Discovery Science Driving Clinical Breakthroughs
In this section, you will learn:
- Genetic and epigenetic characteristics of cancer cells, unveiled by discovery science, are being leveraged to develop novel and innovative treatments for cancer.
- Clinical breakthroughs across all pillars of cancer treatment—surgery, radiotherapy, chemotherapy, molecularly targeted therapy, and immunotherapy—are saving and improving lives.
- There is an urgent need of clinical trials to include patients from diverse ethnic and racial backgrounds to fully realize the potential of precision medicine.
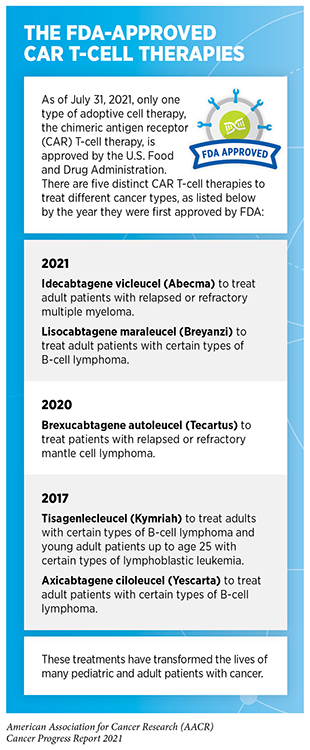
- From August 1, 2020 to July 31, 2021, FDA has approved 16 new anticancer therapeutics that include a revolutionary therapeutic against an altered form of the long intractable protein, KRAS, for certain patients with lung cancer, and the first adoptive cell therapy to treat patients with multiple myeloma.
- During the same period, FDA has expanded the use of 11 previously approved anticancer therapeutics to treat additional cancer types, bringing the promise of research-driven clinical breakthroughs to more patients.
Breakthroughs across the spectrum of cancer science and medicine are improving survival and quality of life for patients around the globe. These advances against cancer are driven by concerted efforts from stakeholders working throughout the medical research cycle (Figure 16).
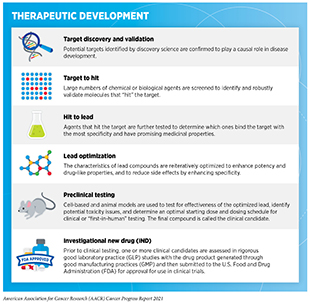
Medical Research
Medical research is a hypothesis-driven, years-long process with the goal of refining and improving clinical care for all individuals (see Figure 16). Researchers use a new discovery or observation at any step of the medical research cycle as a basis to develop a hypothesis. The hypothesis addresses one or more questions, with the potential to improve the practice of medicine or public health, through experiments in a wide range of models that mimic healthy and diseased conditions. Findings from these experiments can lead to new therapeutic targets, inform potential preventive interventions, identify approaches for early diagnosis, or uncover predictive or prognostic biomarkers, each of which has the potential to drive clinical care forward. Once a potential therapeutic target is identified, several candidate therapeutics against the target are rigorously tested to determine the appropriate dosage, dosing schedules, and potential toxicities (see sidebar on Therapeutic Development). These preclinical studies help determine the most promising candidates, which are then tested in a clinical trial.
Clinical Studies
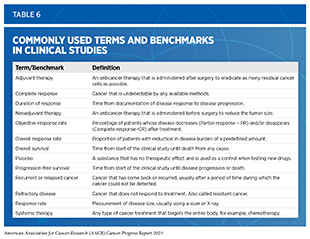
Clinical studies are the backbone of medical research and, together with basic research, provide the foundational knowledge to bring safe and effective medicines to patients in a timely manner. Evidence gathered from clinical studies, also called clinical trials, is reviewed by FDA to determine whether a therapeutic should be approved for use in the clinic. There are many types of clinical trials and each is designed to address different research questions (384)Li A, Bergan RC. Clinical trial design: Past, present, and future in the context of big data and precision medicine. Cancer. 2020;126(22).(see sidebar on Types of Clinical Trials). Because clinical trials involve the use of experimental therapeutics and aim to derive conclusions for the entire population based on data from a cohort of participants, their design and conduct are reviewed and approved by institutional review boards. Clinical trials are closely monitored throughout the duration of the study to ensure safety of the participants.
Clinical trials testing the efficacy and safety of candidate anticancer therapeutics are traditionally conducted in three consecutive phases (see Figure 17). This approach requires substantial investment, thousands of participants, and many years to complete clinical trials. The result is a lengthy and costly undertaking that poses major barriers to rapidly translating discoveries into clinical advances.
To reduce the length of time it takes for patients to access new treatments for life-threatening diseases such as cancer, FDA—the federal agency that oversees clinical trials and drug approvals—has made important procedural changes to expedite the conduct and review of clinical trials. In the past three decades, FDA has introduced expedited review processes to minimize approval times for promising new therapeutics. According to a recent study examining FDA approvals of anticancer drugs from 2012 to 2017, the approval time through accelerated review process took an average of six years compared to more than eight years for regular approvals during the same period (385)Van Norman GA. Update to Drugs, Devices, and the FDA: How Recent Legislative Changes Have Impacted Approval of New Therapies. JACC Basic to Transl Sci. 2020;5(8).. While the expedited review processes have substantially shortened the time that it takes for novel anticancer therapeutics to reach patients, long-term studies are needed to confirm whether therapeutics approved through these pathways result in increased overall survival and/or improved quality of life for cancer patients.
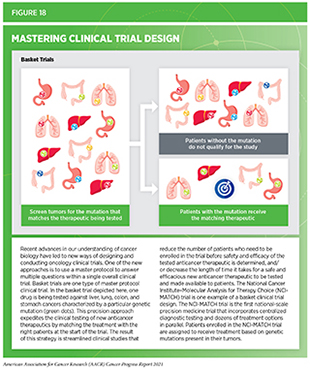
Progress across the continuum of cancer research and care is also improving the design and execution of clinical trials. In 2018, FDA issued guidance for researchers and the pharmaceutical industry to adopt an improved design for clinical trials (see Figure 18). The new strategy—also called the master protocol design—proposes an adaptive and seamless approach to conducting clinical trials for testing the efficacy and safety of new anticancer therapeutics (388)U.S. Food & Drug Adminstration. Master protocols: efficient clinical trial design strategies to expedite development of oncology drugs and biologics guidance for industry, draft guidance for industry. 2018 Oct..
Master protocol design aims to streamline clinical trials by: 1) matching the right therapeutics with the right patient more quickly; 2) reducing the number of patients needed to test the efficacy and safety of the drug; and 3) decreasing the length of time it takes for a new anticancer therapeutic to be tested and made available to patients if the trial shows it is safe and effective (389)Ajmera Y, Singhal S, Dwivedi SN, Dey AB. The changing perspective of clinical trial designs. Perspect Clin Res. 2021;12(2).. Furthermore, the master protocol design addresses multiple questions within a single overall clinical trial. Advances in our understanding of the genetic mutations that drive cancer development are further helping to shape clinical trial design. As an example, “basket” trials allow researchers to test one anticancer drug in a group of patients with a common genetic mutation against which the drug is targeted, regardless of the tissue of origin of the cancer (386)Park JJH, Hsu G, Siden EG, Thorlund K, Mills EJ. An overview of precision oncology basket and umbrella trials for clinicians. CA Cancer J Clin. 2020;70(2).(see Figure 18).
Despite improvements in both the clinical trial design and drug approval processes, there are other opportunities to further minimize the time it takes for a lifesaving anticancer therapeutic to reach patients who will benefit from it the most. The COVID-19 pandemic, despite its adverse effects on nearly all aspects of cancer science and medicine, has also offered a blueprint of success to further revise and reform the clinical trial enterprise and the drug approval process for the benefit of cancer patients (see the sidebar on Lessons from COVID-19 to Streamline Oncology Clinical Trials).
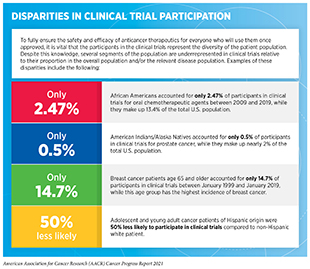
The urgency with which all stakeholders have come together and shared data and resources like never before, led to the unprecedented speed of vaccine development against SARS-CoV-2 (391)Katib AA. Research ethics challenges during the COVID-19 pandemic: what should and what should not be done. J Ideas Heal. 2020;3(Special1)., the virus that causes COVID-19. However, there are still many challenges that need to be addressed. One of the most pressing challenges is that racial and ethnic minorities continue to be significantly underrepresented in many clinical trials, including those testing new anticancer therapeutics and the COVID-19 vaccines (see sidebar on Disparities in Cancer Clinical Trial Participation). This lack of diversity, perpetuated in part by systemic and structural racism, poses a threat to the promise of equitable personalized medicine for all. It is imperative that stakeholders across the continuum of cancer science and medicine come together to increase diversity in clinical trial participation. This vision can be achieved by developing multipronged strategies that include, among others, educating clinical researchers about approaching and encouraging patients from diverse backgrounds to participate in clinical trials; simplifying eligibility criteria and logistics for patients to participate in clinical studies; and implementing effective education and policy initiatives aimed at reducing hesitancy among racial and ethnic minorities to participate in clinical research.
Progress Across the Spectrum of Cancer Treatment
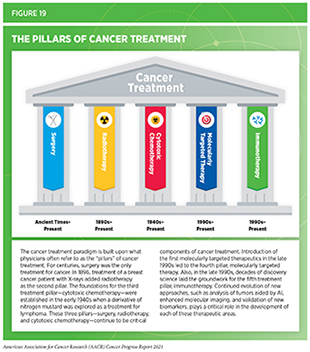
Discovery science continuously drives breakthroughs in cancer etiology, prevention, detection, diagnosis, treatment, and survivorship. Clinical breakthroughs that lead to the FDA approval of anticancer therapeutics and medical devices, in turn, accelerate the pace of the medical research cycle through new real-world observations (see Figure 16) (see Supplemental Table 2(Pt.1)(Pt.2), and Supplemental Table 3). The overall goal is to refine and/or expand the five pillars—surgery, chemotherapy, radiotherapy, molecularly targeted therapy, and immunotherapy—that constitute the current paradigm for cancer treatment (396)Falzone L, Salomone S, Libra M. Evolution of cancer pharmacological treatments at the turn of the third millennium. Front Pharmacol. 2018;9(NOV).(see Figure 19).
This section primarily discusses 16 new anticancer therapeutics, three new diagnostic imaging agents, and two new medical devices approved by FDA during the time frame—August 1, 2020 to July 31, 2021—covered by this report. Also highlighted are the 11 previously approved anticancer therapeutics that were approved by FDA for treating additional types of cancer during the same time (see Table 5 and Supplemental Table 4). Not discussed are the previously approved anticancer drugs for which FDA approved either a supplementary dosing schedule or additional uses during treatment of the same cancer type for which they were originally approved, for example, an expansion for treatment at a less advanced stage of the disease.
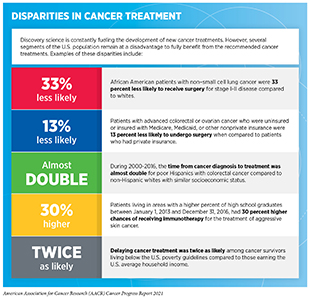
As we make strides toward effectively treating cancer, it is also important to note that not all patients receive and/or benefit from the care recommended for the type and stage of cancer for which they have been diagnosed. Gaps in equitable and affordable access to cancer treatment for patients from all walks of life can result in adverse survival rates that disproportionately affect certain population groups (sidebar on Disparities in Cancer Treatment). It is essential for stakeholders across the cancer research continuum to urgently and collectively address these disparities if the vision of equitable cancer care is to be realized.
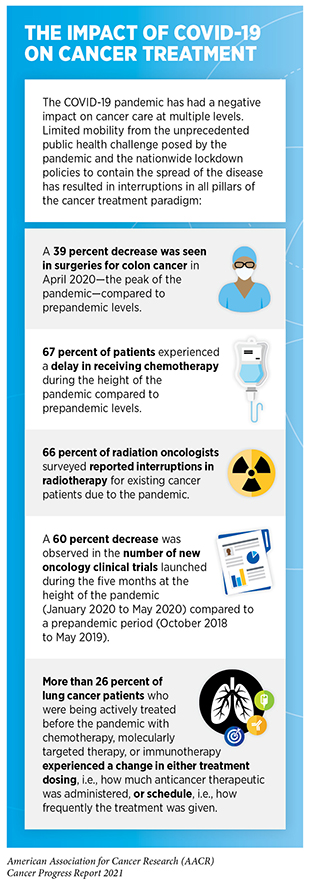
In addition to the existing challenges in the delivery of cancer treatment, the COVID-19 pandemic has created some unique barriers for patients during the past two years. The setbacks from the COVID-19 pandemic on screening rates for various cancer types are likely to have long-term effects on late-stage cancer diagnosis and outcomes for patients. In terms of treatment, cancer patients have experienced serious interruptions across all five pillars of the cancer treatment paradigm, for example, cancellations of anticancer therapies that can only be administered in a medical facility (see sidebar on The Impact of COVID-19 on Cancer Treatment). COVID-19 has also highlighted areas where lessons learned from the pandemic can help revise cancer treatment and care strategies to improve the lives of cancer patients. For example, the pandemic has spurred a shift toward telehealth, which is the distribution of health-related services from health care providers to patients using telecommunication technologies (407)Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract. 2021;17(2).. Another effect of the pandemic on cancer care is the rethinking of when and how anticancer therapeutics are administered. Over the past year, FDA has taken several steps that can reduce the number of times a patient must visit a health care facility for cancer treatment. For example, in April 2020, the agency approved an alternative dosing schedule for the immunotherapeutic pembrolizumab (Keytruda), which is approved for treating a wide array of cancer types (see Releasing the Brakes on the Immune System). Pembrolizumab is administered intravenously, meaning that patients must travel to a health care facility to receive the treatment. The new dosing regimen of 400 mg of pembrolizumab every six weeks provides an alternative to the standard 200 mg every three weeks. In September 2020, FDA approved azacitidine (Onureg) as maintenance therapy for patients with acute myeloid leukemia (AML) in a tablet form, making it easier for adult AML patients to manage their disease effectively without the need to visit a health care facility for the traditional intravenous administration of the drug. As a result, cancer patients have experienced, among other benefits, reduced travel, decreased social anxiety associated with hospital visits, and increased financial savings.
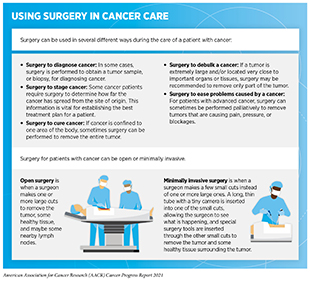
Advances in Cancer Treatment with Surgery
Surgery was the only available treatment for cancer for centuries (see Figure 19) and remains an important treatment option for many patients (see sidebar on Using Surgery for Cancer Treatment). A recent study shows that the global demand for surgery to treat cancer will increase by 52 percent by 2040 (413)Perera SK, Jacob S, Wilson BE, et al. Global demand for cancer surgery and an estimate of the optimal surgical and anaesthesia workforce between 2018 and 2040: a population-based modelling study. Lancet Oncol. 2021;22(2).. Researchers are continuously innovating new and improved strategies to maximize the benefit and minimize harms from surgery for cancer patients.
As new treatments are added across the pillars of cancer treatment (see Figure 19), a common approach to treating patients with cancer has been to use surgery alongside one or more classes of therapies available for the diagnosed cancer type. For many cancers, a multidisciplinary team including surgical, medical, and radiation therapy oncologists as well as other individuals as appropriate (e.g., other medical specialists, nurses, social workers) reviews treatment options and makes recommendations for treatment. Sometimes, additional therapy is given prior to surgery (neoadjuvant), both before and after surgery (perioperative), or after surgery (adjuvant) with the decision based on specifics of the situation. (414)Burotto M, Wilkerson J, Stein WD, Bates SE, Fojo T. Adjuvant and neoadjuvant cancer therapies: A historical review and a rational approach to understand outcomes. Semin Oncol. 2019;46(1).. The primary goal of these therapies is to eliminate any cancer cells that surgery might not remove. When given in the neoadjuvant or perioperative setting, they may also improve the surgeon’s ability to remove the tumor. Researchers have found that neoadjuvant, perioperative, and adjuvant therapies can significantly increase overall survival and/or quality of life in the appropriate clinical settings (414)Burotto M, Wilkerson J, Stein WD, Bates SE, Fojo T. Adjuvant and neoadjuvant cancer therapies: A historical review and a rational approach to understand outcomes. Semin Oncol. 2019;46(1).(see Table 6).
Treating a Rare Bone Tumor with an Innovative Noninvasive Procedure
Osteoid osteoma is a benign, rare bone tumor, which commonly occurs in children and young adults (415)Carneiro BC, Da Cruz IAN, Ormond Filho AG, et al. Osteoid osteoma: the great mimicker. Insights Imaging. 2021;12(1).. The most significant symptom of osteoid osteoma is pain. Current standard of care is removal of the tumor either by surgery or by computed tomography-guided radiotherapy (see sidebar on Using Radiation in Cancer Treatment). In November 2020, FDA approved Sonalleve Magnetic Resonance-guided High Intensity Focused Ultrasound (MR-HIFU) system, an innovative device that altogether eliminates the need for a scalpel or needle to treat osteoid osteomas. Instead, the device delivers focused ultrasound energy inside a lesion in a precise and controlled manner using an external applicator. In a clinical study, eight of the nine patients showed long-term relief from pain within four weeks of treatment and did not need any pain medication (416)Sharma K V., Yarmolenko PS, Celik H, et al. Comparison of Noninvasive High-Intensity Focused Ultrasound with Radiofrequency Ablation of Osteoid Osteoma. J Pediatr. 2017;190.. The remarkable benefit of a noninvasive procedure for patients with osteoid osteomas, like Niyati Shah, highlights how innovative technologies are transforming the lives of patients, including those with rare tumor types.
Using Artificial Intelligence for Precision in Surgical Oncology
Rapid progress in the fields of artificial intelligence (AI) and machine learning (ML) is transforming the landscape of cancer research and care (see Looking to the Future)(417)Liang G, Fan W, Luo H, Zhu X. The emerging roles of artificial intelligence in cancer drug development and precision therapy. Biomed Pharmacother. 2020;128.. During the 12-month span covered in this report, FDA has authorized marketing of Hepatica, an AI-driven software that helps clinicians in making informed decisions before surgical removal of liver cancer. Hepatica uses noninvasive magnetic resonance imaging to provide an assessment of liver health. This assessment is based on dividing the liver into small segments digitally, combining these digital segments of liver with information obtained from biomarkers that detect liver inflammation, and using an integrated AI algorithm to provide an evaluation of liver health. Using AI to delineate the size and health of liver takes 20 fewer minutes per patient compared to the traditional evaluation by a radiologist, thus saving valuable preoperative time. Initial results from a study involving 143 patients with liver cancer, who were surgical candidates, showed that Hepatica effectively identified patients at risk of poor outcomes from surgery and a longer hospital stay, thus preventing unnecessary surgical procedures (418)Mole DJ, Fallowfield JA, Sherif AE, et al. Quantitative magnetic resonance imaging predicts individual future liver performance after liver resection for cancer. PLoS One. 2020;15(12 December).. More than 42,000 new diagnoses of, and more than 30,000 deaths from, liver cancer are estimated in 2021 in the United States (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Information gleaned from Hepatica can inform clinicians to better assess whether a patient is a good candidate for surgery and will benefit from it to treat liver cancer. Knowing precisely which parts of the liver need removing will also guide surgeons to avoid unnecessary removal of healthy tissue.
Researchers are also developing AI-based tools to ensure that all of the tumor tissue is removed during surgery. As an example, scientists have created a new microscope that can rapidly visualize relatively thick pieces of tissue with cellular resolution, allowing for inspection of margins between healthy tissue and the tumor within minutes of surgical removal. The microscope uses an AI program to optimize the collection and analysis of tissue images during surgery. As a result, it takes less time for surgeons to detect any leftover tumor tissue during the procedure, while potentially increasing the accuracy of detection (419)Jin L, Tang Y, Wu Y, et al. Deep learning extended depth-of-field microscope for fast and slide-free histology. Proc Natl Acad Sci U S A. 2021;117(52).. This approach can be further enhanced by molecular imaging approaches, which are currently being developed.
Improving Surgical Outcomes for Patients with Early-stage Cervical Cancer
Roughly 44 percent of women with cervical cancer are diagnosed at an early stage, when tumors are small and cancer has not spread beyond the cervix (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. The most common treatment for women diagnosed with early-stage cervical cancer is removal of the uterus either by open surgery or using minimally invasive surgical procedures. In 2018, results from a clinical trial showed that traditional open surgery for early-stage cervical cancer was superior to minimally invasive surgery (420)Ramirez PT, Frumovitz M, Pareja R, et al. Minimally Invasive versus Abdominal Radical Hysterectomy for Cervical Cancer. N Engl J Med. 2018;379(20).. Researchers found that even though minimally invasive surgery caused less blood loss during the procedure, shortened length of hospital stay, and resulted in less complication after surgery, patients who underwent traditional, open surgery lived longer free of disease and their overall survival increased compared to those treated with minimally invasive surgery (see Table 6). These data are helping both surgeons and patients to make informed decisions to opt for traditional surgery. According to a new report the use of minimally invasive surgery has decreased from 58 percent to 43 percent in the 18 months since the publication of the aforementioned clinical trial (421)Lewicki PJ, Basourakos SP, Qiu Y, et al. Effect of a Randomized, Controlled Trial on Surgery for Cervical Cancer. N Engl J Med. 2021;384(17).. These evidence-based changes in clinical practice also underscore the iterative nature of the medical research cycle to improve outcomes for cancer patients as new evidence accumulates (see Figure 16).
Improvements in Radiation-based Approaches for Cancer Care
Radiotherapy uses high energy rays or particles to control the growth of and/or eradicate cancer cells by damaging their DNA. Discovery of X-rays in 1895 allowed visualization of internal organs at low doses. A year later, the effective use of X-rays at high doses to treat a breast cancer patient firmly established radiotherapy as the second pillar of cancer treatment (398)Gianfaldoni S, Gianfaldoni R, Wollina U, Lotti J, Tchernev G, Lotti T. An overview on radiotherapy: From its history to its current applications in dermatology. Open Access Maced J Med Sci. 2017;5(4 Special Issue GlobalDermatology).(see Figure 19). Today, about 50 percent of all cancer patients in the United States receive radiotherapy as part of their treatment regimens. The number of cancer survivors who have received radiotherapy is projected to increase from 3.38 million in 2020 to 4.17 million in 2030 (422)Bryant AK, Banegas MP, Martinez ME, Mell LK, Murphy JD. Trends in radiation therapy among cancer survivors in the United States, 2000-2030. Cancer Epidemiol Biomarkers Prev. 2017;26(6)..
There are many types and uses of radiotherapy (see sidebar on Using Radiation in Cancer Treatment). However, it is important to note that radiotherapy may also have harmful side effects, partly because of the radiation-induced damage to healthy organs surrounding the tumor tissue. Researchers are continuously working on making radiotherapy safer and more effective and also designing novel radiotherapeutics (alone or in combination) to target more cancer types and benefit more patients. One area of rapid development is the use of AI to enhance radiotherapy and the integration of such improved approaches into clinical practice to increase efficacy and reduce toxicity from these treatments (423)El Naqa I. Prospective clinical deployment of machine learning in radiation oncology. Nat Rev Clin Oncol. Published online 2021..
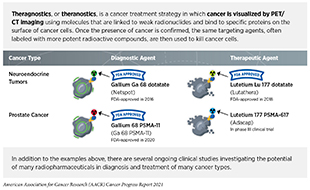
Imaging Prostate Cancer More Clearly
Prostate cancer is the most common type of cancer in men in the United States, with more than two men estimated to be diagnosed every minute in 2021 (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. It is also the second deadliest cancer in men behind only lung cancer. Prostate cancer that is confined to the prostate is usually treated with surgery or radiation therapy. The more precise a patient’s diagnosis, the easier it is for a health care provider to tailor the treatment to ensure that it is as effective and safe as possible. Among the tools physicians use to make cancer diagnoses is positron emission tomography–computed tomography (PET–CT or PET), a form of imaging that can help physicians precisely locate the position of a patient’s cancer within his body and determine the extent to which the cancer may have spread.
Before a PET scan, patients are injected with a radioactive imaging agent. The PET scan detects where in the body the radioactive agent accumulates. In December 2020, FDA approved the agent Gallium-68 PSMA-11 (Ga 68 PSMA-11) as the first molecule that enables the PET imaging of recurrent prostate cancer in men by binding to the prostate-specific membrane antigen (PSMA). PSMA is a protein that is present in abundance on the surface of more than 90 percent of primary and metastatic prostate cancer cells. Ga 68 PSMA-11 contains a short peptide sequence that binds to PSMA and is also attached to Ga 68 radionuclide to enable imaging. When the short peptide binds to PSMA, radiation emitting from radionuclide can be imaged using PET. Clinicians are able to use this information to decide which patient should receive surgery and spare others from unnecessary surgical procedures.
Findings from the two clinical trials that FDA used to approve Ga 68 PSMA-11 indicate that detection of prostate cancers using this approach may help physicians make the best treatment decisions for patients. In one study, prostate cancer patients who were considered at high risk of metastasis, as confirmed by biopsy, underwent PET imaging with Ga 68 PSMA-11 prior to surgical removal of the prostate gland and nearby lymph nodes present in the pelvis. Following surgery, pathological analysis of the removed lesions confirmed that patients who had positive readings on Ga 68 PSMA-11 PET in the pelvic lymph nodes were likely to have metastatic prostate cancer.
Prostate specific antigen (PSA) is a secreted biochemical marker that is used to screen individuals for prostate cancer. In prostate cancer patients who have received treatment, PSA is used for predicting recurrence of the disease. In another clinical trial 635 patients who had rising serum PSA levels after initial prostate cancer treatment with surgery or radiotherapy, underwent a single Ga 68 PSMA-11 PET scan. Seventy-four percent of patients had at least one positive lesion detected by Ga 68 PSMA-11. Among patients with positive PET readings, prostate cancer recurrence or metastasis was definitively confirmed in more than 90 percent of cases using pathological tests (424)Lawhn-Heath C, Flavell RR, Behr SC, et al. Single-center prospective evaluation of 68Ga-PSMA-11 PET in biochemical recurrence of prostate cancer. Am J Roentgenol. 2019;213(2).(425)Hope TA, Aggarwal R, Chee B, et al. Impact of 68Ga-PSMA-11 PET on management in patients with biochemically recurrent prostate cancer. J Nucl Med. 2017;58(12).(426)Fendler WP, Calais J, Eiber M, et al. Assessment of 68Ga-PSMA-11 PET Accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial. In: JAMA Oncology. Vol 5. ; 2019.(427)Calais J, Ceci F, Eiber M, et al. 18F-fluciclovine PET-CT and 68Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial. Lancet Oncol. 2019;20(9).(428)Calais J, Fendler WP, Eiber M, et al. Impact of 68 Ga-PSMA-11 PET/CT on the management of prostate cancer patients with biochemical recurrence. J Nucl Med. 2018;59(3).. Thus, Ga 68 PSMA-11 PET can accurately detect sites of recurrent or metastatic prostate cancer, thereby providing important information that may impact clinical care.
In May 2021, FDA approved another radioactive agent, piflufolastat F 18 (Pylarify), that also targets PSMA to detect prostate cancer lesions that can be imaged by PET. Like Ga 68 PSMA-11, piflufolastat F 18 is a short peptide attached to a radionuclide and is administered in the form of an intravenous injection. Knowledge gleaned from the procedure can be used to make individualized informed decisions about the course of treatment.
FDA approval was based on results from two clinical trials: the first in which patients who already had confirmed prostate cancer as detected by biopsy were subjected to piflufolastat F 18 injection followed by PET imaging, and the second in which patients who had elevated levels of PSA following initial treatment with surgery or radiation were given the piflufolastat F 18 injection followed by PET imaging. In both trials, the piflufolastat F 18-based PET imaging detected the presence of metastatic prostate cancer with high accuracy.
Together, the approvals of Ga 68 PSMA-11 and piflufolastat F 18 are anticipated to help certain patients with prostate cancer avoid unnecessary surgery and undergo a treatment regimen that is tailored for their specific situation.
Detecting Neuroendocrine Tumors with High Accuracy
Neuroendocrine tumors (NET) are cancers that arise in a type of cells in the body, called neuroendocrine cells, that have properties of both nerve and hormone-producing cells and perform specific functions, such as regulating blood flow (429)Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia (United States). 2017;19(12).. NET are considered rare, with an estimated 12,000 people in the United States diagnosed each year (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Because neuroendocrine cells are located throughout the body and perform different functions, the outcome and survival rates for patients vary depending on the type of NET, the tissue of origin, and the feasibility of surgical removal.
In September 2020, FDA approved copper Cu 64 dotatate (Detectnet), to detect certain types of NET. Copper Cu 64 dotatate binds to somatostatin receptors, proteins found in high abundance on the surface of malignant neuroendocrine cells. Copper 64 (Cu 64) is a positron emitting radionuclide, allowing PET imaging of NET. Approval was based on findings from two clinical studies. One study prospectively evaluated 63 participants, of which 42 patients had known or suspected NET as determined by histology, conventional imaging, and/or clinical evaluation. Copper Cu 64 dotatate detected NETs with 91 percent accuracy, as evaluated by three independent oncologists. The second study was a retrospective analysis of published data collected from 112 patients with known history of NET and showed similar performance by copper Cu 64 dotatate. The clinical benefit offered by high accuracy of detecting NET using copper Cu 64 dotatate will guide clinicians in developing a personalized treatment approach for NET patients.
Advances in Treatment with Cytotoxic Chemotherapy
Cytotoxic chemotherapy—use of chemicals to kill cancer cells—remains the backbone of cancer treatment for many patients. First introduced as a pillar of cancer treatment in the early to mid-20th century, use of cytotoxic chemotherapy is continually evolving to minimize its potential harms to cancer patients, while maximizing its benefits (399)DeVita VT, Chu E. A history of cancer chemotherapy. Cancer Res. 2008;68(21):8643-8653..
Reducing the Risk of Blood Cancer Recurrence After Initial Treatment
Acute myeloid leukemia (AML) is a type of blood cancer. It is estimated to be diagnosed in more than 20,000 Americans in 2021 (4)Surveillance, Epidemiology, and End Results (SEER) Program.. Patients with AML undergo intensive first-line chemotherapy to eradicate cancer cells. After the initial chemotherapy, stem cell transplantation is often required to replenish blood-forming cells. Some AML patients need additional intravenous administration of chemotherapeutic agents to prevent recurrence of the disease. Both procedures require a hospital visit and/or stay (431)Kantarjian H, Kadia T, DiNardo C, et al. Acute myeloid leukemia: current progress and future directions. Blood Cancer J. 2021;11(2)..
Researchers are continuously improving the formulation of cytotoxic chemotherapeutics to make them more effective at lower doses, as well as more convenient to administer. In September 2020, FDA approved a new formulation of azacitidine (Onureg) as a maintenance treatment for adults with newly diagnosed AML who had achieved complete remission after intensive chemotherapy. Azacitidine is a routinely used chemotherapeutic drug that is typically injected under the skin or into a vein by a medical professional in a medical facility. The newly approved formulation is in a tablet form that allows for convenient dosing and permits easier delivery of azacitidine as a maintenance therapeutic. The clinical trial evaluating safety and efficacy of the new formulation found that once daily oral administration of azacitidine increased the life spans of AML patients by nearly one year compared to those patients who only received placebo (432)Wei AH, Döhner H, Pocock C, et al. Oral Azacitidine Maintenance Therapy for Acute Myeloid Leukemia in First Remission. N Engl J Med. 2020;383(26).. The drug also reduced the risk of relapse by 35 percent compared to a placebo without compromising health-related quality of life. The approved formulation, which is a result of more than a decade of research and 13 preclinical and clinical studies, makes azacitidine the first oral chemotherapeutic for maintenance therapy in AML patients who are in complete remission (433)Acute Myeloid Leukemia News. FDA approves oral chemotherapy onureg for newly diagnosed AML patients in remission. 2020 Sep 3.. This approval will especially benefit those AML patients who are not able to complete intensive curative therapy, such as stem cell transplantation.
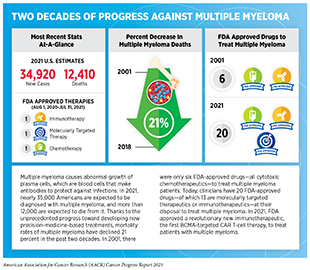
Effectively Delivering Cytotoxic Drugs to Kill Multiple Myeloma Cells
Multiple myeloma is one of the most diagnosed blood cancers in the United States (4)Surveillance, Epidemiology, and End Results (SEER) Program.. Over the last two decades, there has been unprecedented progress toward developing new precision medicine-based treatments for multiple myeloma (see sidebar on Two Decades of Progress Against Multiple Myeloma). Despite the advances, many patients develop resistance to treatment over time and then the disease returns.
Recurring or relapsed multiple myeloma is particularly challenging to treat because patients with recurring or relapsed multiple myeloma often develop resistance to available treatments. In February 2021, FDA approved melphalan flufenamide (Pepaxto), a first-in-class hybrid drug. Melphalan flufenamide combines a potent cytotoxic agent with a peptide that helps rapid uptake of the drug by myeloma cells and quickly releases the cytotoxic agent once inside the cells (435)Wickström M, Nygren P, Larsson R, et al. Melflufen – A peptidase-potentiated alkylating agent in clinical trials. Oncotarget. 2017;8(39).. The high concentration of the above cytotoxic drug kills multiple myeloma cells, and this approach has been effective in treating patients who have developed resistance to other types of treatment. Melphalan flufenamide was approved in combination with dexamethasone, a commonly used steroid with anti-inflammatory and immunosuppressive effects, for adult patients with relapsed or refractory multiple myeloma who have received at least four prior treatments and whose disease no longer responds to at least one proteasome inhibitor, one immunomodulatory agent, or one CD-38 directed monoclonal antibody. The approval was based on results from an ongoing clinical trial in which nearly 30 percent of the participating multiple myeloma patients, who had developed resistance to other treatments, responded to melphalan flufenamide and had an overall survival of nearly a year (436)Richardson PG, Oriol A, Larocca A, et al. Melflufen and dexamethasone in heavily pretreated relapsed and refractory multiple myeloma. J Clin Oncol. 2021;39(7).. A continued evaluation of patients’ response to the drug will be important to further improve overall outcome.
Advances in Treatment with Molecularly Targeted Therapy
Advances in precision medicine, fueled by discovery science, are providing a deeper understanding of the numerous genetic mutations that drive cancer development and are thus offering clinicians a new arsenal of molecularly targeted therapeutics against cancer. As a result, cancer patients now have many treatment options available that are specific to the genetic changes driving their cancer or based on the characteristics of their cancer type. Importantly, therapeutics directed to the molecules influencing cancer cell multiplication and survival target the cells within a tumor more precisely than cytotoxic chemotherapeutics which target all rapidly dividing cells, thereby limiting damage to healthy tissues. The greater precision of molecularly targeted therapeutics tends to make them more effective and less toxic than cytotoxic chemotherapeutics. Thus, molecularly targeted therapeutics are not only saving the lives of cancer patients, but are also leading to a higher quality of life for cancer survivors after treatment.
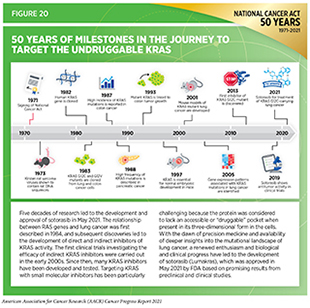
Between August 1, 2020 and July 31, 2021—the 12-month period covered in this report—FDA has approved 10 new anticancer therapeutics that are directed against particular molecules or genetic mutations (see Table 5). A significant breakthrough in molecularly targeted therapeutics covered in this report is the FDA approval of sotorasib (Lumakras) for the treatment of certain patients with lung cancer. Sotorasib is a molecularly targeted therapeutic specifically developed to target an altered from of KRAS that is produced by the G12C mutation, one of the most common non–small cell lung cancer-associated mutations and previously considered an undruggable target (see section on New Wave of Innovation to Aim at Cancer’s Most Intractacble Targets).
Additionally, FDA also expanded the use of five previously approved molecularly targeted therapeutics to treat new types of cancer. These expansions included treatment of anaplastic large-cell lymphoma (ALCL) patients with crizotinib (Xalkori), a molecularly targeted therapeutic first approved to treat lung cancer with alterations in the ALK gene. The experimental use of crizotinib for the treatment of ALCL was first highlighted in the AACR Cancer Progress Report 2014 through the experience of Zachary (Zach) Witt, a nine-year-old at the time, who participated in the clinical trial testing crizotinib (129)Arteaga CL, Adamson PC, Engelman JA, et al. AACR Cancer Progress Report 2014. Clin Cancer Res. 2014;20(19).. The inspiring journey of Zach, now a 16-year-old high school student, underscores how discovery science drives clinical breakthroughs to save and improve the lives of cancer patients.
A New Breakthrough in Treating Lung Cancer
One of the most significant advances in cancer precision medicine in the 12 months covered in this report was the FDA approval of sotorasib. Sotorasib is the first ever molecularly targeted therapeutic designed to target the KRAS G12C mutation, one of the most frequent genetic alterations found in NSCLC patients. The FDA also approved a companion diagnostic (see Companion Diagnostics), called the Guardant Health-developed Guardant360 CDx test, to help identify patients with NSCLC carrying the KRAS G12C mutation.
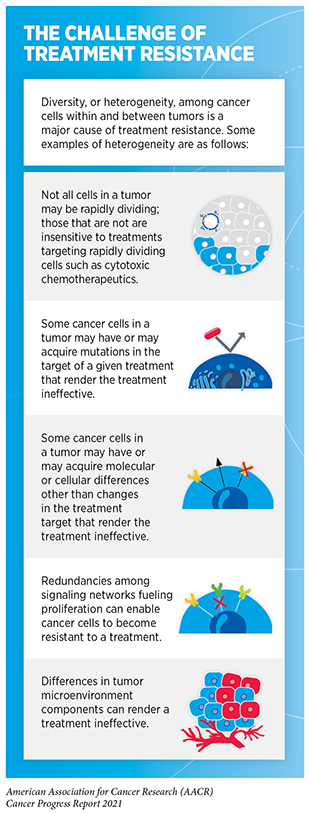
Remarkable progress has been made toward prevention and treatment of lung cancer in the past five decades (see Landmark Discoveries Fueling Advances in Lung Cancer Diagnostics and Treatment). Yet lung cancer remains the third most diagnosed and the deadliest cancer in the United States, with 27 new diagnoses and 15 deaths estimated every hour in 2021 (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. The NSCLC subtype of lung cancer constitutes about 84 percent of all lung cancers, and approximately 25 percent of NSCLC patients carry mutations in KRAS, an essential protein needed for growth and survival of normal lung cells (437)Uprety D, Adjei AA. KRAS: From undruggable to a druggable Cancer Target. Cancer Treat Rev. 2020;89.. For early-stage NSCLC, surgery is the standard treatment, sometimes with chemotherapy, alone or in combination with radiation therapy. Advanced-stage NSCLC is usually treated with chemotherapy and/or immunotherapy. Unfortunately, NSCLC patients who harbor KRAS mutations develop resistance to other types of treatments, and only 25 percent of these patients live five years or more after diagnosis (see sidebar on The Challenge of Treatment Resistance)(438)Ghimessy A, Radeczky P, Laszlo V, et al. Current therapy of KRAS-mutant lung cancer. Cancer Metastasis Rev. 2020;39(4)..
The FDA approved sotorasib (Lumakras) for adult NSCLC patients with locally advanced or metastatic disease, whose tumors harbor the KRAS G12C mutation, a genetic alteration more frequently found in former or current smokers (439)Dogan S, Shen R, Ang DC, et al. Molecular epidemiology of EGFR and KRAS mutations in 3,026 lung adenocarcinomas: Higher susceptibility of women to smoking-related KRAS-mutant cancers. Clin Cancer Res. 2012;18(22).. The approval of sotorasib was based on a phase II clinical trial (440)Skoulidis F, Li BT, Dy GK, et al. Sotorasib for Lung Cancers with KRAS p.G12C Mutation . N Engl J Med. 2021;384(25).. Treatment with sotorasib shrank tumors in over 37 percent of NSCLC patients who had responded poorly to previous treatment with either chemotherapy or immunotherapy. Importantly, responses lasted more than 11 months, and progression -free survival(see Table 6), a measure of how long cancer is held in check, was almost seven months. Even with relatively modest benefits, these responses were roughly two times higher compared to historical results achieved through standard chemotherapy regimens and mark a significant advance for the treatment of patients with KRAS-mutated lung cancer, for whom there are no good options after initial treatment. Developing effective therapeutics that target KRAS has been a daunting challenge and discoveries over the past five decades have fueled the development of sotorasib (Figure 20). Approval of sotorasib and other KRAS inhibitors that are progressing from the bench to the clinic not only brings hope for NSCLC patients, such as Steve Castellaw, but it also holds future promise for treating other KRAS-mutated malignancies that include pancreatic and colorectal cancers.
Targeting Protein Kinases for Treatment of Solid Tumors
In addition to the landmark approval of sotorasib, in the 12 months covered in this report FDA also approved three new molecularly targeted therapeutics—amivantamab-vmjw (Rybrevant), pralsetinib (Gavreto), and tepotinib (Tempetko)—for the treatment of lung cancers that harbor certain alterations in the EGFR, RET, or MET genes, respectively. EGFR, RET, and MET belong to a family of proteins called receptor tyrosine kinases which are located on the surface of cancer cells and play a critical role in the development and progression of many cancer types.
In May 2021, FDA approved amivantamab-vmjw for adult patients with locally advanced or metastatic NSCLC, whose cancer continued to progress after chemotherapy and who have certain alterations in the EGFR gene (insertion mutations in exon 20). The FDA also approved the Guardant360 CDx liquid biopsy test as a companion diagnostic for amivantamab-vmjw to identify patients who have the exon 20 insertion mutant forms of the EGFR gene.
Patients with NSCLC whose tumors harbor insertion mutations in the region exon 20 of the EGFR gene do not respond well to EGFR-targeted therapeutics, such as osimertinib, and generally have poor prognosis (441)Remon J, Hendriks LEL, Cardona AF, Besse B. EGFR exon 20 insertions in advanced non-small cell lung cancer: A new history begins. Cancer Treat Rev. 2020;90.. Amivantamab-vmjw is a first-in-class bispecific antibody approved to treat aggressive forms of NSCLC. Unlike molecularly targeted therapeutics such as osimertinib that work by inhibiting the function of EGFR, amivantamab-vmjw binds to two different receptor tyrosine kinase proteins—EGFR and MET—present on the surface of lung cancer cells and disrupts EGFR and MET functions through blocking ligand binding and/or degradation of EGFR and MET proteins. The presence of EGFR and MET on the surface of tumor cells also allows for targeting of these cells for destruction through antibody-dependent cellular cytotoxicity (ADCC) (442)Neijssen J, Cardoso RMF, Chevalier KM, et al. Discovery of amivantamab (JNJ-61186372), a bispecific antibody targeting EGFR and MET. J Biol Chem. 2021;296.. The FDA decision was based on results from a phase I clinical trial showing that amivantamab-vmjw significantly reduced tumors in 40 percent of the patients. Moreover, these responses lasted at least six months in the majority of patients who were sensitive to amivantamab-vmjw. These encouraging results, and the approval of amivantamab-vmjw, provide a new treatment option for patients with a debilitating form of lung cancer.
In February 2021, FDA approved the targeted therapy tepotinib for treating certain patients with NSCLC. Tepotinib targets an aberrant form of the protein MET, which arises from a genetic alteration known as exon 14 skipping in the MET gene found in approximately 3-4 percent of NSCLC patients (443)Socinski MA, Pennell NA, Davies KD. MET Exon 14 Skipping Mutations in Non–Small-Cell Lung Cancer: An Overview of Biology, Clinical Outcomes, and Testing Considerations . JCO Precis Oncol. 2021;(5).). This alteration is observed in many cancer types (such as lung, thyroid, colorectal, ovarian, breast, and pancreatic cancer) and leads to the overactivation of the MET protein, which causes uncontrolled growth of cancer cells (444)Comoglio PM, Trusolino L, Boccaccio C. Known and novel roles of the MET oncogene in cancer: A coherent approach to targeted therapy. Nat Rev Cancer. 2018;18(6).. NSCLC patients with MET alterations have limited treatment options and a poor clinical outcome. The FDA approved tepotinib for NSCLC patients with advanced or metastatic disease harboring the exon 14 skipping alterations in MET based on results from a phase II clinical trial (445)Paik PK, Felip E, Veillon R, et al. Tepotinib in Non–Small-Cell Lung Cancer with MET Exon 14 Skipping Mutations . N Engl J Med. 2020;383(10).. More than 40 percent of NSCLC patients with advanced or metastatic disease who received tepotinib had shrinkage of their tumors and had sustained response to the treatment for nearly one year. Continued follow-up of NSCLC patients treated with tepotinib will be necessary to establish long-term clinical benefit.
Pralsetinib is designed to treat patients with lung cancer who harbor certain genetic alterations in RET, a protein necessary for growth of normal lung cells. While the activity of RET protein is tightly regulated in normal cells, various mutant forms of the RET gene produce hyperactive proteins in cancer cells and result in uncontrolled cell growth. Mutant RET forms found in lung and other cancers include chromosomal translocations that result in fusion genes, missense mutations, and insertions and deletions (446)Ding SJ, Wang R, Peng SL, et al. Targeted therapies for RET-fusion cancer: Dilemmas and breakthrough. Biomed Pharmacother. 2020;132.. Cancer patients with altered RET proteins (such as lung and thyroid cancer patients) have limited treatment options and poor survival. In September 2020, FDA approved the molecularly targeted therapeutic pralsetinib for the treatment of NSCLC patients harboring alterations in RET proteins. Findings from a phase I/II basket clinical trial (see sidebar on Types of Clinical Trials) that informed the FDA decision showed a significant reduction in tumor size in almost 60 percent of NSCLC patients treated with pralsetinib and complete responses in nearly six percent of the treated patients (447)Gainor JF, Curigliano G, Kim D-W, et al. Pralsetinib for RET fusion-positive non-small-cell lung cancer (ARROW): a multi-cohort, open-label, phase 1/2 study. Lancet Oncol. 2021;22(7)..
According to the most recent estimates, about 44,280 new cases of thyroid cancer will be diagnosed in the United States in 2021; one third of these cases will be among AYA (ages 15 to 39) (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Thyroid cancer has many subtypes, the most common of which is called papillary thyroid cancer. Papillary thyroid cancer, which constitutes up to 80 percent of all thyroid cancer cases, develops from glandular epithelial cells that normally produce the essential iodine-containing thyroid hormones (448)Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. 2016;12(11).. Approximately 10-20 percent of people with papillary thyroid cancer have RET fusion-positive tumors, and roughly 90 percent of patients with advanced medullary thyroid cancer, a less common form of thyroid cancer, carry RET mutations (449)Salvatore D, Santoro M, Schlumberger M. The importance of the RET gene in thyroid cancer and therapeutic implications. Nat Rev Endocrinol. 2021;17(5).. Traditionally, patients with RET-altered thyroid cancers are treated with nonselective therapies, with only a modest efficacy and significant side effects. Promising results from the same basket trial that showed the efficacy of pralsetinib for patients with NSCLC harboring RET alterations prompted FDA to expand the use of pralsetinib for treatment of patients with thyroid cancer. In December 2020, pralsetinib was approved for treatment of adult and pediatric patients 12 years of age and older with advanced or metastatic medullary thyroid cancer (MTC) harboring alterations in the RET protein who require systemic therapy or patients with RET fusion-positive thyroid cancer who require systemic therapy, and who have developed resistance to treatment with radioactive iodine. Pralsetinib demonstrated durable clinical activity, as measured by tumor shrinkage among other parameters, in thyroid cancer patients with or without prior therapy, regardless of what type of RET genetic alteration was present in tumors. Almost 80 percent of patients who responded to the treatment experienced a response lasting for six months or more (450)Kim J, Bradford D, Larkins E, et al. FDA Approval Summary: Pralsetinib for the Treatment of Lung and Thyroid Cancers With RET Gene Mutations or Fusions . Clin Cancer Res. Published online 2021..
In May 2021, FDA granted accelerated approval to infigratinib (Truseltiq) for adults with locally advanced or metastatic bile duct cancer, harboring alterations (fusion or other rearrangement) in the tyrosine kinase protein fibroblast growth factor receptor 2 (FGFR2), that had been previously treated and could not be removed surgically. The FDA also approved a companion diagnostic test for selection of patients with FGFR2 fusion or other rearrangement for treatment with infigratinib. While rare—roughly 8,000 cases diagnosed in the United States annually—the 5-year relative survival rate for metastatic bile duct cancer (also known as cholangiocarcinoma) is only two percent (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. More than seven percent of patients with bile duct cancer harbor alterations in FGFR proteins (451)Wang J, Xing X, Li Q, et al. Targeting the FGFR signaling pathway in cholangiocarcinoma: promise or delusion? Ther Adv Med Oncol. 2020;12.. Infigratinib selectively binds to and inhibits the activities of FGFR1, 2, and 3, and induces cancer cell death by blocking tumor cell proliferation (452)Casadei C, Dizman N, Schepisi G, et al. Targeted therapies for advanced bladder cancer: new strategies with FGFR inhibitors. Ther Adv Med Oncol. 2019;11.. Efficacy of infigratinib was determined in a phase II clinical trial. Infigratinib was given to 108 bile duct cancer patients. Among the 23 patients whose tumor shrank substantially with the treatment, 8 patients maintained the response for 6 months or more (453)Makawita S, K Abou-Alfa G, Roychowdhury S, et al. Infigratinib in patients with advanced cholangiocarcinoma with FGFR2 gene fusions/translocations: The PROOF 301 trial. Futur Oncol. 2020;16(30).. Infigratinib is only the second FGFR-specific inhibitor approved by FDA, after erdafitinib (Balversa) that was approved in April 2019 to treat certain patients with bladder cancer, and covered in the AACR Cancer Progress Report 2019 (454)Sengupta R, Honey K. AACR cancer progress report 2019: Transforming lives through innovative cancer science. Clin Cancer Res. 2019;25(18).. Additional clinical studies will be necessary to determine whether infigratinib can also treat the more than seven percent of patients with cancer types, such as cervical, colon, endometrial, and esophageal cancers, whose tumors also harbor alterations in FGFR (455)Helsten T, Elkin S, Arthur E, Tomson BN, Carter J, Kurzrock R. The FGFR landscape in cancer: Analysis of 4,853 tumors by next-generation sequencing. Clin Cancer Res. 2016;22(1)..
Inhibiting the Blood Supply to Tumors
Angiogenesis is the formation of a network of blood vessels that supplies nutrients to newly formed tissues during normal development. In 1970, researchers first posited that tumors secrete factor(s) to drive blood vessel formation in and around the tumor, thus establishing a “supply chain” of nutrients for tumors to grow and spread (456)Sherwood LM, Parris EE, Folkman J. Tumor Angiogenesis: Therapeutic Implications. N Engl J Med. 1971;285(21).. Fifty years of discovery science since then have led to the identification of key molecules that are necessary for tumor angiogenesis. Researchers have leveraged this knowledge to develop molecules, sometimes called antiangiogenic drugs or angiogenesis inhibitors, that inhibit tumor angiogenesis (Figure 21)(457)Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77(9).. Clinical breakthroughs stemming from this research are highlighted by the development and FDA approval of 12 angiogenic inhibitors—including tivozanib (Fotivda) approved in March 2021—to treat a wide range of solid tumors.
Renal cell carcinoma (RCC) is the most common type of kidney cancer. An estimated 76,080 new cases of kidney cancer will be diagnosed in the United States in 2021, and nine out of 10 will be RCC cases (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Despite the availability of an array of treatment options, patients with advanced RCC, which develops in the lining of small tubes in kidneys, have a poor 5-year survival rate of only 13 percent (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. In March 2021, FDA approved tivozanib for adult patients with RCC whose disease had relapsed or became nonresponsive following two or more systemic therapies. Tivozanib is a potent inhibitor of vascular endothelial growth factor receptors (VEGFR), which play an essential role in tumor angiogenesis (457)Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell Mol Life Sci. 2020;77(9).. The phase III clinical trial evaluating efficacy of tivozanib compared the responsiveness of RCC patients treated with tivozanib with those treated with sorafenib (Nexavar), another molecularly targeted therapeutic that inhibits angiogenic as well as other cancer-causing proteins and has been approved by FDA to treat RCC (458)Escudier B, Worden F, Kudo M. Sorafenib: key lessons from over 10 years of experience. Expert Rev Anticancer Ther. 2019;19(2).. Tivozanib treatment increased disease-free survival by nearly two months (5.6 months) when compared to sorafenib (3.9 months). The objective response rate—a measure of how well a patient responds to a treatment as determined by the reduction in size of the tumor after the treatment, among other parameters—more than doubled for RCC patients treated with tivozanib (459)Szarek M, Needle MN, Rini BI, et al. Q-TWiST Analysis of Tivozanib Versus Sorafenib in Patients With Advanced Renal Cell Carcinoma in the TIVO-3 Study. Clin Genitourin Cancer. Published online 2021..
Delivering Cytotoxic Agents Precisely to Cancer Cells
Researchers are continuously developing precise strategies that selectively target cancer cells for eradication without harming the normal tissue. Antibody-drug conjugates (ADCs), which use antibodies to deliver an attached toxin specifically to cancer cells, constitute one such strategy of precision anticancer therapeutics (see Figure 22). The antibody used in an ADC is directed against a protein that is overexpressed on the surface of cancer cells. The choice of cytotoxic agent is informed by the cancer type as well as other pharmacological considerations, such as the effective dose of the toxin needed to kill cancer cells and how stable the toxin is inside the body. Once antibody binds to its target on the cancer cell surface, the ADC is taken up by the cell where it releases the cytotoxic drug, which ultimately kills the cancer cell (460)Khongorzul P, Ling CJ, Khan FU, Ihsan AU, Zhang J. Antibody-drug conjugates: A comprehensive review. Mol Cancer Res. 2020;18(1).. This approach minimizes the side effects of the cytotoxic agent compared to a traditional systemic delivery.
The past two decades have seen remarkable progress against multiple myeloma, with 20 therapies available today and a declining mortality rate from the cancer (see sidebar on Two Decades of Progress Against Multiple Myeloma). Most patients with multiple myeloma respond well to the initial treatment regimen. Unfortunately, the disease often relapses and patients become resistant to currently available therapies (461)Robak P, Drozdz I, Szemraj J, Robak T. Drug resistance in multiple myeloma. Cancer Treat Rev. 2018;70.. Up until 2021, the antibody-based molecularly targeted therapeutics approved by FDA to treat multiple myeloma were directed against one of two proteins, CD38 [daratumumab (Darzalex) and isatuximab-irfc (Sarclisa)] or SLAMF7 [elotuzumab (Empliciti)], that are found on the surfaces of normal plasma cells and are overexpressed in multiple myeloma cells.
Approval of belantamab mafodotin-blmf (Blenrep) marks a significant therapeutic milestone—and is designated a first-in-class drug by FDA because it is directed against a different cell surface protein, B-cell maturation antigen (BCMA), which is present in abundance on multiple myeloma cells (462)Yu B, Jiang T, Liu D. BCMA-targeted immunotherapy for multiple myeloma. J Hematol Oncol. 2020;13(1).. Using BCMA to deliver a cytotoxic agent to multiple myeloma cells raises hope for patients who have developed resistance to anti-CD38-antibody-based treatments. In belantamab mafodotin-blmf, the anti-BCMA antibody is conjugated with an inhibitor of microtubules, which are a component of the cellular cytoskeleton and have a number of functions including cell division. Thus, inhibition of microtubules prevents cells from multiplying and ultimately results in cell death. The clinical trial investigating the efficacy of belantamab mafodotin-blmf only included multiple myeloma patients who had received three or more prior treatments and had stopped responding to a proteasome inhibitor, an immunomodulatory agent, and an anti-CD38 antibody therapy. Nearly one third of all treated patients responded to belantamab mafodotin-blmf, and 73 percent of patients who responded showed a response duration of six months or more (463)Lonial S, Lee HC, Badros A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21(2).. Importantly, the use of BCMA to direct cytotoxic agents or engineered T cells to cancer cells (see Engineering Immune Cells to Fight Cancer) provides new options for targeting multiple myeloma with anticancer therapeutics.
Another ADC approved by FDA during the 12 months covered in this report is loncastuximab tesirine-lpyl (Zynlonta). Loncastuximab tesirine-lpyl comprises an antibody directed against CD19—a protein found in abundance on the surface of cancerous B cells (464)Wang K, Wei G, Liu D. CD19: a biomarker for B cell development, lymphoma diagnosis and therapy. Exp Hematol Oncol. 2012;1(1).—conjugated with a chemotherapeutic alkylating agent that irreversibly binds to DNA and blocks cell division. The FDA approved loncastuximab tesirine-lpyl for adult patients with relapsed or refractory large B-cell lymphoma—including diffuse large B-cell lymphoma (DLBCL)—who have received two or more lines of systemic therapy. DLBCL is the most common type of non-Hodgkin lymphoma (NHL) in the United States, accounting for about one out of every three lymphomas (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. DLBCL is an aggressive NHL that affects a type of white blood cells called B-lymphocytes, and despite recent treatment advances, such as the use of anti-CD20 monoclonal antibody rituximab (Rituxan), approximately 40 percent of patients relapse or show poor response (465)Xiros N, Economopoulos T, Valsami S, Rontogianni D, Fountzilas G, Raptis S. Rituximab in combination with vinorelbine/gemcitabine chemotherapy in patients with primary refractory or early relapsed T cell rich B cell lymphoma: A pilot study. Leuk Res. 2003. Efficacy of loncastuximab tesirine-lpyl was evaluated in 145 adult patients who participated in a phase II clinical trial. Nearly 50 percent of patients responded favorably to treatment with loncastuximab tesirine-lpyl and showed a significant decrease in cancer. Importantly, DLBCL was undetectable in nearly 25 percent of responders for at least 10 months (466)Hamadani M, Radford J, Carlo-Stella C, et al. Final results of a phase 1 study of loncastuximab tesirine in relapsed/refractory B-cell non-Hodgkin lymphoma. Blood. 2021;137(19)..
In January 2021, FDA expanded the use of the ADC fam-trastuzumab deruxtecan-nxki (Enhertu), originally approved in December 2019 for the treatment of metastatic HER2-positive breast cancer (467)Sengupta R, Honey K. AACR Cancer Progress Report 2020: Turning Science into Lifesaving Care. Clin Cancer Res. 2020;26(19)., to treat HER2-positive gastric (stomach) or gastroesophageal junction (GEJ) adenocarcinomas, after they had progressed on trastuzumab therapy. Gastric cancer accounts for about 1.5 percent of all cancer cases in the United States, with an estimated 26,560 new diagnoses in 2021 (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Currently there are no tests for the early detection of gastric cancers among average-risk individuals. As a result, gastric cancer is often diagnosed at an advanced stage when it is difficult to treat and has a very poor 5-year relative survival rate of less than 20 percent (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Roughly 22 percent of gastric cancer patients have tumors with abnormally high levels of the protein HER2, and HER2-overexpression remains an important biomarker for the selection of patients eligible for anti-HER2 targeted therapies (468)Yan M, Schwaederle M, Arguello D, Millis SZ, Gatalica Z, Kurzrock R. HER2 expression status in diverse cancers: review of results from 37,992 patients. Cancer Metastasis Rev. 2015;34(1). (see sidebar on Biomarkers and Their Use in Cancer Science and Medicine). However, in contrast to HER2-positive breast cancer, HER2-targeted treatments did not improve outcomes for patients with gastric cancer whose disease had progressed on trastuzumab treatment in the past (469)Zhao D, Klempner SJ, Chao J. Progress and challenges in HER2-positive gastroesophageal adenocarcinoma. J Hematol Oncol. 2019;12(1).. Treatment of patients with HER2-positive gastric cancer with fam-trastuzumab deruxtecan-nxki increased overall survival by four months compared to patients treated with standard chemotherapy. Furthermore, the objective response rate (see Table 6) was reported in 51 percent of the patients in the trastuzumab deruxtecan group, as compared to 14 percent of those who received chemotherapy(470)Shitara K, Bang Y-J, Iwasa S, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Gastric Cancer. N Engl J Med. 2020;382(25):2419-2430.. Therefore, approval of fam-trastuzumab deruxtecan-nxki is an important advance toward expanding targeted therapy options for gastric cancer patients like Bryan Chagolla.
In the 12 months covered in this report FDA also expanded the use of sacituzumab govitecan-hziy (Trodelvy)—an ADC previously approved to treat locally advanced or metastatic triple-negative breast cancer—for the treatment of locally advanced or metastatic urothelial cancer patients who have been previously treated with standard chemotherapy and at least one checkpoint inhibitor. Seventy-seven percent of patients with locally advanced or metastatic urothelial cancer who responded to the sacituzumab govitecan-hziy treatment showed a decrease in detectable cancer; progression-free survival (see Table 6) was 5.4 months and the median overall survival was nearly 11 months following the treatment (472)Tagawa ST, Balar A V., Petrylak DP, et al. TROPHY-U-01: A Phase II Open-Label Study of Sacituzumab Govitecan in Patients With Metastatic Urothelial Carcinoma Progressing After Platinum-Based Chemotherapy and Checkpoint Inhibitors. J Clin Oncol. Published. An estimated 83,730 Americans—64,280 men and 19,450 women—will be diagnosed with bladder cancer in 2021, and 90 percent of those cases will be urothelial cancer. The relative 5-year survival rate for patients with metastatic urothelial cancer is only 5.5 percent (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Thus, the expansion of sacituzumab govitecan-hziy use to treat metastatic urothelial cancer provides a valuable additional treatment option for these patients.
Collectively, the approval of two new ADCs and expansion of two previously approved ADCs between August 1, 2020 and July 31, 2021 highlights the accelerated innovations in the development of these unique and powerful targeted therapeutics that can transform the lives of many patients with cancer.
Expanding Treatment Options for Patients with Rare Blood Cancers
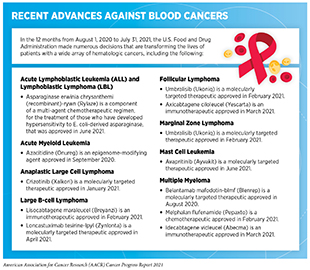
Blood or hematologic cancers arise in the bone marrow where blood is formed, or in cells of the immune system. In the 12 months covered in the report, FDA has made numerous decisions that are transforming the lives of patients with a wide array of blood cancer types (see sidebar on Recent Advances against Blood Cancers). Some of these approvals are expanding treatment options for patients with very rare forms of blood cancers.
Lymphoma is a type of blood cancer that develops when B- or T-cell lymphocytes, the white blood cells that are primarily involved in the body’s adaptive immune system, or less commonly natural killer (NK) cells that are involved in both the innate and adaptive immune response, grow out of control. There are more than 70 different types of lymphoma, ranging from slow growing to highly aggressive forms. The most common type of lymphoma, called non-Hodgkin lymphoma (NHL), accounts for four percent of all cancers in the United States (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. About 85 percent of all NHL originate from B-cell lymphocytes (473)Armitage JO, Gascoyne RD, Lunning MA, Cavalli F. Non-Hodgkin lymphoma. Lancet. 2017;390(10091):298-310.. Recent advances in treatment of NHL have markedly improved survival rates and quality of life for patients (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Although some forms of B-cell NHL, such as follicular lymphoma (FL) and marginal zone lymphoma (MZL), respond well to initial treatments, they remain difficult to cure because many patients develop resistance to the treatment (474)Bojarczuk K, Wienand K, Chapuy B. Molecular classification of large B-cell non-hodgkin lymphoma. Cancer J (United States). 2020;26(4).. Additionally, these lymphomas are rare which can make it challenging for researchers to study and for clinicians to treat these diseases (see sidebar on The Challenges Posed by Rare Cancers).
In February 2021, FDA granted accelerated approval to umbralisib (Ukoniq) for treatment of patients who have relapsed or refractory MZL and have received at least one prior anti-CD20-based therapy. Umbralisib, a selective inhibitor of an enzyme—PI3K delta—which is primarily expressed in tumor cells and helps them grow (475)Nguyen PH, Niesen E, Hallek M. New roles for B cell receptor associated kinases: when the B cell is not the target. Leukemia. 2019;33(3).—was also approved to treat patients with relapsed or refractory FL who have received at least three prior treatments. The decision was based on a randomized phase II trial in which nearly half of the MZL patients treated with umbralisib showed a significant decrease in cancer burden, and about 16 percent of the patients were free of any signs of cancer (476)Fowler NH, Samaniego F, Jurczak W, et al. Umbralisib, a dual PI3Kδ/CK1ε inhibitor in patients with relapsed or refractory indolent lymphoma. In: Journal of Clinical Oncology. Vol 39. ; 2021.(477)Mato AR, Ghosh N, Schuster SJ, et al. Phase 2 study of the safety and efficacy of umbralisib in patients with CLL who are intolerant to BTK or PI3Kδ inhibitor therapy. Blood. 2021;137(20).. For patients with FL, the overall response rate to the treatment was 43 percent and three percent of the patients showed no signs of disease at the end of the treatment. The approval of umbralisib has given hope to patients with otherwise incurable blood cancers.
Another key therapeutic advance in treating a rare form of lymphoma is the expanded use of crizotinib (Xalkori)—originally approved in 2011 to treat certain patients with NSCLC that express an abnormal form of the ALK protein—for treatment of children and young adults who have relapsed or refractory anaplastic large cell lymphoma (ALCL) expressing aberrant forms of the ALK gene. Unlike MZL and FL which are derived from B-cell lymphocytes, ALCL originates from T-cell lymphocytes, and accounts for about two percent of lymphomas. ALCL tends to be fast-growing and accounts for 10 to 20 percent of lymphomas in children and young adults (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. The approval of crizotinib, which is a molecularly targeted therapeutic against ALK and MET proteins, to treat ALK-positive ALCL was based on findings from a phase II clinical trial. Eighty-one percent of patients who participated in the trial no longer showed any signs of the cancer. Of the patients who responded to the treatment, 39 percent maintained such a response for at least six months and 22 percent maintained response for at least a year following treatment (478)Balis FM, Thompson PA, Mosse YP, et al. First-dose and steady-state pharmacokinetics of orally administered crizotinib in children with solid tumors: a report on ADVL0912 from the Children’s Oncology Group Phase 1/Pilot Consortium. Cancer Chemother Pharma. Treatment with crizotinib has transformed the lives of patients such as Zachary (Zach) Witt, who was highlighted in the AACR Cancer Progress Reports in 2014 and 2015 as a participant in the clinical trial evaluating the efficacy of crizotinib for treatment of ALK-positive ALCL patients (129)Arteaga CL, Adamson PC, Engelman JA, et al. AACR Cancer Progress Report 2014. Clin Cancer Res. 2014;20(19).(139)Baselga J, Bhardwaj N, Cantley LC, et al. AACR Cancer Progress Report 2015. In: Clinical Cancer Research : An Official Journal of the American Association for Cancer Research. Vol 21. ; 2015..
In June 2021, FDA approved the molecularly targeted therapeutic avapritinib (Ayvakit) for treating adults with certain aggressive forms of a rare disorder known as advanced systemic mastocytosis. In patients with this disorder, immune cells called mast cells accumulate in internal organs such as the liver, spleen, bone marrow, and small intestine.
Research has shown that most cases of systemic mastocytosis are caused by mutations in the gene that encodes the KIT tyrosine kinase receptor, which is one of the targets of avapritinib. The approval of avapritinib for treating advanced systemic mastocytosis, including in patients with an associated hematological neoplasm and mast cell leukemia, was based on two clinical trial results. The data from the clinical trials showed that in 28 percent of patients all signs and symptoms of cancer disappeared, and, in another 28 percent, there was a reduction in the extent of cancer in the body following treatment with the molecularly targeted therapeutic.
Inhibiting the Progression of Prostate Tumors and Improving Quality of Life
In patients with advanced prostate cancer, the tumors use testosterone and other androgens, hormones naturally produced by the body, to stimulate cell division and metastasis. These patients are typically treated with androgen deprivation therapy (ADT). One class of drugs used in ADT is agonists of gonadotrophin-releasing hormone (GnRH), a hormone that acts on pituitary gland and decreases the production of testosterone. A commonly used GnRH agonist is leuprolide (Lupron), which is given via injection every few months. Leuprolide reduces the production of testosterone, thus starving advanced prostate cancer of the fuel that it needs to grow and spread. A serious side effect of leuprolide (and other ADT drugs) is increased risk of heart attacks and heart failure, highlighting the need of new drugs without harmful effects for prostate cancer patients (479)Crawford ED, Heidenreich A, Lawrentschuk N, et al. Androgen-targeted therapy in men with prostate cancer: evolving practice and future considerations. Prostate Cancer Prostatic Dis. 2019;22(1)..
In December 2020, relugolix (Orgovyx)—a new drug to treat men with advanced prostate cancer—was approved by FDA. Relugolix is a GnRH antagonist, which also acts on the pituitary gland, but blocks testosterone production more directly and rapidly (480)Nakata D, Masaki T, Tanaka A, et al. Suppression of the hypothalamic-pituitary-gonadal axis by TAK-385 (relugolix), a novel, investigational, orally active, small molecule gonadotropin-releasing hormone (GnRH) antagonist: Studies in human GnRH receptor kn. In a large clinical trial, relugolix was more effective at reducing testosterone levels in men with advanced prostate cancer than leuprolide. About 97 percent of men treated with relugolix reached and maintained very low testosterone levels, compared to 89 percent of men who received leuprolide. Unlike patients treated with many other drugs used for ADT, men treated with relugolix also had significantly less serious cardiac issues, and restoration of their testosterone back to normal levels within a few months of stopping therapy (481)Shore ND, Saad F, Cookson MS, et al. Oral Relugolix for Androgen-Deprivation Therapy in Advanced Prostate Cancer. N Engl J Med. 2020;382(23).. Another benefit of relugolix is that it is a tablet that patients can take every day, further minimizing any inconvenience to patients from intramuscular administration. Relugolix is a significant therapeutic advance that is expected to substantially improve the quality of life for patients with advanced prostate cancer.
Advances in Cancer Immunotherapy
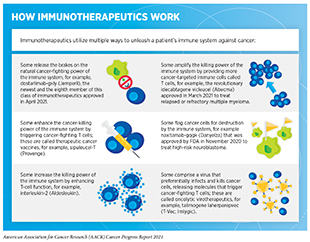
Cancer immunotherapy unleashes the natural ability of a patient’s immune system to fight cancer (482)Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol. 2020;20(11).. More than a century of research indicated that our immune system could detect and destroy cancer cells. Insights gathered in recent decades into functioning of the immune system have also provided the necessary information to weaponize a patient’s immune system against cancer (483)Dobosz P, Dzieciątkowski T. The Intriguing History of Cancer Immunotherapy. Front Immunol. 2019;10.. Knowledge gleaned from these discoveries has allowed for the development of therapeutics, known as immunotherapeutics, that harness the power of the immune system against cancer in multiple ways (see sidebar on How Immunotherapeutics Work).
The remarkable success of a variety of immunotherapeutics in the clinic has firmly established cancer immunotherapy as the fifth pillar of cancer treatment (see Figure 19). This is, in part, because of the durable response to these revolutionary treatments in some patients with metastatic cancer. It is, however, important to note that not all patients who receive immunotherapy have experienced such an incredible response to the treatment (484)Galluzzi L, Chan TA, Kroemer G, Wolchok JD, López-Soto A. The hallmarks of successful anticancer immunotherapy. Sci Transl Med. 2018;10(459).. Furthermore, immunotherapeutics currently approved by FDA treat only a subset of cancer types. Researchers are continuously investigating new and improved strategies to fully realize the potential of immunotherapeutics for all cancers. Numerous ongoing clinical trials are evaluating new and improved immunotherapeutics and testing the use of those we already have against additional types of cancer, alone or in combination with other types of cancer treatments (485)Kubli SP, Berger T, Araujo D V., Siu LL, Mak TW. Beyond immune checkpoint blockade: emerging immunological strategies. Nat Rev Drug Discov. Published online 2021.(486)Keilson JM, Knochelmann HM, Paulos CM, Kudchadkar RR, Lowe MC. The evolving landscape of immunotherapy in solid tumors. J Surg Oncol. 2021;123(3).. One area of active research is the use of NK cells—a type of immune cells that rapidly kill abnormal cells by releasing cytotoxic chemicals—to develop a new class of immunotherapeutics (487)Liu S, Galat V, Galat4 Y, Lee YKA, Wainwright D, Wu J. NK cell-based cancer immunotherapy: from basic biology to clinical development. J Hematol Oncol. 2021;14(1).(488)Miller JS, Lanier LL. Natural killer cells in cancer immunotherapy. Annu Rev Cancer Biol. 2019;3(1).(489)Mujal AM, Delconte RB, Sun JC. Natural Killer Cells: From Innate to Adaptive Features. Annu Rev Immunol. 2021;39.. Several clinical studies have established that the NK cell-based immunotherapeutics are safe for use in humans (490)Tonn T, Schwabe D, Klingemann HG, et al. Treatment of patients with advanced cancer with the natural killer cell line NK-92. Cytotherapy. 2013;15(12).(491)Dolstra H, Roeven MWH, Spanholtz J, et al. Successful transfer of umbilical cord blood CD34+ hematopoietic stem and progenitor-derived NK cells in older acute myeloid leukemia patients. Clin Cancer Res. 2017;23(15).(492)Arai S, Meagher R, Swearingen M, et al. Infusion of the allogeneic cell line NK-92 in patients with advanced renal cell cancer or melanoma: A phase I trial. Cytotherapy. 2008;10(6)., rapidly kill tumor cells (493)Wu SY, Fu T, Jiang YZ, Shao ZM. Natural killer cells in cancer biology and therapy. Mol Cancer. 2020;19(1).(494)Ljunggren HG, Kärre K. In search of the “missing self”: MHC molecules and NK cell recognition. Immunol Today. 1990;11(C). and, importantly, can be developed from stored or “off-the-shelf” NK cells (495)Suck G, Odendahl M, Nowakowska P, et al. NK-92: an ‘off-the-shelf therapeutic’ for adoptive natural killer cell-based cancer immunotherapy. Cancer Immunol Immunother. 2016;65(4).(496)Veluchamy JP, Kok N, van der Vliet HJ, Verheul HMW, de Gruijl TD, Spanholtz J. The rise of allogeneic Natural killer cells as a platform for cancer immunotherapy: Recent innovations and future developments. Front Immunol. 2017;8(MAY).(497)Lupo KB, Matosevic S. Natural killer cells as allogeneic effectors in adoptive cancer immunotherapy. Cancers (Basel). 2019;11(6).(498)Nham T, Poznanski SM, Fan IY, et al. Ex Vivo-expanded Natural Killer Cells Derived from Long-term Cryopreserved Cord Blood are Cytotoxic Against Primary Breast Cancer Cells. J Immunother. 2018;41(2).. Current efforts are focused on improving the ability to expand NK cells and enhance their function (499)Freund-Brown J, Chirino L, Kambayashi T. Strategies to enhance NK cell function for the treatment of tumors and infections. Crit Rev Immunol. 2018;38(2)., as well as genetically modifying NK cells to increase their effectiveness against tumor cells (500)Mantesso S, Geerts D, Spanholtz J, Kučerová L. Genetic Engineering of Natural Killer Cells for Enhanced Antitumor Function. Front Immunol. 2020;11..
Here, we focus on the FDA approvals of new immunotherapeutics and the expansions of the previously approved immunotherapeutics for use against additional types of cancer between August 1, 2020 and July 31, 2021, the 12-months period covered in this report (see Table 5).
Releasing the Brakes on the Immune System
Decades of discovery science have shown that immune cells, called T cells, are naturally capable of destroying cancer cells. We have also learned that some tumor cells have developed ways to escape destruction by T cells. One of the mechanisms by which tumor cells evade elimination by T cells is by expressing high levels of certain proteins that attach to and trigger “brakes” on T cells and stop them from attacking cancers. These brakes are proteins on the surface of T cells and are called immune-checkpoint proteins. Researchers have identified many checkpoint proteins and their binding partners on tumor cells involved in the process of inhibiting T cell activation, three of which—CTLA-4, PD-1, and PD-L1—have proven to be effective targets for drug development (482)Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol. 2020;20(11). (see Figure 23). This knowledge has spurred a new class of therapeutics—called immune checkpoint inhibitors—that can trigger T cells to destroy cancer cells by releasing these brakes (501)Sharma P, Siddiqui BA, Anandhan S, et al. The Next Decade of Immune Checkpoint Therapy. Cancer Discov. 2021;11(4)..
A key advantage of checkpoint inhibitors is their broad utility against cancer, as highlighted by FDA approvals of checkpoint inhibitors to treat multiple types of cancer (see Figure 24). During the 12-month period covered in this report—August 1, 2020 to July 31, 2021—, one of the most significant advances toward realizing the promise of checkpoint inhibitors for treatment of cancer is the FDA approval of a new checkpoint inhibitor, dostarlimab-gxly (Jemperli), to treat metastatic endometrial cancer. During this period, FDA also expanded the use of four previously approved checkpoint inhibitors—cemiplimab-rwlc (Libtayo), nivolumab (Opdivo), pembrolizumab (Keytruda), and ipilimumab (Yervoy)—to treat additional types of cancer. As of July 31, 2021, one or more checkpoint inhibitors have been approved for treating 18 types of cancer and for treating any types of solid tumors that are characterized by certain molecular characteristics, such as microsatellite instability (MSI)–high, DNA mismatch–repair deficiency (dMMR), and tumor mutational burden (TMB)–high.
Endometrial cancer is the most common cancer of the female reproductive organs that develops in the inner lining of the uterus. An estimated 66,570 new cases of endometrial cancer (most common type of uterine cancer) will be diagnosed in 2021 (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. About 75 percent of endometrial cancers are diagnosed at an early stage and are curable with surgery. Women whose cancer continues to advance or returns after initial treatment with chemotherapeutics, however, have limited treatment options (502)Makker V, Green AK, Wenham RM, Mutch D, Davidson B, Miller DS. New therapies for advanced, recurrent, and metastatic endometrial cancers. Gynecol Oncol Res Pract. 2017;4(1).. Approximately 25-30 percent of patients with advanced endometrial cancer also have a specific genetic biomarker, called deficient mismatch repair (dMMR)(503)Bonneville R, Krook MA, Kautto EA, et al. Landscape of Microsatellite Instability Across 39 Cancer Types. JCO Precis Oncol. 2017;(1)., that can be determined by an FDA-approved test.
In April 2021, FDA granted accelerated approval to a new checkpoint inhibitor dostarlimab-gxly for treating patients with recurrent or advanced endometrial cancer that has progressed despite chemotherapy and whose cancers have the dMMR biomarker (see sidebar on Biomarkers and Their Use in Cancer Science and Medicine). Dostarlimab-gxly is a monoclonal antibody that binds to the PD-1 protein—one of the brakes on T cells—and inhibits its activity, thus unleashing the immune system to kill cancer cells. The decision by FDA to approve dostarlimab-gxly was based on results from a basket clinical trial (see sidebar on Types of Clinical Trials). Findings from the trial showed that the tumors either completely disappeared or shrank significantly in more than 40 percent of women who had dMMR recurrent or advanced endometrial cancer and were treated with dostarlimab-gxly. Importantly, the response lasted for six months or more in 93 percent of women who responded to the treatment (504)Oaknin A, Tinker A V., Gilbert L, et al. Clinical Activity and Safety of the Anti-Programmed Death 1 Monoclonal Antibody Dostarlimab for Patients with Recurrent or Advanced Mismatch Repair-Deficient Endometrial Cancer: A Nonrandomized Phase 1 Clinical Tri. While many ongoing clinical studies are investigating the enormous potential of dostarlimab-gxly in treating additional cancer types, it has already transformed the lives of many patients with endometrial cancer, such as Patricia Hawkins.
In October 2020, FDA granted approval to a combination of two checkpoint inhibitors—nivolumab and ipilimumab—as first-line treatment for adult patients with malignant pleural mesothelioma that cannot be removed by surgery. Mesothelioma—although rare, with about 3,000 cases diagnosed each year in the United States—is an aggressive cancer with 5-year relative survival rate of less than 20 percent (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Mesothelioma originates in the thin layer of tissue that covers the majority of internal organs; pleural mesothelioma affects tissue that surrounds lungs (505)Porpodis K, Zarogoulidis P, Boutsikou E, et al. Malignant pleural mesothelioma: Current and future perspectives. J Thorac Dis. 2013;5(SUPPL.4).. Patients with malignant pleural mesothelioma that cannot be surgically removed and those who did not receive any previous anticancer therapy were randomly assigned to receive a combination of nivolumab and ipilimumab or standard chemotherapy for up to 2 years. Overall survival was significantly extended among patients treated with the combination of nivolumab and ipilimumab (18.1 months) compared to those who received chemotherapy (14.1 months). The 2-year overall survival rate (see Table 6) was 41 percent versus 27 percent for patients treated with a combination of the two checkpoint inhibitors versus those who received chemotherapy, respectively(506)Baas P, Scherpereel A, Nowak AK, et al. First-line nivolumab plus ipilimumab in unresectable malignant pleural mesothelioma (CheckMate 743): a multicentre, randomised, open-label, phase 3 trial. Lancet. 2021;397(10272).). This is remarkable progress toward treating a devastating type of cancer and brings the transformative power of immunotherapy to mesothelioma patients, such as Susan Falbo.
Skin cancer is one of the most common cancer types, with an estimated 5.4 million cases diagnosed each year in the United States. Two of the most common forms of skin cancer are called squamous cell carcinoma (SCC), which accounts for about 20 percent of the nonmelanoma skin cancer cases, and basal cell carcinoma (BCC), which makes up 80 percent of the nonmelanoma skin cancer diagnoses (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Both forms originate from two different skin cell types—squamous and basal—that, together with a third type of cells called melanocytes, make up the top layer of skin. The FDA originally approved the immune checkpoint inhibitor cemiplimab-rwlc in September 2018 for treatment of advanced SCC. In February 2021, FDA expanded the use of cemiplimab-rwlc as the first immunotherapy for patients with locally advanced or metastatic BCC who were previously treated with a hedgehog pathway inhibitor (HHI), a type of molecularly targeted therapeutic, or for whom HHI was not appropriate. Approval was based on the findings that 79 percent of locally advanced BCC and all metastatic BCC patients who responded to the treatment maintained their response for at least six months (507)Stratigos AJ, Sekulic A, Peris K, et al. Cemiplimab in locally advanced basal cell carcinoma after hedgehog inhibitor therapy: an open-label, multi-centre, single-arm, phase 2 trial. Lancet Oncol. 2021;22(6)..
In February 2021, cemiplimab-rwlc was also approved as the first line of treatment for patients with advanced NSCLC whose tumors do not have any aberrations in EGFR, ALK or ROS1 proteins and have high expression of PD-L1, one of the proteins on cancer cells that apply the PD-1 brake on T-cells, as determined by an FDA-approved test. With this decision, cemiplimab-rwlc becomes the sixth checkpoint inhibitor approved by FDA for treatment of patients with NSCLC. The assessment was based on encouraging results from a randomized clinical trial comparing the outcomes of advanced NSCLC patients treated with either cemiplimab-rwlc or standard chemotherapy. More patients responded to cemiplimab-rwlc treatment compared to chemotherapy (37 percent versus 21 percent, respectively), and overall survival was increased by nearly eight months (22.1 months versus 14.3 months, respectively)(508)Sezer A, Kilickap S, Gümüş M, et al. Cemiplimab monotherapy for first-line treatment of advanced non-small-cell lung cancer with PD-L1 of at least 50%: a multicentre, open-label, global, phase 3, randomised, controlled trial. Lancet. 2021;397(10274)..
Patients with esophageal or gastroesophageal junction (GEJ) cancer have poor overall survival; only 20 percent of patients diagnosed at any stage of the disease survive five years or more (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Furthermore, findings from a recent analysis show an alarming increase in the incidence of esophageal cancer among those younger than 50 years (108)Codipilly DC, Sawas T, Dhaliwal L, et al. Epidemiology and Outcomes of Young-Onset Esophageal Adenocarcinoma: An Analysis from a Population-Based Database. Cancer Epidemiol Biomarkers Prev. Published online December 2020.. The standard of care for esophageal cancer patients is neoadjuvant chemoradiotherapy followed by surgery to remove the tumor. Until recently, no adjuvant treatment had been established, and surveillance was the only course of action for patients who remained at high risk of recurrence after surgery. A phase III clinical trial evaluated the benefit of using the immune checkpoint inhibitor nivolumab—previously approved in June 2020 for treatment of advanced esophageal cancer in patients who do not respond well to cytotoxic chemotherapy (467)Sengupta R, Honey K. AACR Cancer Progress Report 2020: Turning Science into Lifesaving Care. Clin Cancer Res. 2020;26(19).—as adjuvant therapy to eradicate the residual cancer following surgery. The clinical trial that was used by FDA to approve nivolumab as adjuvant therapy showed that the risk of death or recurrence of cancer decreased 31 percent in patients who were treated with nivolumab following surgery when compared to patients in the control group. Moreover, the median disease-free survival of patients who underwent adjuvant therapy with nivolumab was twice as long as for those who received placebo (509)Kelly RJ, Ajani JA, Kuzdzal J, et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N Engl J Med. 2021;384(13).. These results led FDA to approve nivolumab in May 2021 as an adjuvant therapy for esophageal and GEJ cancer patients, who had residual cancer at the time of surgery.
In April 2021, FDA approved nivolumab in combination with fluoropyrimidine- and platinum-containing chemotherapy for the initial treatment of patients with advanced or metastatic gastric cancer, GEJ cancer, and esophageal adenocarcinoma. The approval was based on data from a large clinical trial which showed that the addition of nivolumab to a chemotherapeutic regimen increased median overall survival of patients by more than two months compared to chemotherapy alone.
During the 12 months spanning this report, FDA also approved the immune checkpoint inhibitor pembrolizumab in combination with fluoropyrimidine- and platinum-containing chemotherapy to treat patients with metastatic or locally advanced esophageal or GEJ cancer whose tumor can neither be removed by surgery nor treated with chemoradiotherapy. The addition of pembrolizumab to chemotherapeutic regimens increased median overall survival of patients to more than a year, compared to less than 10 months in those who only received chemotherapy.
In May 2021, FDA expanded the use of pembrolizumab in combination with the HER2-targeted therapeutic trastuzumab and fluoropyrimidine- and platinum-containing chemotherapy for the first-line treatment of gastric or GEJ cancer patients whose tumors were metastatic or at an advanced stage and were positive for HER2, a protein frequently found on the cell surface of many types of cancer including gastric cancer. Seventy-four percent of patients who had pembrolizumab added to their treatment regimen (i.e., trastuzumab and fluoropyrimidine- and platinum-containing chemotherapy) had tumor shrinkage compared to 52 percent of those who were in the control group.
Recurrent or metastatic triple-negative breast cancer accounts for about 10-15 percent of all breast cancer and is characterized by rapid clinical progression and limited treatment options (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. During the 12 months spanning this report, FDA further expanded the use of pembrolizumab in combination with chemotherapy to treat patients who have locally recurrent or metastatic triple-negative breast cancer (TNBC) that cannot be surgically removed and whose tumors express the checkpoint protein PD-L1. The FDA also approved the PD-L1 IHC 22C3 pharmDx as a companion diagnostic for selecting patients with TNBC who are eligible for treatment with pembrolizumab. The approval was based on findings that TNBC patients, treated with a combination of pembrolizumab and chemotherapy, showed a median progression-free survival of 9.7 months, compared to only 5.6 months in the control group (510)Cortes J, Cescon DW, Rugo HS, et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomised, placebo-controlled, double.
The remarkable benefit of checkpoint inhibitors in saving and improving the lives of patients across a broad spectrum of cancer types is somewhat restricted by the fact that not all types of tumors respond to these immunotherapeutics and many that do eventually develop resistance to the treatment. Researchers are continuously working to develop innovative and improved strategies to bring the promise of these immunotherapeutics to as many additional cancer patients as possible. It will also be important to establish whether patients who are treated with newly approved immunotherapeutics develop any common side effects, as has been recently reported for melanoma patients on adjuvant immunotherapy, and how to effectively mitigate these adverse effects (511)Patrinely JR, Johnson R, Lawless AR, et al. Chronic immune-related adverse events following adjuvant anti-PD-1 therapy for high-risk resected melanoma. JAMA Oncol. 2021;7(5)..
Engineering Immune Cells to Eliminate Cancer
Another form of immunotherapy that has shown extraordinary success against certain types of cancer is called adoptive cell therapy or cellular immunotherapy. Adoptive cell therapy is one of the more recent approaches that is designed to dramatically increase the number of cancer-killing T cells, thus giving a patient’s immune system a boost to seek and destroy cancer cells (512)Rohaan MW, Wilgenhof S, Haanen JBAG. Adoptive cellular therapies: the current landscape. Virchows Arch. 2019;474(4).. Adoptive cell therapy is a complex multistep medical procedure. During the treatment, T cells are harvested from the patient to either expand them in number or genetically modify them in the laboratory to enhance their cancer-fighting capabilities, and then reinfused in the patient to help eliminate cancer cells. Currently, there are three types of adoptive cell therapies:
- For chimeric antigen receptor (CAR) T-cell therapy, T cells are harvested from a patient’s blood and genetically modified in the laboratory to have a new gene that encodes a protein called a CAR. The T cells are expanded in number and infused back into the patient. The CAR modification targets the T cells specifically to the patient’s cancer cells and triggers them to attack when they get there. This is the only type of adoptive cell therapy that is currently approved by FDA for treatment of different types of cancer (see sidebar on FDA-approved CAR T-Cell Therapies).
- For T-cell receptor (TCR) T-cell therapy, T cells are harvested from a patient’s blood and genetically modified in the laboratory to have a new gene that encodes a protein called a TCR. The T cells are expanded in number and infused back into the patient. The TCR modification targets the T cells specifically to the patient’s cancer cells that express a particular peptide recognized by the TCR and triggers them to attack.
- For tumor-infiltrating lymphocyte (TIL) therapy, T cells are harvested directly from a patient’s tumor, expanded in number in the laboratory, and infused back into the patient. Many of these T cells naturally recognize and kill the patient’s cancer cells.
Because of the complex nature of the procedure, as well as the potentially life-threatening side effects of the treatment, CAR T-cell therapies are only performed at specially certified health care facilities by highly trained medical professionals. Ongoing research is focused on developing strategies that reduce the complexity of the procedure, while simultaneously increasing the benefit for the patient. One such strategy is to use frozen or “off-the-shelf” CAR T-cells that are developed using T cells from donors other than the patient. The benefits of using these CAR T-cells include immediate availability and the possibility to genetically modify them against multiple targets present on the cancer cell surface (513)Depil S, Duchateau P, Grupp SA, Mufti G, Poirot L. ‘Off-the-shelf’ allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov. 2020;19(3).. However, potentially life-threatening side effects of using frozen CAR T-cells, as well as the challenge of their rapid elimination by the patient’s immune system, remain key barriers in routinely using this strategy to treat cancer and addressing these barriers is an active area of cancer immunology research (514)Perez C, Gruber I, Arber C. Off-the-Shelf Allogeneic T Cell Therapies for Cancer: Opportunities and Challenges Using Naturally Occurring “Universal” Donor T Cells. Front Immunol. 2020;11..
The extraordinary progress toward harnessing the potential of adoptive T-cell therapy for treatment of cancer is underscored by the approval of two new CAR T-cell therapies covered in this report: idecabtagene vicleucel (Abecma) to treat relapsed or refractory multiple myeloma, and lisocabtagene maraleucel (Breyanzi) to treat relapsed or refractory large B-cell lymphoma. During the 12 months covered in this report, FDA also expanded the use of axicabtagene ciloleucel (Yescarta) to treat relapsed or refractory follicular lymphoma. These approvals bring the number of FDA-approved CAR T-cell therapies to five.
Idecabtagene vicleucel is the first FDA-approved adoptive cell therapy for multiple myeloma (see sidebar on Two Decades of Progress Against Multiple Myeloma) and is great news for multiple myeloma patients like Dr. David Wellenstein. It was approved for the treatment of adult patients with relapsed or refractory multiple myeloma who have received four or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody. The design of idecabtagene vicleucel is unique because it is directed against the protein B-cell maturation antigen (BCMA) on cancer cells, compared to prior CAR T-cell therapies approved by FDA that were directed against the protein CD19 on cancer cells (464)Wang K, Wei G, Liu D. CD19: a biomarker for B cell development, lymphoma diagnosis and therapy. Exp Hematol Oncol. 2012;1(1).. Expression of BCMA is largely restricted to plasma cells, which are blood cells that make antibodies to protect against infections (434)van de Donk NWCJ, Pawlyn C, Yong KL. Multiple myeloma. Lancet. 2021;397(10272):410-427., and is much higher in myeloma cells compared to normal plasma cells (462)Yu B, Jiang T, Liu D. BCMA-targeted immunotherapy for multiple myeloma. J Hematol Oncol. 2020;13(1).. Among the 128 patients participating in the clinical trial who received idecabtagene vicleucel, the overall response rate was 73 percent, and 33 percent of patients achieved complete response (see Table 6), meaning that cancer was no longer detectable. An estimated 65 percent of those with complete response maintained this response for at least one year (515)Munshi NC, Anderson LD, Shah N, et al. Idecabtagene Vicleucel in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2021;384(8):705-716.. The use of BCMA marks a key milestone in CAR T-cell therapy because it provides options to develop CAR T cells that are more specific to a cancer type and can potentially reduce some of the serious side effects associated with CAR T-cell therapies.
The second newly approved CAR T-cell therapy is lisocabtagene maraleucel, which is directed against CD19 and induces cell death in CD19-expressing cancer cells. In February 2021, FDA approved lisocabtagene maraleucel for the treatment of adult patients with relapsed or refractory large B-cell lymphoma who have received two or more lines of systemic therapy, including patients with diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma.
The FDA approval of lisocabtagene maraleucel was based on data from a clinical trial evaluating efficacy of the treatment in 192 adult patients with relapsed or refractory large B-cell non-Hodgkin lymphoma who have received at least two previous therapies. Of these patients, 54 percent had minimal or no detectable lymphoma remaining following treatment with lisocabtagene maraleucel and another 19 percent achieved a partial response. Of 104 patients who achieved the best overall response to the treatment, the cancer remained undetectable or at reduced levels for at least nine months in 62 percent of patients (516)Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254)..
Treatment with lisocabtagene maraleucel can cause severe and potentially life-threatening adverse effects. One of the most concerning is cytokine-release syndrome (CRS), an inflammatory response to the modified T cells that can rapidly cause organ dysfunction and/or failure, and neurotoxicity. Because of the potential serious side effects, FDA has approved lisocabtagene maraleucel with a risk evaluation and mitigation strategy under which health care facilities administering the treatment are required to be specially certified to recognize and manage CRS and nervous system toxicities.
During the 12-month period covered by this report, FDA also expanded the use of a previously approved CAR T-cell therapy, axicabtagene ciloleucel (Yescarta), for adult patients with relapsed or refractory follicular lymphoma (FL) who have received two or more lines of systemic therapy. The FDA’s decision was based on clinical trial results showing that axicabtagene ciloleucel therapy eliminated all signs of cancer in 60 percent of patients within one month of the treatment.
Ongoing research is focused on identifying proteins that are preferably present only on the surface of cancer cells and can be used to develop CAR T-cell therapies that are more specific to the type of cancer against which they are being used. These approaches, such as development of a CAR that targets both CD19 and CD22 proteins present on the cell surface in B-cell lymphoma thereby increasing specificity against cancer cells (517)Qin H, Ramakrishna S, Nguyen S, et al. Preclinical Development of Bivalent Chimeric Antigen Receptors Targeting Both CD19 and CD22. Mol Ther – Oncolytics. 2018;11., will ensure that there are minimal adverse side effects for patients treated with these immunotherapeutics.
Unleashing the Body’s Defense System Against Cancer
One class of immunotherapeutics to treat cancer works, in part, by helping immune cells find cancer cells more effectively (see Cell Lysis Mediators in Supplemental Table 2). These immunotherapeutics use a mechanism, called antibody-dependent cellular toxicity (ADCC), to direct immune cells to the tumor, where immune cells kill the target cancer cells. During the 12-month period covered in this report, FDA approved two new immunotherapeutics—naxitamab-gqgk (Danyelza) and margetuximab-cmkb (Margenza)—that invoke ADCC to destroy cancer cells.
In December 2020, FDA approved margetuximab-cmkb in combination with chemotherapy for the treatment of adult patients with metastatic HER2-positive breast cancer who have received two or more prior HER2-targeted treatments, at least one of which was for metastatic disease. Margetuximab-cmkb is an antibody that targets HER2, a protein commonly present in high concentrations on the surface of certain types of aggressive breast cancer. Once bound to HER2 protein, margetuximab-cmkb inhibits tumor growth and is designed to enhance recruitment of immune cells to kill cancer cells (518)Nordstrom JL, Gorlatov S, Zhang W, et al. Anti-tumor activity and toxicokinetics analysis of MGAH22, an anti-HER2 monoclonal antibody with enhanced Fcγ receptor binding properties. Breast Cancer Res. 2011;13(6).. The FDA’s decision was based on results of a phase III randomized clinical trial (519)Rugo HS, Im SA, Cardoso F, et al. Efficacy of Margetuximab vs Trastuzumab in Patients with Pretreated ERBB2-Positive Advanced Breast Cancer: A Phase 3 Randomized Clinical Trial. JAMA Oncol. 2021;7(4).. About 22 percent of patients treated with a combination of margetuximab-cmkb and chemotherapy responded to the treatment, compared to 16 percent of those treated with a combination of chemotherapy and another anti-HER2 targeted therapeutic trastuzumab (Herceptin). Patients in the margetuximab-cmkb treatment group also showed a modest increase in the length of time when the tumor did not progress (about six months versus five months in the trastuzumab treatment group). HER2-positive breast cancer is more aggressive and more likely to return than HER2-negative breast cancer (520)Mitsogianni M, Trontzas IP, Gomatou G, Ioannou S, Syrigos NK, Kotteas EA. The changing treatment of metastatic her2-positive breast cancer (Review). Oncol Lett. 2021;21(4).. Even a modest benefit from new immunotherapeutics such as margetuximab-cmkb is a positive step toward improving the lives of patients with HER2 positive metastatic breast cancer.
Neuroblastoma, although a rare cancer, is the most common cancer type in infants who are less than one year old. It accounts for roughly six percent of all childhood cancers. Neuroblastoma is a particularly devastating type of cancer because, in about two thirds of the cases, it has already spread to the lymph nodes or to other parts of the body at the time of diagnosis (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15.. Most common treatments for neuroblastoma—depending on the extent to which the disease has progressed—include surgery, chemotherapy, and radiation therapy. Only 40-50 percent of patients diagnosed with high-risk neuroblastoma—the form of neuroblastoma that cannot be removed surgically—live five years or more after diagnosis (3)American Cancer Society. American Cancer Society: Cancer Facts and Figures 2021. Atlanta Am Cancer Soc. Published online 2021:13-15., underscoring an unmet need to develop effective therapeutics against it (521)Van Arendonk K, Chung D. Neuroblastoma: Tumor Biology and Its Implications for Staging and Treatment. Children. 2019;6(1).. In November 2020, FDA granted approval to naxitamab-gqgk (Danyelza) in combination with granulocyte-macrophage colony-stimulating factor (GM-CSF), an immune-system boosting agent, for children one year of age and older and adult patients with relapsed or refractory high-risk neuroblastoma in the bone or bone marrow who have shown a partial response, minor response, or stable disease to prior therapy. Naxitamab-gqgk joins dinutuximab (Unituxin) to become the second immunotherapeutic approved by FDA to treat patients with high-risk neuroblastoma. Similar to dinutuximab, naxitamab-gqgk also binds to GD2, a lipid-carbohydrate hybrid molecule, that is present on the surface of neuroblastoma cells (522)Terzic T, Cordeau M, Herblot S, et al. Expression of Disialoganglioside (GD2) in Neuroblastic Tumors: A Prognostic Value for Patients Treated With Anti-GD2 Immunotherapy. Pediatr Dev Pathol. 2018;21(4).. Naxitamab-gqgk binds to GD2 and flags neuroblastoma cells for immune cells which upon binding to another part of naxitamab-gqgk are triggered to destroy the cancer cell. In one of the two clinical trials evaluating efficacy of naxitamab-gqgk, the overall response rate (see Table 6) among 38 patients treated with naxitamab-gqgk was 34 percent, and 23 percent of those who responded maintained the response for at least six months. Long term evaluation of patients who received the treatment, as well additional independent clinical studies, will be necessary to determine whether naxitamab-gqgk treatment also improves overall survival and quality of life for patients with high-risk neuroblastoma.