physical inactivity.
- Many cases of skin cancer could be prevented by protecting the skin from ultraviolet radiation from the sun and indoor tanning devices.
- Nearly all cases of cervical cancer, as well as many cases of head and neck and anal cancers, could be prevented by HPV vaccination, but more than 41 percent of U.S. adolescents have not yet received the recommended doses of the vaccine.
- The mechanisms by which certain risk factors such as obesity, unhealthy diet, and physical inactivity increase cancer incidence are currently under investigation.
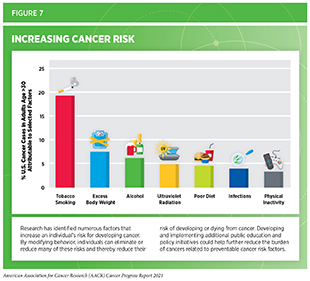
Factors that increase a person’s chances of developing cancer are referred to as cancer risk factors. Decades of research have led to the identification of numerous cancer risk factors (see Figure 7) such as tobacco use, poor diet, physical inactivity, obesity, infection with certain pathogens, and exposure to ultraviolet (UV) radiation. Given that several of these risks can be avoided, many cases of cancer could potentially be prevented. In fact, according to a recent report, healthy lifestyle habits can reduce risks even among those with a higher genetic risk for cancer (see sidebar on How Do I Know If I Am at High Risk for Developing an Inherited Cancer?)(180)Zhu M, Wang T, Huang Y, et al. Genetic Risk for Overall Cancer and the Benefit of Adherence to a Healthy Lifestyle. Cancer Res. Published online 2021.. In the United States, more than 40 percent of all new cancer cases diagnosed in 2014, which are the most recent data available, were attributable to preventable risk factors (181)Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. 2018;68(1):31-54.. Emerging data indicate that certain cancer risk factors are also associated with worse outcomes after a cancer diagnosis including development of secondary cancers (182)Sung H, Hyun N, Leach CR, Yabroff KR, Jemal A. Association of first primary cancer with risk of subsequent primary cancer among survivors of adult-onset cancers in the United States. JAMA – J Am Med Assoc. 2020;324(24).(183)Petrelli F, Cortellini A, Indini A, et al. Association of Obesity With Survival Outcomes in Patients With Cancer. JAMA Netw Open. 2021;4(3)..
Many cancer risk factors also contribute to other chronic diseases, such as cardiovascular disease, respiratory diseases, and diabetes. Therefore, reducing or eliminating exposure through lifestyle changes, behavior modifications, public education, and policy implementation has the potential to reduce the burden of cancer as well as several other diseases.
In the United States, many of the greatest reductions in cancer morbidity and mortality have been achieved through the implementation of effective public education and policy initiatives. For example, such initiatives have helped reduce cigarette smoking rates among U.S. adults by 67 percent from 1965 to 2019 (23)Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep. Published online 2020.. These reductions have contributed significantly to the dramatic decline in overall U.S. cancer mortality rates (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. However, cigarette smoking still accounted for nearly four out of 10 cancer deaths in parts of the United States between 2013 and 2017 (185)Islami F, Bandi P, Sahar L, Ma J, Drope J, Jemal A. Cancer deaths attributable to cigarette smoking in 152 U.S. metropolitan or micropolitan statistical areas, 2013–2017. Cancer Causes Control. 2021;(0123456789):2013-2017.. It is also concerning that the prevalence of certain cancer risk factors, such as obesity has been rising steadily among U.S. adults (186)Trust for America’s Health. The state of obesity 2020: better policies for a healthier America. Robert Wood Johnson Foundation. 2020 Sept.(187)Sung H, Siegel RL, Rosenberg PS, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Heal. 2019;4(3):e137-e147.(188)Koroukian SM, Dong W, Berger NA. Changes in Age Distribution of Obesity-Associated Cancers. JAMA Netw Open. 2019;2(8):e199261-e199261.. Consequently, progress in terms of mortality reduction has slowed down for obesity-related cancers compared to cancers not associated with obesity (189)Avery CL, Howard AG, Nichols HB. Comparison of 20-Year Obesity-Associated Cancer Mortality Trends with Heart Disease Mortality Trends in the US. JAMA Netw Open. Published online 2021.. There are, however, significant disparities in the burden of cancer risk factors among certain segments of the U.S. population such as racial and ethnic minorities and individuals from low socioeconomic status (see sidebar on Disparities in the Prevalence of Preventable Cancer Risk Factors). Therefore, it is imperative that all stakeholders come together to identify better strategies for the dissemination of our current knowledge of cancer prevention and implementation of effective evidence-based practices that promote a healthier lifestyle among all populations.
Eliminate Tobacco Use
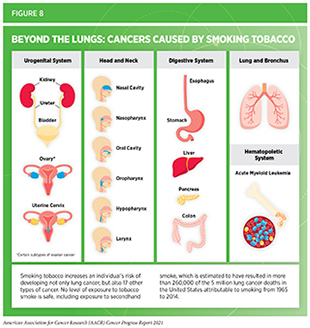
Use of tobacco is the leading cause of preventable disease, disability, and death in the United States, taking more than 480,000 lives each year (196)American Lung Association. State of tobacco control 2021. [cited 2021 Jul 10].. Smoking tobacco has been shown to increase the risk of developing 17 different types of cancer in addition to lung cancer (see Figure 8). Smokers are exposed to numerous harmful chemicals that damage DNA, causing genetic and epigenetic alterations that lead to cancer development (197)Centers for Disease Control and Prevention. Cancer and tobacco use. CDC Vital Signs, November 2016.(198)M V, SY H, I K, et al. Chronic Cigarette Smoke-Induced Epigenomic Changes Precede Sensitization of Bronchial Epithelial Cells to Single-Step Transformation by KRAS Mutations. Cancer Cell. 2017;32(3):360-376.e6.(199)TM B, H K, R T, et al. Smoking is associated with hypermethylation of the APC 1A promoter in colorectal cancer: the ColoCare Study. J Pathol. 2017;243(3):366-375.. Fortunately, quitting tobacco at any age can reduce risks from cancer as well as several other smoking-related adverse health effects, such as cardiovascular and pulmonary diseases (200)United States Public Health Services Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General. Washington (DC); US Department o.
Thanks to the implementation of nationwide comprehensive tobacco control initiatives, cigarette smoking among U.S. adults has been declining steadily (201)U.S. Department of Health and Human Services. The health consequences of smoking – 50 years of progress: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.. In 2019, which is the most recent year for which such data are available, 14 percent of U.S. adults ages 18 and older smoked cigarettes, a significant decline from 42.4 percent of adults in 1965 (23)Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep. Published online 2020.(201)U.S. Department of Health and Human Services. The health consequences of smoking – 50 years of progress: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.. Cigarette use has also declined among U.S. youth, especially over the past decade (21)Meza R, Jimenez-Mendoza E, Levy DT. Trends in Tobacco Use Among Adolescents by Grade, Sex, and Race, 1991-2019. JAMA Netw open. 2020;3(12):e2027465.. However, nearly 51 million adults and 4.5 million middle and high school students in the United States were still using some type of tobacco product in 2019 and 2020, respectively (23)Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco Product Use Among Adults — United States, 2019. MMWR Morb Mortal Wkly Rep. Published online 2020.(202)Gentzke AS. Tobacco Product Use Among Middle and High School Students — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881-1888.. It has been documented that most adult users initiate smoking in their youth. Recent studies corroborate these findings further showing that among youth who were previously nonsusceptible to cigarette use, many initiate smoking between ages 16 and 18 years although the age at initiation varies by sex and race or ethnicity (203)Pérez A, N’Hpang RS, Callahan E, et al. Age at Initiation of Cigarette Use in a Nationally Representative Sample of US Youth, 2013-2017. JAMA Netw Open. 2021;4(2).. Recent data also suggest that the age of smoking onset may be shifting upward from youth to young adulthood. According to a new report, the proportion of smokers who initiated smoking in their early adulthood, between ages 18 and 23 years, more than doubled between 2002 and 2018 (204)Barrington-Trimis JL, Braymiller JL, Unger JB, et al. Trends in the Age of Cigarette Smoking Initiation Among Young Adults in the US From 2002 to 2018. JAMA Netw open. 2020;3(10).. Collectively, these data reinforce the fact that smoking prevention efforts targeting youth and young adults are vital and may have significant, long-term positive impact on smoking-related health outcomes.
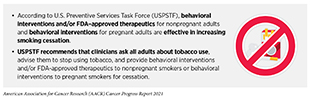
It is imperative that researchers, public health experts, and policy makers work together to identify evidence-based, population-level interventions such as tobacco price increases, public health campaigns, age and marketing restrictions, cessation counseling and medications, and smoke-free laws to further reduce smoking rates and smoking-related cancer burden in the United States. Effective interventions should also help drive down secondhand smoke exposure which is a risk factor for lung cancer among adult nonsmokers. Recent reports indicate that innovative interventions such as smoking cessation advice along with free samples of nicotine replacement therapy offered to expectant fathers or a smartphone application-based therapy offered to parents while they are visiting the office of their child’s pediatrician can increase smoking cessation (206)Drouin O, Sato R, Drehmer JE, et al. Cost-effectiveness of a Smoking Cessation Intervention for Parents in Pediatric Primary Care. JAMA Netw Open. 2021;4(4).(207)Luk TT, Lam TH, Leung WC, et al. Brief Advice, Nicotine Replacement Therapy Sampling, and Active Referral for Expectant Fathers Who Smoke Cigarettes: A Randomized Clinical Trial. JAMA Intern Med. Published online 2021.(208)E N-B, JE D, B HW, et al. Treating Parents for Tobacco Use in the Pediatric Setting: The Clinical Effort Against Secondhand Smoke Exposure Cluster Randomized Clinical Trial. JAMA Pediatr. 2019;173(10):931-939.. Ongoing research in this area is essential since over half of adult smokers try to quit smoking each year but fewer than 10 percent are successful (200)United States Public Health Services Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General. Washington (DC); US Department o. Notably, FDA-approved therapeutics and behavioral counseling have both been shown to improve the chances of quitting smoking and using them together can double the odds of quitting successfully (200)United States Public Health Services Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General. Washington (DC); US Department o.
The use of other combustible tobacco products (for example, cigars), smokeless tobacco products (for example, chewing tobacco and snuff), and waterpipes (hookahs) is also associated with adverse health outcomes including cancer (211)CH C, B R, C C, et al. Association of Cigarette, Cigar, and Pipe Use With Mortality Risk in the US Population. JAMA Intern Med. 2018;178(4):469-476.. Electronic cigarettes (e-cigarettes) have gained enormous popularity among U.S. youth and young adults over the past decade (see sidebar on E-Cigarettes: What Have We Learned and What Do We Need to Know?). E-cigarettes, first introduced to the U.S. market in 2007, have been the most used tobacco product among U.S. middle and high school students since 2014 (202)Gentzke AS. Tobacco Product Use Among Middle and High School Students — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1881-1888.(212)Surgeon General’s Advisory on E-cigarette Use Among Youth The E-cigarette Epidemic Among Youth.. Since their introduction to the U.S. marketplace, the landscape of e-cigarettes has evolved to include different types of products such as prefilled pods (cartridge–based devices) and disposable (single use) devices, among others. E-cigarettes come in flavors that appeal to youth, and these flavors are key drivers of use among youth and young adults. E-cigarettes deliver very high levels of nicotine, an extremely addictive substance, that is harmful to the developing brain (213)U.S. Department of Health and Human Services. E-cigarette use among youth and young adults. A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2016., and are known to contain high levels of other toxic chemicals including reactive aldehydes (214)Public Health Consequences of E-Cigarettes. Public Heal Consequences E-Cigarettes. Published online 2018..
The surge in the use of e-cigarettes between 2011 and 2019 among youth and young adults, populations especially vulnerable to the detrimental effects of nicotine, raised great concern among U.S. public health officials. In December 2018, the Office of the U.S. Surgeon General issued an advisory declaring e-cigarette use in youth an epidemic, and since then FDA, the federal government, and many local governments have proposed several restrictions on e-cigarettes including bans on certain flavors to curb youth appeal (see Reducing Tobacco-related Illness Through Public Health Policy). Therefore, it is encouraging that the use of e-cigarettes declined among U.S. youth and young adults between 2019 and 2020. However, 3.6 million youth and young adults still reported using e-cigarettes in 2020 (216)Gentzke AS, Wang TW, Neff LJ, et al. E-cigarette Use Among Middle and High School Students — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1310-1312.. Clearly, more work needs to be done to effectively curb the use of these products. Beyond the United States, e-cigarettes are emerging as a serious public health threat globally, necessitating the WHO to call for better regulation of these products in its latest report on the global tobacco epidemic (230)World Health Organization. WHO report on the global tobacco epidemic 2021: addressing new and emerging products. 2021 Jul 27..
It is known that more than 80 percent of e-cigarette users prefer flavored products. In February 2020, FDA implemented certain restrictions on flavoring in pod/cartridge-based e-cigarettes (see Reducing Tobacco-related Illness Through Public Health Policy). While these are welcome changes, one outstanding concern is that disposable products were exempted from any flavor restrictions, leaving many youth-friendly flavors on the market. Notably, there has been a striking surge in the use of disposable products among middle (400 percent) and high school (1000 percent) students between 2019 and 2020 (216)Gentzke AS, Wang TW, Neff LJ, et al. E-cigarette Use Among Middle and High School Students — United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1310-1312.. Recent data also suggest that many youth and young adults were able to access e-cigarettes from online stores (instead of regular retail shops) during the COVID-19 pandemic, emphasizing the need for strict enforcement of policies such as age verification to limit youth access (231)Gaiha SM, Lempert LK, Halpern-Felsher B. Underage Youth and Young Adult e-Cigarette Use and Access Before and During the Coronavirus Disease 2019 Pandemic. JAMA Netw open. 2020;3(12):e2027572.[/tooltip.
Interestingly, based on a new survey that polled 498 e-cigarette users between ages 12 and 17 years, nearly half of the participants expressed interest in quitting, highlighting the vital need for evidence-based e-cigarette cessation interventions [tooltip text="232" url="https://doi.org/10.1001/jamapediatrics.2020.2348" newwindow="true"]Smith TT, Nahhas GJ, Carpenter MJ, et al. Intention to Quit Vaping among United States Adolescents. JAMA Pediatr. 2021;175(1).. In this regard, a recent clinical trial conducted among e-cigarette users between ages 18 and 24 showed that a text message-based cessation intervention that delivered social support and cognitive and behavioral coping skills to the participants was effective at helping more than 24 percent of participants abstain from e-cigarettes for up to seven months of follow-up (233)Graham AL, Amato MS, Cha S, Jacobs MA, Bottcher MM, Papandonatos GD. Effectiveness of a Vaping Cessation Text Message Program among Young Adult e-Cigarette Users: A Randomized Clinical Trial. JAMA Intern Med. Published online 2021.. Whether similar interventions have the potential to be effective among younger users remains to be assessed.
While the prevalence of e-cigarette use in U.S. adults is lower than that in youth and young adults, it must be noted that nearly 80 percent of adult e-cigarette users are either current or former smokers, and most users report using or having used e-cigarettes to quit smoking (235)Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic Characteristics, Cigarette Smoking, and e-Cigarette Use Among US Adults. JAMA Netw open. 2020;3(10). even though there is no clear evidence that e-cigarettes are effective as a smoking cessation tool. There is, however, data that former smokers who use e-cigarettes are more likely to experience a smoking relapse (236)Everard CD, Silveira ML, Kimmel HL, Marshall D, Blanco C, Compton WM. Association of Electronic Nicotine Delivery System Use with Cigarette Smoking Relapse among Former Smokers in the United States. JAMA Netw Open. 2020;3(6).. In addition, there are accumulating data on the adverse health outcomes of e-cigarette use. For instance, according to a new study from a nationally representative cohort of U.S. adults, e-cigarette use was shown to be associated with a significantly increased risk of major respiratory diseases, such as COPD, emphysema, and asthma independent of the use of cigarettes or other types of tobacco products (226)Xie W, Kathuria H, Galiatsatos P, et al. Association of Electronic Cigarette Use with Incident Respiratory Conditions among US Adults from 2013 to 2018. JAMA Netw Open. 2020;3(11).. Clearly, the significant harm to public health outweighs the currently unclear role in smoking cessation among adult smokers. It is imperative that public health professionals continue to evaluate the long-term health outcomes associated with e-cigarette use and gather definitive evidence on their role in smoking cessation.
Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active
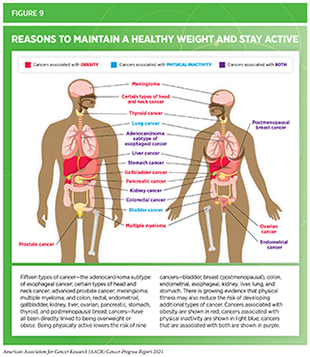
Nearly 20 percent of new cancer cases and 16 percent of cancer deaths in U.S. adults are attributable to a combination of excess body weight, poor diet, physical inactivity, and alcohol consumption (181)Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. 2018;68(1):31-54.. Being overweight or obese as an adult increases a person’s risk for 15 types of cancer; being physically active reduces risk for nine types of cancer (see Figure 9). Therefore, maintaining a healthy weight, being physically active, and consuming a balanced diet are effective ways a person can lower the risk of developing or dying from cancer (see sidebar on Reduce Your Risk for Cancer by Maintaining a Healthy Weight, Being Physically Active, and Consuming a Balanced Diet). Identifying the underlying mechanisms by which obesity, unhealthy diet, and physical inactivity increase cancer risk and quantifying the magnitude of such risks are areas of active research.
The prevalence of obesity has been rising steadily in the United States. In 2018, which is the most recent year for which data are available, 21 percent of youth ages 12 to 19, and 42 percent of adults age 20 and older were considered obese (186)The State of Obesity 2020: Better Policies for a Healthier America.(244)Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and hispanic origin – 1999-2000 to 2017-2018. JAMA – J Am Med Assoc. 2020;324(12).. There are, however, stark disparities based on levels of income as well as race/ethnicity (186)The State of Obesity 2020: Better Policies for a Healthier America.. It is also concerning that 40 percent of U.S. adults who are overweight and nearly 10 percent of adults who are obese do not consider themselves to be overweight (245)Kwak YE, McMillan R, McDonald EK. Trends in Overweight and Obesity Self-awareness Among Adults With Overweight or Obesity in the United States, 1999 to 2016. Ann Intern Med. 2021;174(5).. Notably, among individuals who are obese, awareness of their obesity status is associated with a 2.5-fold increase in their attempts to lose weight (245)Kwak YE, McMillan R, McDonald EK. Trends in Overweight and Obesity Self-awareness Among Adults With Overweight or Obesity in the United States, 1999 to 2016. Ann Intern Med. 2021;174(5).. Collectively, these data highlight the need for public education to raise awareness about the adverse health outcomes of excess body weight, as well as the importance of evidence-based interventions to help maintain a healthy weight. In this regard, a recent clinical trial conducted at several primary care clinics serving racially diverse low-income populations across Louisiana showed that a diet, exercise, and health coaching-based intervention resulted in significantly higher weight loss over 24 months when compared to routine primary care (246)Katzmarzyk PT, Martin CK, Newton RL, et al. Weight Loss in Underserved Patients — A Cluster-Randomized Trial. N Engl J Med. 2020;383(10)..
Over the past three decades the United States has witnessed unprecedented progress against cancer as is evident by a steady decline in overall cancer mortality rates. Unfortunately, the rising obesity trends threaten to slow down this progress against cancer. In fact, recent data show that while the decline in mortality rates over the past two decades accelerated for cancers not associated with obesity, mortality improvements have decelerated for obesity-associated cancers (189)Avery CL, Howard AG, Nichols HB. Comparison of 20-Year Obesity-Associated Cancer Mortality Trends with Heart Disease Mortality Trends in the US. JAMA Netw Open. Published online 2021.. Beyond cancer, obesity increases the risk of developing and dying from several other health problems including type 2 diabetes, high blood pressure, stroke, and heart, liver, and kidney disease. Most recently, obesity has been shown to be associated with worse outcomes from COVID-19 (247)Centers for Disease Control and Prevention. COVID-19: people with certain medical conditions. [updated 2021 May 13; cited 2021 Jul 11].. Encouragingly, according to a recent report, weight loss between early adulthood and midlife among individuals who were obese during their early adulthood is associated with a greater than 50 percent reduction in the subsequent risk of early death (248)Xie W, Lundberg DJ, Collins JM, et al. Association of Weight Loss between Early Adulthood and Midlife with All-Cause Mortality Risk in the US. JAMA Netw Open. 2020;3(8).. There are also emerging data showing that weight loss intervention through bariatric surgery may lower the future risk of certain obesity-related cancers (249)Tao W, Santoni G, von Euler-Chelpin M, et al. Cancer Risk After Bariatric Surgery in a Cohort Study from the Five Nordic Countries. Obes Surg. 2020;30(10).(250)Schauer DP, Feigelson HS, Koebnick C, et al. Bariatric Surgery and the Risk of Cancer in a Large Multisite Cohort. Ann Surg. 2019;269(1).(251)DocWire News. Weight loss surgery cuts risk of pancreatic cancer for obese patients with type 2 diabetes. 2020 Oct 14. [cited 2021 Jul 10]. .While further research is needed to elucidate whether weight loss can effectively mitigate risks of developing and/or dying from all obesity-related cancers, evidence-based population-level interventions to address obesity must certainly be a top priority among U.S. public health efforts.
Complex and interrelated factors ranging from socioeconomic, environmental, and biological to individual lifestyle factors contribute to obesity. There is, however, sufficient evidence that consumption of high-calorie, energy-dense foods and beverages and lack of physical activity play a significant role (186)The State of Obesity 2020: Better Policies for a Healthier America.. To achieve and maintain good health, U.S. Department of Agriculture (USDA) and U.S. Department of Health and Human Services, in Dietary Guidelines for Americans, 2020-2025, recommend that individuals follow a healthy dietary pattern at every stage of life (253)U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary guidelines for Americans: 2020-2025. 9th edition; December 2020.. According to the guidelines, all individuals should fulfill their nutritional needs by consuming nutrient-dense food and beverages including fruits, vegetables, whole grains, low-fat dairy products, lean meat, eggs, seafood, beans, legumes, nuts, and vegetable oil, and limit foods and beverages that are high in added sugars, saturated fat, and sodium, as well as alcoholic beverages (253)U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary guidelines for Americans: 2020-2025. 9th edition; December 2020..
In the United States, more than 5 percent of all newly diagnosed cancer cases among adults are attributable to eating a poor diet (254)Zhang FF, Cudhea F, Shan Z, Michaud DS, Imamura F, Eom H, et al. Preventable cancer burden associated with poor diet in the United States. JNCI Cancer Spectr 2019;3:pkz034. and there is increasing evidence linking diet to cancer incidence and outcomes. For instance, a recent analysis showed that daily intake of five servings of fruit and vegetables was associated with a 10 percent reduction of overall cancer mortality when compared to intake of two servings per day (255)Wang DD, Li Y, Bhupathiraju SN, et al. Fruit and Vegetable Intake and Mortality: Results from 2 Prospective Cohort Studies of US Men and Women and a Meta-Analysis of 26 Cohort Studies. Circulation. Published online 2021.. There is also convincing evidence that higher intake of red meat is associated with increased risk, whereas higher intake of dietary fiber is associated with reduced risk of colorectal cancer incidence (256)Veettil SK, Tse ;, Wong Y, et al. Role of Diet in Colorectal Cancer Incidence Umbrella Review of Meta-analyses of Prospective Observational Studies Key Points + Supplemental content. JAMA Netw Open. 2021;4(2):2037341.(257)Gurjao C, Zhong R, Haruki K, et al. Discovery and features of an alkylating signature in colorectal cancer. Cancer Discov. Published online 2021.. Therefore, it is concerning that only seven percent of high school students met their fruit intake recommendations and only two percent of high school students met their vegetable intake recommendations in 2017; only 26 percent of adults met their fruit intake recommendations and 12 percent of adults met their vegetable intake recommendations in 2019 (193)Bandi P, Minihan AK, Siegel RL, et al. Updated Review of Major Cancer Risk Factors and Screening Test Use in the United States in 2018 and 2019, with a Focus on Smoking Cessation. Cancer Epidemiol Biomarkers Prev. Published online 2021.(258)Lange SJ, Moore LV, Harris DM, Merlo CL, Lee SH, Demissie Z, et al. Percentage of Adolescents Meeting Federal Fruit and Vegetable Intake Recommendations — Youth Risk Behavior Surveillance System, United States, 2017. MMWR Morb Mortal Wkly Rep 2021;70:69–74.. Furthermore, individuals who are overweight or obese are even less likely to follow recommended guidelines on dietary intake (259)Good M, Braun AC, Taylor CA, Spees CK. US Adults Fall Short of the Dietary Guidelines for Cancer Prevention Regardless of BMI Category. J Acad Nutr Diet. Published online 2021.. Intensive efforts by all stakeholders are needed if we are to increase the number of people who consume a balanced diet such as that recommended by the Dietary Guidelines for Americans, 2020-2025.
One of the major barriers to a healthy diet is “food insecurity,” which is defined by the USDA as the lack of access by all people in a household at all times to enough food for an active, healthy life. Many studies have found an association between food insecurity and excess body weight (186)The State of Obesity 2020: Better Policies for a Healthier America.. It is therefore extremely concerning that the prevalence of food insecurity increased from approximately nine percent to 18 percent between 2000 and 2016, and that racial and ethnic minorities and individuals living in poverty have significantly higher odds of living with food insecurity (260)Myers CA, Mire EF, Katzmarzyk PT. Trends in Adiposity and Food Insecurity among US Adults. JAMA Netw Open. 2020;3(8).. The COVID-19 pandemic has exacerbated these challenges with indications that point to an increased level of food insecurity in 2020 compared to the previous year (186)The State of Obesity 2020: Better Policies for a Healthier America.. It is imperative that all sectors work together to identify evidence-based public policies and programs that can eliminate food insecurity and ensure sustained availability of healthy food options for all Americans.
Evidence-based public policies implemented by state and federal governments play an important role in promoting healthy dietary habits. FDA, for example, recently began requiring food manufacturers to display updated nutrition labels on their product packaging. These labels must include information on added sugars and display calories and serving sizes in bolder and larger type (261)U.S. Food & Drug Adminstration. What’s new with the nutrition facts label. [updated 2020 Mar 11; cited 2021 Jul 10].. Another public policy aimed at reducing obesity is the introduction of taxes on sugar-sweetened beverages (SSBs) in several local jurisdictions in the United States (262)American Cancer Society. Cancer prevention & early detection: facts & figures 2021-2022. Atlanta: American Cancer Society: 2021.. SSBs are a major contributor to caloric intake among U.S. youth and adults, and there are some emerging data indicating that consumption of SSBs may be associated with an increased risk of cancer incidence and mortality (263)Koyratty N, McCann SE, Millen AE, Nie J, Trevisan M, Freudenheim JL. Sugar-sweetened soda consumption and total and breast cancer mortality: The western new york exposures and breast cancer (WEB) study. Cancer Epidemiol Biomarkers Prev. 2021;30(5).(264)Hur J, Otegbeye E, Joh HK, et al. Sugar-sweetened beverage intake in adulthood and adolescence and risk of early-onset colorectal cancer among women. Gut. Published online 2021.(265)Chazelas E, Srour B, Desmetz E, et al. Sugary drink consumption and risk of cancer: Results from NutriNet-Santé prospective cohort. BMJ. 2019;366.(266)Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened Beverage Consumption Among U.S. Youth, 2011-2014. NCHS Data Brief. 2017;(271):1-8.(267)Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened Beverage Consumption Among U.S. Adults, 2011-2014. NCHS Data Brief. 2017;(270):1-8.(268)Joh HK, Lee DH, Hur J, et al. Simple Sugar and Sugar-Sweetened Beverage Intake During Adolescence and Risk of Colorectal Cancer Precursors. Gastroenterology. 2021;161(1).. Thus, it is encouraging that the prevalence of heavy SSB intake (consumption of more than 500 kcal from SSBs per day) has declined among U.S. children and adults in recent years (269)Vercammen KA, Moran AJ, Soto MJ, Kennedy-Shaffer L, Bleich SN. Decreasing Trends in Heavy Sugar-Sweetened Beverage Consumption in the United States, 2003 to 2016. J Acad Nutr Diet. 2020;120(12).[/tooltip. Interestingly, researchers estimate that both policies—nutrition facts/added-sugar labeling and SSB taxes—can be cost effective and can potentially result in significant health gains as well as economic benefits for all populations including those who experience cancer health disparities [tooltip text="270" url="https://doi.org/10.1093/JNCICS/PKAA073" newwindow="true"]Du M, Griecci CF, Kim DD, et al. Cost-effectiveness of a national sugar-sweetened beverage tax to reduce cancer burdens and disparities in the united states. JNCI Cancer Spectr. 2021;4(6).(271)Du M, Griecci CF, Cudhea FF, et al. Cost-effectiveness Analysis of Nutrition Facts Added-Sugar Labeling and Obesity-Associated Cancer Rates in the US. JAMA Netw Open. Published online 2021.. Continued research is necessary to identify effective policies related to food and nutrition that maximize health benefits and to evaluate the long-term effects of these policies on obesity and obesity-related health outcomes such as cancer.
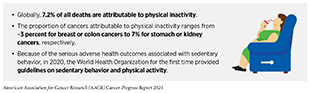
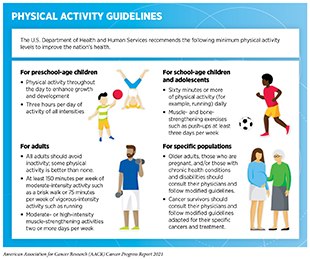
Three percent of overall cancer cases in the United States can be attributed to physical inactivity (181)Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. 2018;68(1):31-54.. According to a recent report, being sedentary (inactive) for 13 or more hours per day can increase the risk of dying from cancer by 52 percent while replacing 30 minutes of sedentary time with 30 minutes of moderate to high intensity physical activity can lower risk of cancer death by 30 percent (272)SC G, VJ H, T A, et al. Association of Sedentary Behavior With Cancer Mortality in Middle-aged and Older US Adults. JAMA Oncol. 2020;6(8):1210-1217.. Engaging in recommended amounts of physical activity (see sidebar on Physical Activity Guidelines) can lower the risks for developing nine types of cancer (Figure 9), and there is emerging evidence that there may be risk reduction for even more cancer types (238)CE M, SC M, H A, et al. Amount and Intensity of Leisure-Time Physical Activity and Lower Cancer Risk. J Clin Oncol. 2020;38(7):686-698.(239)AV P, CM F, SC M, et al. American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Med Sci Sports Exerc. 2019;51(11):2391-2402.(240)Moore SC, Lee I-M, Weiderpass E, et al. Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern Med. 2016;176(6):816-825.. Considering this evidence, it is concerning that more than a quarter of U.S. adults reported no leisure time physical activity in 2018, and about 17 percent of U.S. high school students reported no physical activity in 2019 (262)American Cancer Society. Cancer prevention & early detection: facts & figures 2021-2022. Atlanta: American Cancer Society: 2021.(273)American Cancer Society. Cancer prevention & early detection facts & figures 2019-2020. Atlanta: American Cancer Society; 2019.. There are added concerns that the COVID-19 pandemic may have led to further decreases in physical activity and increases in sedentary behavior across several population groups (274)Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc Med. 2021;7(1).. It is imperative that health care professionals and policy makers work together to increase awareness of the benefits of physical activity and support efforts to implement programs and policies to facilitate a physically active lifestyle for everyone.
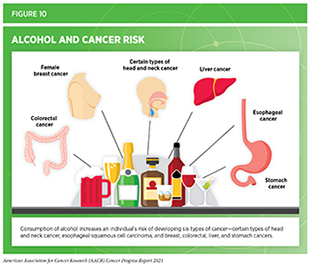
Limit Alcohol Consumption
Drinking alcohol increases the risk for six different types of cancer (241)World Cancer Research Fund/American Institute for Cancer Research. Diet and Cancer Report. Continuous Update Project. Expert Report. Diet, nutrition, physical activity and cancer: a global perspective.(see Figure 10) while emerging evidence suggests that there may be risks for additional cancer types (277)Papadimitriou N, Markozannes G, Kanellopoulou A, et al. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat Commun. 2021;12(1).. Even modest use of alcohol may increase cancer risk, but the greatest risks are associated with excessive and/or long-term consumption (278)Hydes TJ, Burton R, Inskip H, Bellis MA, Sheron N. A comparison of gender-linked population cancer risks between alcohol and tobacco: how many cigarettes are there in a bottle of wine? BMC Public Heal 2019 191. 2019;19(1):1-8.(279)NK L, AM B, JS K, JK M, AJ A. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36(1):83-93.(280)AJ W, LA D, CR W, DP S. Lifetime Alcohol Intake, Binge Drinking Behaviors, and Breast Cancer Risk. Am J Epidemiol. 2017;186(5):541-549.(281)B X, SP V, M Z, C M, Y Y, J M. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol. 2017;70(8):913-922. (see sidebar on Guidelines for Alcohol Consumption). In the United States, alcohol consumption accounted for greater than 75,000 cancer cases and nearly 19,000 cancer deaths annually between 2013 and 2016 (282)Goding Sauer A, Fedewa SA, Bandi P, et al. Proportion of cancer cases and deaths attributable to alcohol consumption by US state, 2013-2016. Cancer Epidemiol. 2021;71(PA):101893.. In the United States, consumption of alcohol has been rising in recent years (283)BH H, AA M, R F, JJ P. Binge Drinking Among Older Adults in the United States, 2015 to 2017. J Am Geriatr Soc. 2019;67(10):2139-2144.(284)Kanny D. Trends in Total Binge Drinks per Adult Who Reported Binge Drinking — United States, 2011–2017. MMWR Morb Mortal Wkly Rep. 2020;69(2):30-34.(285)National Cancer Institute. Cancer Trends Progress Report. Alcohol consumption. [updated 2021 Jul; cited 2021 Jul 10].. Concurrent with increases in consumption, rates of alcohol-related deaths have also increased at an alarming rate. According to a recent report, the age-adjusted rates of all alcohol-induced deaths among adults age 25 and older increased by 43 percent between 2006 and 2018 (286)Spencer MR, Curtin SC, Hedegaard H. Rates of alcohol-induced deaths among adults aged 25 and over in urban and rural areas: United States, 2000-2018. NCHS Data Brief 2020;383:1–8.. There are also concerns that the COVID-19 pandemic has further increased alcohol use in 2020 compared to previous years (287)Pollard MS, Tucker JS, Green HD. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Netw open. 2020;3(9)..
Beyond the United States, alcohol poses a significant public health challenge globally. In fact, alcohol-use disorders are now the most prevalent of all substance-use disorders worldwide (290)The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The lancet Psychiatry. 2018;5(12):987-1012., and in 2020, 4.1 percent of all new cases of cancer globally were attributed to alcohol consumption (291)Rumgay H, Shield K, Charvat H, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22(8):1071-1080.. These data underscore the importance of adhering to comprehensive guidelines to limit alcohol intake (for those who drink) and minimize the risk of developing a disease or dying due to alcohol. Future efforts focused on public education and evidence-based policy interventions, such as regulating alcohol retail density, taxes, and prices, need to be implemented along with effective clinical strategies to reduce the burden of alcohol-related cancers. In this regard, recent studies from Canada indicate that when alcohol bottles contain labels providing drinking guidelines, as well as, clear information on the risks of alcohol consumption, people are better informed about alcohol’s adverse effects and may limit their drinking (292)E H, A W, K V, et al. Testing Alcohol Labels as a Tool to Communicate Cancer Risk to Drinkers: A Real-World Quasi-Experimental Study. J Stud Alcohol Drugs. 2020;81(2):249-261.. Ongoing efforts are underway to implement similar policies requiring cancer-specific warning labels to be displayed on all alcoholic beverages in the United States (293)DEPARTMENT OF THE TREASURY ALCOHOL AND TOBACCO TAX AND TRADE. Published online 2020..
Protect Skin from UV Exposure
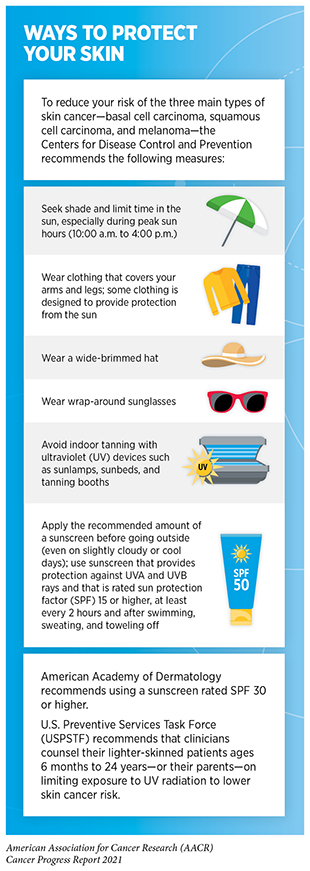
Three main types of skin cancer—basal cell carcinoma, squamous cell carcinoma, and melanoma which is the deadliest form of skin cancer—are largely caused by exposure to UV radiation from the sun or indoor tanning devices. In the United States, an estimated 91 percent of the total cases of melanoma during 2011–2015 could be attributed to UV exposure (294)F I, AG S, KD M, et al. Cutaneous melanomas attributable to ultraviolet radiation exposure by state. Int J cancer. 2020;147(5):1385-1390.. Sunburn, a clear indication of excessive exposure to UV radiation, is a preventable risk factor for skin cancer, and those events occurring in childhood pose the greatest risk (295)LK D, MJ V, LE BF, BJ S, DV D, JA C. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18(8):614-627.. Therefore, one of the most effective ways a person can reduce his or her risk of skin cancer is by practicing sun-safe habits and not using UV indoor tanning devices (see sidebar on Ways to Protect Your Skin).
In the United States, melanoma incidence has been rising for decades—incidence in 2018 was six times higher than it was in 1975 (4)Surveillance, Epidemiology, and End Results (SEER) Program.(184)AACR cancer progress report 2018: Harnessing research discoveries for patient benefit. Clin Cancer Res. 2018;24(18).(296)Welch HG, Mazer BL, Adamson AS. The Rapid Rise in Cutaneous Melanoma Diagnoses. N Engl J Med. 2021;384(1).. While ongoing research will determine the relative contribution of UV exposure versus increased screening through skin examinations to this rapid rise in melanoma cases (296)Welch HG, Mazer BL, Adamson AS. The Rapid Rise in Cutaneous Melanoma Diagnoses. N Engl J Med. 2021;384(1)., it is vital that all sectors including health care, the federal government, business, advocacy, and communities coordinate efforts to reduce risk exposure for all skin cancers through public health campaigns such as those encouraging sun-protective behaviors as well as evidence-based public policies. Public education regarding skin cancer risk reduction is extremely important considering findings from a recent survey which found that one third of its participants lacked a basic understanding of skin cancer and sun protection practices that can help reduce their risk of skin cancer (297)American Academy of Dermatology Association. New American Academy of Dermatology survey finds one-third of Americans fail basic quiz on skin cancer and sun exposure. 2021 Apr 27..
As of January 1, 2021, in the U.S., 20 states and the District of Columbia have laws prohibiting tanning for minors (under the age of 18) without exemptions (273)American Cancer Society. Cancer prevention & early detection facts & figures 2019-2020. Atlanta: American Cancer Society; 2019.. There is evidence that these policies are in fact effective in reducing tanning practice. As one example, a 2013 New Jersey legislation banning indoor tanning for those 17 and under led to a 50 percent reduction in the prevalence of indoor tanning among high school students in 2018 compared to 2012 (298)Stapleton JL, Hrywna M, Coups EJ, Delnevo C, Heckman CJ, Xu B. Prevalence and location of indoor tanning among high school students in newjersey 5 years after the enactment of youth access restrictions. JAMA Dermatology. 2020;156(11).. The health and economic benefits of banning indoor tanning are also highlighted in recent studies that estimate the cost benefits of such policies. For instance, in a new analysis, researchers project that a national policy banning tanning beds among the 17.1 million minors ages 14 to 17 years residing in the United States would prevent more than 15,000 melanoma cases and save $205 million in health care costs over their lifetimes (299)Eskander A, Marqueen KE, Edwards HA, et al. To ban or not to ban tanning bed use for minors: A cost-effectiveness analysis from multiple US perspectives for invasive melanoma. Cancer. 2021;127(13)..
Prevent and Eliminate Infection with Cancer-causing Pathogens
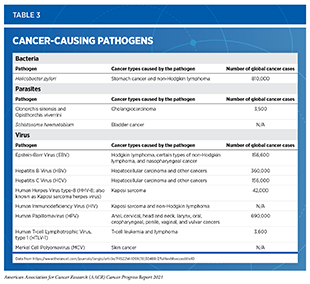
Persistent infection with several pathogens—bacteria, viruses, and parasites that cause disease—increases a person’s risk for several types of cancer (see Table 3). Globally, an estimated 13 percent of all cancer cases in 2018 were attributable to infection, with more than 90 percent of these cases attributable to just four pathogens: human papillomavirus (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), and Helicobacter pylori (300)de Martel C, Georges D, Bray F, et al. Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis. Lancet Glob Heal. 2020;8(2):e180-e190.(301)CY H, DH S, D K, et al. Incidence of extrahepatic cancers among individuals with chronic hepatitis B or C virus infection: A nationwide cohort study. J Viral Hepat. 2020;27(9):896-903.. In the United States, about 3 percent of all cancer cases are attributable to infection with pathogens (181)Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. 2018;68(1):31-54.. Individuals can significantly lower their risks by protecting themselves from infection or by obtaining treatment, if available, to eliminate an infection (see sidebar on Preventing or Eliminating Infection with the Four Main Cancer-causing Pathogens). It is important to note that even though strategies to eliminate, treat, or prevent infection with Helicobacter pylori, HBV, HCV, and HPV can significantly lower an individual’s risks for developing cancers, these strategies are not effective at treating infection-related cancers once they develop.
Chronic infection with HBV and HCV can cause liver cancer and is increasingly recognized as a risk factor for additional malignancies such as non-Hodgkin lymphoma. Despite the availability of a safe and effective vaccine, in the United States, the rate of acute HBV cases as well as the age-adjusted HBV-associated deaths has not changed between 2012 and 2019 (194)Centers for Disease Control and Prevention. Viral hepatitis surveillance – United States. [cited 2021 Jul 10].. Acute infection with HCV is often asymptomatic but more than half of these cases progress to chronic infection. Therefore, it is extremely concerning that the rate of reported acute HCV cases in the United States increased by 89 percent between 2014 and 2019 with most cases occurring among individuals ages 20–39 years (194)Centers for Disease Control and Prevention. Viral hepatitis surveillance – United States. [cited 2021 Jul 10].. Unfortunately, many HCV-positive individuals are unaware of their status (302)Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly Reported Acute and Chronic Hepatitis C Cases ― United States, 2009–2018 . MMWR Morb Mortal Wkly Rep. 2020;69(14).. Collectively, these data prompted CDC and USPSTF to update their screening recommendation to suggest universal HCV screening at least once in their lifetime for all average-risk individuals age 18 to 79 years (303)DK O, KW D, AH K, et al. Screening for Hepatitis C Virus Infection in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323(10):970-975.(304)Schillie S. CDC Recommendations for Hepatitis C Screening Among Adults — United States, 2020. MMWR Recomm Reports. 2020;69(2):1-17.. Notably, testing for HCV declined by 59 percent in 2020 due to the COVID-19 pandemic compared to prior years (305)Kaufman HW, Bull-Otterson L, Meyer WA 3rd, Huang X, Doshani M, Thompson WM, et al. Decreases in hepatitis C testing and treatment during the COVID-19 pandemic. Am J Prev Med 2021 May 10.. While it is reassuring that HCV testing started to rebound later during the year after the first peak of the pandemic, continued public education and policy implementation would be required to prevent any long-term adverse consequences on public health. To eliminate viral hepatitis as a public health threat, U.S. Department of Health and Human Services recently released the Viral Hepatitis National Strategic Plan for the United States: A Roadmap to Elimination (2021–2025) (306)U.S. Department of Health and Human Services. 2020. Viral hepatitis national strategic plan for the United States: a roadmap to elimination (2021–2025). Washington, DC.. The primary goals listed in the report are to prevent new infections, improve hepatitis-related health outcomes for infected individuals, reduce disparities and health inequities related to hepatitis, improve surveillance of viral hepatitis, and bring together all relevant stakeholders in coordinating efforts to address the hepatitis epidemic.
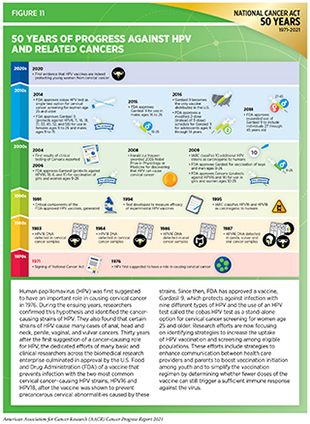
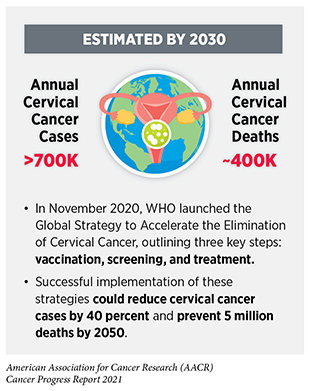
Persistent infection with HPV is responsible for almost all cervical cancers, 90 percent of anal cancers, about 70 percent of oropharyngeal cancers, and more than half of all vaginal, vulvar, and penile cancers (307)Centers for Disease Control and Prevention. HPV and cancer: cancers associated with human papillomavirus (HPV).. This knowledge has driven the development of vaccines that prevent infection with some cancer-causing strains of HPV and the development of a clinical test that detects cancer-causing HPV strains in cervical cells (see Figure 11). There are 13 different types of HPV that can cause cancers; the HPV vaccine currently used in the United States, Gardasil 9, can protect against nine of these HPV strains (307)Centers for Disease Control and Prevention. HPV and cancer: cancers associated with human papillomavirus (HPV).. There is emerging evidence confirming that the receipt of guideline-concordant HPV vaccination significantly lowers the risk of infection with HPV types that are covered by the vaccines and dramatically reduces the incidence of cervical cancers among the vaccinated (308)Rosenblum HG, Lewis RM, Gargano JW, Querec TD, Unger ER, Markowitz LE. Declines in Prevalence of Human Papillomavirus Vaccine-Type Infection Among Females after Introduction of Vaccine — United States, 2003–2018. MMWR Surveill Summ. 2021;70(12).(309)Lei J, Ploner A, Elfström KM, et al. HPV Vaccination and the Risk of Invasive Cervical Cancer. 2020;383(14):1340-1348.(310)Mix JM, van Dyne EA, Saraiya M, Hallowell BD, Thomas CC. Assessing impact of HPV vaccination on cervical cancer incidence among women aged 15–29 years in the United States, 1999–2017: An ecologic study. Cancer Epidemiol Biomarkers Prev. 2021;30(1).. According to a recent analysis of data from nearly 1.7 million women from Sweden, HPV vaccination before the age of 17 years was shown to lower the risk of cervical cancer incidence by nearly 90 percent (309)Lei J, Ploner A, Elfström KM, et al. HPV Vaccination and the Risk of Invasive Cervical Cancer. 2020;383(14):1340-1348.. Unfortunately, the uptake of HPV vaccines has been suboptimal in the United States. Even though there has been some progress in the uptake of vaccines in recent years, only 56 percent of boys and 61 percent of girls who are eligible were up to date on their vaccination regimen in 2020 (311)Pingali C. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years — United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(35):1183-1190..
All stakeholders must work together and develop better strategies to increase the uptake of HPV vaccination in the United States. These include increasing health care provider recommendations to eligible adolescents and their parents, improving provider-parent communication, increasing parental awareness, and removing structural and financial barriers to increase access to vaccination. In this regard, a recent clinical trial conducted at 48 pediatric practices across 19 states showed that training pediatric clinicians on strategies on how to communicate with parents led to a reduction in missed opportunities for HPV vaccination and an increase in rates of HPV vaccination initiation (313)Szilagyi PG, Humiston SG, Stephens-Shields AJ, et al. Effect of Training Pediatric Clinicians in Human Papillomavirus Communication Strategies on Human Papillomavirus Vaccination Rates: A Cluster Randomized Clinical Trial. JAMA Pediatr. Published online 2. However, recent data also show that while more physicians recommended the HPV vaccine to unvaccinated youth in 2018 compared to 2012, even in 2018, half of the more than seven million youth who were eligible for vaccination did not receive a recommendation from their providers (314)Sonawane K, Zhu Y, Lin Y-Y, et al. HPV Vaccine Recommendations and Parental Intent. Pediatrics. 2021;147(3):e2020026286.. Additionally, it is concerning that hesitancy around the HPV vaccine has increased among parents and that misinformation about vaccination is playing a role in the increased hesitancy (314)Sonawane K, Zhu Y, Lin Y-Y, et al. HPV Vaccine Recommendations and Parental Intent. Pediatrics. 2021;147(3):e2020026286..
Currently, health care providers across the United States are facing similar challenges with hesitancy and misinformation with regard to the SARS-CoV2 vaccines. To confront the adverse impacts of misinformation, the U.S. Surgeon General has released a public statement to draw attention to this serious public health issue and provide recommendations on how it could be addressed (315)Murthy VH. Confronting health misinformation: the U.S. Surgeon General’s advisory on building a healthy information environment.. To accelerate our progress against HPV-related cancers and other infectious diseases such as COVID-19, it is vital that evidence-based interventions are implemented in both health care and community settings to enhance public trust in vaccination as well as other preventive measures that improve health outcomes.
Be Cognizant of Reproductive and Hormonal Influences
Breastfeeding
Studies have shown that having children reduces the risk of a common type of breast cancer, estrogen receptor-positive tumors, in mothers but increases the risk of breast cancers that are estrogen receptor negative (316)Ambrosone CB, Higgins MJ. Relationships between breast feeding and breast cancer subtypes: Lessons learned from studies in humans and in mice. Cancer Res. 2020;80(22).(317)Lord SJ, Bernstein L, Johnson KA, et al. Breast cancer risk and hormone receptor status in older women by parity, age of first birth, and breastfeeding: A case-control study. Cancer Epidemiol Biomarkers Prev. 2008;17(7).. There is also strong evidence that breastfeeding decreases the risk of breast cancer in mothers (318)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the risk of cancer..
Notably, breastfeeding greatly reduces the increased risk of estrogen receptor-negative cancers that are associated with having children. Women who breastfeed also have a lower risk of a particularly aggressive type of breast cancer known as triple-negative breast cancer (319)JR P, E V, MA T, et al. Parity, lactation, and breast cancer subtypes in African American women: results from the AMBER Consortium. J Natl Cancer Inst. 2014;106(10).. According to recent data, breastfeeding is associated with a 22 percent reduction in the risk of developing triple-negative breast cancer, whereas weaker or no correlations have been observed with other types of breast cancer (320)F I, Y L, A J, et al. Breastfeeding and breast cancer risk by receptor status–a systematic review and meta-analysis. Ann Oncol Off J Eur Soc Med Oncol. 2015;26(12):2398-2407.. Emerging evidence suggests that breastfeeding may also be associated with a lower risk of ovarian cancer, conferring reduction of cancer risk in both white and African American women (321)PG M, AJ A, EV B, et al. Reproductive factors and ovarian cancer risk in African-American women. Ann Epidemiol. 2016;26(9):654-662.(322)A B, N S, BA R, et al. Association Between Breastfeeding and Ovarian Cancer Risk. JAMA Oncol. 2020;6(6).. Unfortunately, according to a recent national survey, fewer than 40 percent of U.S. women are aware of the benefits of breastfeeding in reducing cancer risk (323)Hoyt-Austin A, Dove MS, Abrahão R, Kair LR, Schwarz EB. Awareness That Breastfeeding Reduces Breast Cancer Risk: 2015-2017 National Survey of Family Growth. Obstet Gynecol. 2020;136(6):1154-1156.. Increasing public awareness of this information is important if we are to increase breastfeeding initiation among all women. It would also be critical to identify targeted interventions for certain population groups, such as African American women, who have a disproportionately high incidence of triple-negative breast cancer and a lower prevalence of breastfeeding compared to all other U.S. racial and ethnic groups (324)Chiang K V., Li R, Anstey EH, Perrine CG. Racial and Ethnic Disparities in Breastfeeding Initiation ─ United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70(21).(325)Beauregard JL. Racial Disparities in Breastfeeding Initiation and Duration Among U.S. Infants Born in 2015. MMWR Morb Mortal Wkly Rep. 2019;68(34):745-748..
Hormone Replacement Therapy
Hormone replacement therapy (HRT) refers to treatments that aim to relieve the common symptoms of menopause and the long-term biological changes, such as bone loss, that occur after menopause. These changes occur due to the decline in the levels of the hormones estrogen and progesterone in a woman’s body. HRT usually involves treatment with estrogen alone or estrogen in combination with progestin, a synthetic hormone similar to progesterone. Women who have a uterus are prescribed estrogen plus progestin. This is because estrogen alone, but not in combination with progestin, is associated with an increased risk of endometrial cancer, a type of cancer that forms in the tissue lining the uterus. Estrogen alone is used only in women who have had their uteruses removed.
Some of the most comprehensive evidence about the health effects of HRT was obtained from clinical trials conducted by NIH as part of the Women’s Health Initiative (WHI). The data indicated that women who use estrogen plus progestin have an increased risk of developing breast cancer (326)RT C, GL A, AK A, et al. Association of Menopausal Hormone Therapy With Breast Cancer Incidence and Mortality During Long-term Follow-up of the Women’s Health Initiative Randomized Clinical Trials. JAMA. 2020;324(4):369-380.(327)RT C, G A, M P, et al. Estrogen plus progestin and breast cancer detection by means of mammography and breast biopsy. Arch Intern Med. 2008;168(4):370-377.. The risk is greater with longer duration of use (328)Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet (London, England). 2019;394(10204):1159-1168.(329)RT C, LH K, RL P, et al. Breast cancer after use of estrogen plus progestin in postmenopausal women. N Engl J Med. 2009;360(6):573-587.. Women who are no longer using HRT have a lower risk than current users but remain at an elevated risk for more than a decade after they have stopped taking the drugs (328)Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet (London, England). 2019;394(10204):1159-1168.. Notably, the increased risks were observed both for white and Black women (330)Rosenberg L, Bethea TN, Viscidi E, et al. Postmenopausal Female Hormone Use and Estrogen Receptor–Positive and –Negative Breast Cancer in African American Women. JNCI J Natl Cancer Inst. 2016;108(4):361.(331)Ellingjord-Dale M, Vos L, Tretli S, Hofvind S, dos-Santos-Silva I, Ursin G. Parity, hormones and breast cancer subtypes – results from a large nested case-control study in a national screening program. Breast Cancer Res. 2017;19(1).. A recent analysis from the United Kingdom corroborated the data from the WHI and showed that treatment with estrogen plus progestin is associated with a 26 percent increase in the risk of breast cancer (332)Vinogradova Y, Coupland C, Hippisley-Cox J. Use of hormone replacement therapy and risk of breast cancer: Nested case-control studies using the QResearch and CPRD databases. BMJ. 2020;371.. All individuals who are seeking relief from menopausal symptoms should discuss with their health care providers the advantages and possible risks of using HRT before deciding what is right for them.
Limit Exposure to Environmental Carcinogens
Environmental exposures to pollutants and certain occupational agents can increase a person’s risk of cancer. For example, radon, a naturally occurring radioactive gas that comes from the breakdown of uranium in soil, rock, and water, is the second leading cause of lung cancer death in the United States although levels of naturally occurring radon vary widely based on geographic location within the country (273)American Cancer Society. Cancer prevention & early detection facts & figures 2019-2020. Atlanta: American Cancer Society; 2019.(333)National Cancer Institute, NIH, DHHS. Cancer trends progress report. Bethesda, MD, 2021 Jul.. Other examples of environmental carcinogens include arsenic, asbestos, lead, radiation, and benzene (334)U.S. Department of Health and Human Services. 14th report on carcinogens. [updated 2016 Nov 3; cited 2021 Jul 10].. According to the WHO, environmental risk factors account for nearly 20 percent of all cancers globally, most of which occur in low- and middle-income countries.
It can be difficult for people to avoid or reduce their exposure to environmental carcinogens, and not every exposure will lead to cancer. The intensity and duration of exposure, combined with an individual’s biological characteristics such as genetic makeup, and lifestyle factors determine each person’s chances of developing cancer over his or her lifetime. In addition, when studying environmental cancer risk factors, it is important to consider that exposure to several environmental cancer risk factors may occur simultaneously. Growing knowledge of the environmental pollutants to which different segments of the U.S. population are exposed highlights new opportunities for education and policy initiatives to improve public health.
Outdoor air pollution is classified by the International Agency for Research on Cancer (IARC), an affiliate of the WHO, as a potential cause of cancer in humans (336)D L, Y G, B L-S, et al. The carcinogenicity of outdoor air pollution. Lancet Oncol. 2013;14(13):1262-1263.. Two types of air pollution are most common in the United States: ozone and particle pollution. Particle pollution refers to a mix of tiny solid and liquid particles that are in the air we breathe, and in 2013, IARC concluded that particle pollution may cause lung cancer (195)American Lung Association. Key findings: state of the air. [cited 2021 Jul 10].. Therefore, it is concerning that nearly 21 million people in the United States were exposed year-round to unhealthy levels of particle pollution between 2017 and 2019 (195)American Lung Association. Key findings: state of the air. [cited 2021 Jul 10].. Communities of color and people living in poverty were at an increased risk of being exposed to polluted air (195)American Lung Association. Key findings: state of the air. [cited 2021 Jul 10].. Therefore, new policies to reduce the release of pollutants into the atmosphere are urgently needed to combat the adverse health effects of air pollution.
Involuntary exposures to many of the environmental pollutants are usually higher in subgroups of the population, such as workers in certain industries who may be exposed to carcinogens on the job, racial and ethnic minorities, or individuals living in low-income neighborhoods. Similarly, there are disparities in the burden of cancers caused by environmental exposures based on geographic locations and socioeconomic status (337)Baurick T, Younes L, Meiners J. Welcome to “cancer alley,” where toxic air is about to get worse. ProPublica 2019 Oct 30. Available from:. https://www.propublica.org/article/welcome-to-cancer-alley-where-toxic-air-is-about-to-get-worse. As we learn more about environmental and occupational cancer risk factors and identify those segments of the U.S. population who are exposed to these factors, new and/or more effective policies need to be developed and implemented for the benefit of all populations, especially the most vulnerable and underserved.