Reducing the Risk of Cancer Development
In this section, you will learn:
- In the United States (US), about 40 percent of all cancer cases are associated with modifiable risk factors, which necessitates a robust emphasis on and support for public health–focused research.
- The significant decline in cancer mortality over the past three decades is, in part, attributable to reductions in smoking following the implementation of public health campaigns and policy initiatives.
- Nearly 20 percent of US cancer diagnoses are related to excess body weight, unhealthy dietary patterns, alcohol intake, and physical inactivity.
- Vaccination against human papillomavirus (HPV) nearly eliminates the risk of cancers of the cervix, vagina, penis and anus caused by the virus.
- Exposure to high levels of chemicals in the environment, including air pollution, radon, endocrine-disrupting chemicals, and industrial chemicals, can increase an individual’s risk of certain types of cancer.
- Workers who are exposed to carcinogens and those who participate in night-shift work are also at an elevated risk of developing certain types of cancer.
- Reproductive and hormone-related factors can significantly influence the risk of developing various cancers, with effects varying by cancer type, timing, and duration of hormone exposure.
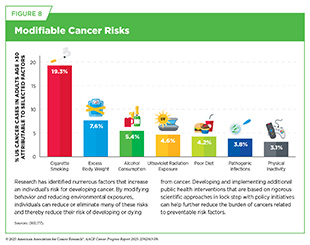
Advances in basic, clinical, translational, and population sciences have significantly expanded our understanding of the factors that contribute to an individual’s risk of developing cancer (see Figure 8). In 2019, an estimated 40 percent of all new cancer cases diagnosed in the United States (US) were attributable to modifiable risk factors including: cigarette smoking, ultraviolet (UV) radiation, excess body weight, alcohol consumption, physical inactivity, and infectious agents (163)Islami F, et al. (2024) CA Cancer J Clin.. Similarly, at the global level, around 40 percent of the total cancer burden is attributed to tobacco use, infectious agents, alcohol consumption and excess body fat (164)American Cancer Society. The Cancer Atlas. Accessed: June 30, 2025.. Because many of these risk factors are potentially modifiable or manageable, a substantial proportion of cancer cases could be possibly avoided through tailored prevention strategies.
Importantly, while these factors are considered modifiable, they are influenced by social and structural drivers of health (see Figure 3) and may not always be addressed solely through individual behavior change. For example, individuals experiencing food insecurity—a social driver of health—struggle to obtain a healthy diet. Similarly, those living in unsafe neighborhoods without well-maintained parks face significant barriers to engaging in regular physical activity. To effectively reduce the burden of modifiable risk factors and, in turn, the overall cancer burden, interventions must incorporate both individual- and societal-level strategies.
While our discussion in the following section focuses primarily on behavioral or lifestyle-related risk factors, the role of psychosocial risk factors should not be overlooked. Psychosocial risk factors, which include depression, anxiety, and stress, have been associated with cancer risk (165)McGee R, et al. (1994) Soc Sci Med, 38: 187.(166)Oerlemans ME, et al. (2007) Clin Pract Epidemiol Ment Health, 3: 29. and outcomes (167)Chida Y, et al. (2008) Nat Clin Pract Oncol, 5: 466. with mixed findings. However, when examined independently, stress—whether chronic or acute—has been more consistently associated with increased cancer risk (168)Dalton SO, et al. (2002) Eur J Cancer, 38: 1313.. Despite this evidence, its exact role remains difficult to determine due to challenges in quantifying stress exposure and controlling stress. In addition, stress may indirectly elevate cancer risk by promoting unhealthy behaviors such as smoking, alcohol use, and poor diet, all of which are well-established risk factors for cancer development.
Increasing evidence shows that stress is not just a trigger for risk-enhancing behaviors but may also act directly on the body by promoting inflammation, disrupting hormone balance, and weakening immune function, all of which can contribute to cancer development and worse outcomes (169)Antoni MH, et al. (2023) Annu Rev Psychol, 74: 423.(170)Mohan A, et al. (2022) Eur J Cancer Prev, 31: 585.. As such, stress is gaining recognition as an independent risk factor for cancer initiation and progression (see Sidebar 15).
In the United States, many of the greatest reductions in cancer morbidity and mortality have been achieved through the implementation of effective public education and policy initiatives. A recent study by the National Cancer Institute (NCI) estimated that approximately 5.94 million cancer deaths were averted from 1975 to 2020 due to public health interventions—including tobacco control programs, national screening, and vaccination programs, as well as advances in treatment (see Advancing Policies to Strengthen Cancer Prevention and Screening Programs). These gains were primarily seen in cancers for which effective screening methods are available: breast, cervical, colorectal, and prostate cancers (see Cancer Screening for Early Detection). Lung cancer accounted for the greatest number of deaths averted, largely due to tobacco control efforts (67)Islami F, et al. (2025) CA Cancer J Clin, 75: 216..
While smoking rates have declined significantly, the increasing prevalence of other risk factors, including obesity among US children and adults and alcohol consumption among adults, remains a significant public health concern (178)Ochiai E, et al. (2021) J Public Health Manag Pract, 27: S235.. In 2018, the most recent year for which data are available, 52.8 percent of US adults reported regular alcohol consumption (179)National Center for Health Statistics. FastStats – Alcohol Use. Accessed: June 30, 2025.. Compounding these concerns is the underutilization of preventive interventions in the United States, including vaccination against cancer-causing viruses like human papillomavirus (HPV), the primary cause of cervical cancer and certain head and neck cancers.
Harmful contaminants found in air and drinking water, including arsenic, nitrates, disinfection byproducts, and per- and poly-fluoroalkyl substances (PFAS), have been linked to elevated cancer risk (180)Beane Freeman LE, et al. (2022) Environ Health Perspect, 130: 57006.(181)Purdue MP, et al. (2023) Environ Health Perspect, 131: 77007.. Additionally, occupational exposures to hazardous agents—such as chemicals encountered during firefighting, silica dust in mining, and noxious fumes in fabrication or roofing—can significantly contribute to cancer development.
Emerging data indicate that certain cancer risk factors are also associated with worse outcomes after a cancer diagnosis, including development of secondary cancers (see Supporting Cancer Patients and Survivors). In addition, cancer risk factors contribute to other chronic diseases, such as cardiovascular and respiratory diseases and diabetes. Increased recognition of these modifiable risk factors can help local and national public health organizations enhance prevention efforts and lessen the negative health and economic impact of these diseases, including cancer.
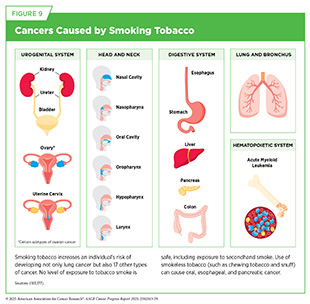
Eliminate Tobacco Use
Tobacco use, particularly cigarette smoking, is the leading preventable cause of cancer and is linked to the development of 17 different types of cancer in addition to lung cancer (see Figure 9). In the United States, cigarette use is responsible for approximately 19 percent of all cancer cases and nearly 30 percent of all cancer-related deaths (163)Islami F, et al. (2024) CA Cancer J Clin.. Between 80 and 90 percent of US lung cancer deaths are attributable to smoking (182)Warren GW, et al. (2013) Am Soc Clin Oncol Educ Book, 33: 359.. Moreover, cigarette use is associated with a significant reduction in life expectancy, contributing to nearly 10 years of life lost (183)Jha P, et al. (2013) N Engl J Med, 368: 341..
Research over the past 50 years has demonstrated that byproducts released from smoking tobacco products, such as cigarettes, cause permanent cellular and molecular alterations, which lead to cancer (184)Alexandrov LB, et al. (2016) Science, 354: 618.(185)Pezzuto A, et al. (2019) Future Sci OA, 5: FSO394.(186)Yang Y, et al. (2023) J Hazard Mater, 455: 131556.. Furthermore, smoking causes many other chronic conditions, including chronic obstructive pulmonary disease (COPD), asthma, and many types of cardiovascular diseases, particularly coronary artery disease.
In response to the serious health risks associated with smoking, nationwide tobacco control initiatives have played a critical role in reducing cigarette use among US adults. Smoking rates have dropped from 42.4 percent in 1965 to just 11 percent in 2023 (31,187). Between 2017 and 2023 alone, the number of adults who exclusively smoked cigarettes decreased by 6.8 million. However, this decline was nearly offset by a rise in electronic cigarette (e-cigarette) use in adults (approximately 7.2 million) (188)Arrazola RA, et al. (2025) MMWR Morb Mortal Wkly Rep, 74:118.. Additionally, in 2023, the most recent year for which such data are available, an estimated 48.6 million US adults reported using any tobacco product (e.g., cigarettes, cigars, and pipes) (188)Arrazola RA, et al. (2025) MMWR Morb Mortal Wkly Rep, 74:118..
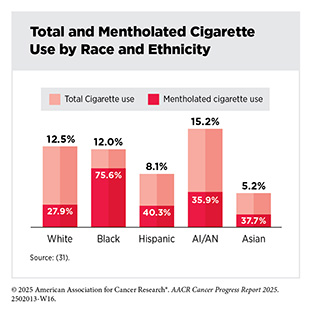
There are striking disparities in the use of tobacco products as well as in exposure to secondhand smoke, also a cancer risk factor, as highlighted in the AACR Cancer Disparities Progress Report 2024. Overall, current use of cigarettes is higher among males, individuals ages 45 to 64, individuals without a high school diploma, sexual and gender minorities, those who are uninsured or insured by Medicaid, and US residents who live in the South and Midwest (31)Bandi P, et al. (2025) Cancer Epidemiol Biomarkers Prev, 34: 836..
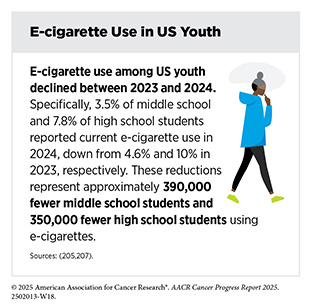
Similar to the trend in adults, tobacco use among US youth—including middle and high school students—is also declining. In 2024, 5.4 percent of middle and 10.1 percent of high school students reported current use of any tobacco product (189)Jamal A, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 917.. Among high school students, the number of current tobacco users dropped from 1.97 million in 2023 to 1.58 million in 2024, representing 390,000 fewer users. Unlike adults, for whom cigarettes remain the most commonly used tobacco product, e-cigarettes are the most used tobacco product among middle and high school–age youth.
Flavored tobacco products, such as mentholated cigarettes, pose a significant health risk, because they are associated with increased nicotine dependence, lowered smoking cessation rates, and increased mortality compared to nonmentholated cigarettes (187)Bandi P, et al. (2025) Tob Control.(190)Villanti AC, et al. (2021) Nicotine Tob Res, 23: 1318.(191)Delnevo CD, et al. (2011) Am J Prev Med, 41: 357.. In 2020, 43.4 percent of Americans who smoke used mentholated cigarettes, with usage particularly high in Black individuals and young adults ages 18 to 25 years (192)Goodwin RD, et al. (2023) Nicotine Tob Res, 25: 692.. Among middle and high school students, who predominantly use e-cigarettes, 87.6 percent used flavored e-cigarettes, with fruit flavors being the most popular (189)Jamal A, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 917..
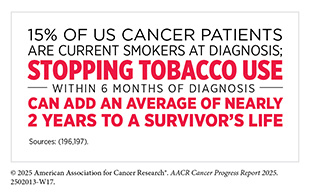
Although smoking prevalence in the United States has declined significantly, cessation remains a challenge. In 2022, 67.7 percent of current smokers expressed a desire to stop, and 53.3 percent made an attempt, yet only 8.8 percent were successful (193)VanFrank B, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 633.. Smoking cessation yields both immediate and long-term health benefits, especially when cessation occurs at a younger age. Within 10 years of cessation, the risk of developing cancers of the larynx, oral cavity, and pharynx is reduced by half (194)Khalifeh M, et al. (2024) BMJ Open, 14: e074723.(195)Marron M, et al. (2010) Int J Epidemiol, 39: 182..
Public health campaigns aimed at banning the sale of mentholated cigarettes and flavored e-cigarettes have been met with mixed responses (198)Anderer S (2025) JAMA, 333: 657.(199)Rubin R (2024) JAMA, 332: 692.. Nonetheless, evidence-based interventions at local, state, and federal levels—such as increasing tobacco prices, implementing public health campaigns, restricting targeted marketing, providing subsidized smoking cessation counseling through insurance, offering FDA-approved medications, and enforcing smoke-free laws—are essential to sustaining the downward trend of tobacco use (see Flavored Tobacco Products).
Secondhand smoke—the combination of smoke exhaled by individuals who use tobacco products and the smoke emitted from burning tobacco—contains more than 7,000 chemicals, including at least 70 known carcinogens (200)Yousuf H, et al. (2020) JAMA Netw Open, 3: e201177.(201)Stepanek L, et al. (2022) Int J Environ Res Public Health, 19.. Encouragingly, exposure to secondhand smoke in the United States has decreased, from 27.7 percent during 2009–2010 to 20.7 percent in 2017–2018, the most recent period for which data are available (202)QuickStats: Trends in Secondhand Smoke Exposure Among Nonsmoking Adults, by Race and Hispanic Origin — National Health and Nutrition Examination Survey, United States, 2009–2018. MMWR Morb Mortal Wkly Rep 2021;70:224.. However, exposure remains disproportionately high among some populations. These include children ages 3 to 11 years, regardless of race; non-Hispanic (NH) Black individuals; people with lower income or educational attainment; those living in rental or multi-unit housing; and those employed in blue-collar occupations (203)Centers for Disease Control and Prevention. Trends and Disparities in Secondhand Smoke | Smoking and Tobacco Use. Accessed:.
E-cigarettes were first introduced in the United States in 2006 and have gained popularity, particularly among individuals who have never previously used tobacco products. Since 2014, e-cigarettes have been the most used tobacco product among middle and high school students (189)Jamal A, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 917.. Recent estimates show that e-cigarette usage was highest among individuals ages 18 to 24 years, with 13.4 percent reporting current use; among these, 71.5 percent of individuals ages 18 to 20 years had never smoked combustible cigarettes (31)Bandi P, et al. (2025) Cancer Epidemiol Biomarkers Prev, 34: 836.(204)Erhabor J, et al. (2023) JAMA Netw Open, 6: e2340859..
In 2024, nearly 6 percent of middle and high school students used e-cigarettes, with 26.3 percent of users reporting daily use of e-cigarettes (205)Park-Lee E, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 774.. Among daily users, 87.6 percent reported using flavored e-cigarette products (205)Park-Lee E, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 774.. Several factors contribute to the initiation of tobacco use among youth, including the availability of flavored products, targeted marketing, a strong social media presence, and misperceptions about the potential harms of e-cigarettes (189)Jamal A, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 917.(206)Meehan J, et al. (2024) Global Pediatrics, 9: 100190..
While e-cigarettes emit fewer carcinogens than combustible tobacco, they still expose individuals to many toxic chemicals, including metals that can damage DNA and trigger inflammation (208)Goniewicz ML, et al. (2018) JAMA Netw Open, 1: e185937.(209)Herbst RS, et al. (2022) Clin Cancer Res, 28: 4861.. Further research is warranted on e-cigarettes and their long-term health effects, especially in teens and young adults so that appropriate preventive interventions can be implemented.
E-cigarettes have also become a popular tool for smoking cessation in adults. A recent review found that nicotine-based e-cigarettes increased quit rates by 59 percent compared to nicotine replacement therapy, and by 46 percent compared to non-nicotine e-cigarettes (210)Lindson N, et al. (2025) Cochrane Database of Systematic Reviews.. However, more rigorous research, including randomized clinical trials, is still needed to fully understand the effectiveness and long-term efficacy of e-cigarettes as a smoking cessation tool.
Maintain a Healthy Weight, Eat a Healthy Diet, and Stay Active
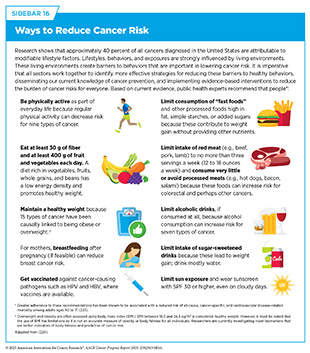
More than 20 percent of new cancer cases and more than 18 percent of cancer deaths in US adults are attributable to a combination of excess body weight, poor diet, physical inactivity, and alcohol consumption (see Figure 10) (163)Islami F, et al. (2024) CA Cancer J Clin.(211)Islami F, et al. (2018) CA Cancer J Clin, 68: 31.(212)Islami F, et al. (2019) JAMA Oncol, 5: 384.. Following a healthier lifestyle—maintaining a healthy weight, being physically active, and consuming a balanced diet—may reduce the risk of developing certain cancers, as well as many other adverse health outcomes (see Sidebar 16).
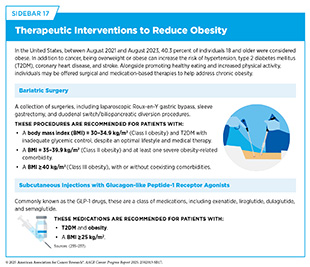
Excess body weight is responsible for 7.6 percent of all cancer cases (163)Islami F, et al. (2024) CA Cancer J Clin.. In the United States, the prevalence of obesity among adults was 40.3 percent between 2021 and 2023 (213)Emmerich SD, et al. (2024) NCHS Data Brief.. High body mass index (BMI) has also emerged as a major risk factor for reduced life expectancy in the United States, ranking among the top five risk factors that lead to a decline in life expectancy for the past 10 years (214)Ng, Marie et al. (2025) Lancet, 405: 813.. Obesity is not only a national concern but also a global public health crisis, according to the World Health Organization (WHO). In 2022, the most recent year for which global data are available, 43 percent and 16 percent of adults worldwide were classified as overweight and obese, respectively (215)Brauer, Michael et al. (2024) Lancet, 403: 2162.. In addition, childhood obesity is on the rise globally, with 8 percent of children and adolescents considered obese in 2022, a fourfold increase from 2 percent in 1990.
If current trends continue, more than half of the global adult population will be overweight or obese by 2050 (214)Ng, Marie et al. (2025) Lancet, 405: 813.. To address this crisis, Member States of WHO endorsed the WHO acceleration plan to stop obesity at its 2022 World Health Assembly. The plan includes policies aimed at protecting people from the harmful impact of processed food marketing; nutrition labeling (including front-of-pack labeling); fiscal policies (including taxes and subsidies to promote healthy diets); public food procurement and reformulation policies; physical activity; as well as school food and nutrition policies (including school food standards, food provision, and nutrition education) (225)World Health Organization. WHO Acceleration Plan to Stop Obesity. Accessed: June 30, 2025..
Emerging data show that weight loss interventions (see Sidebar 17) can be effective in reducing the risk of cancers associated with obesity (227)Schauer DP, et al. (2017) Obesity (Silver Spring), 25 Suppl 2: S52.(228)Bruno DS, et al. (2020) Ann Transl Med, 8: S13..
Bariatric surgery is a collection of procedures that when effectively paired with healthy eating and regular exercise may help people who are obese lose weight. Bariatric surgery has also been shown to lower the risk of developing and/or dying from certain obesity-associated cancers by between 37 percent and 65 percent (234)Wilson RB, et al. (2023) Int J Mol Sci, 24.. These include cancers of the liver, colon, pancreas, and gallbladder, as well as breast, endometrial, and ovarian cancers in women (234)Wilson RB, et al. (2023) Int J Mol Sci, 24..
Another increasingly popular weight loss strategy is the use of medications, such as semaglutide (Ozempic, Wegovy, Rybelsus) and tirzepatide (Mounjaro, Zepbound), which were originally used to treat individuals with type 2 diabetes mellitus (T2DM). These medications belong to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic GLP-1, a natural hormone that helps regulate insulin levels, suppresses appetite, and increases feelings of fullness after eating (238)Bettadapura S, et al. (2025) Int J Obes (Lond), 49: 418..
When combined with a healthy diet and regular physical activity, GLP-1 receptor agonists have led to significant weight loss for many individuals. A recent study found that BMI and obesity prevalence in the United States declined slightly in 2023 compared to 2022, with the most pronounced decrease in the South—where per capita use of GLP-1 receptor agonists was the highest (239)Rader B, et al. (2024) JAMA Health Forum, 5: e243685.. However, for individuals with obesity, bariatric surgery remains the most effective therapeutic option for achieving substantial and sustained weight reduction (240)Sarma S, et al. (2022) Obesity (Silver Spring), 30: 2111..
Although the effect of GLP-1 receptor agonists on weight loss is encouraging, more research is required to understand the long-term impact of these medications on reducing cancer risk. Emerging data show that in patients with T2DM, the use of GLP-1 receptor agonists can significantly reduce the risk of esophageal, colorectal, endometrial, gallbladder, kidney, liver, ovarian, and pancreatic cancers, as well as meningioma and multiple myeloma (241). Further, a study comparing bariatric surgery and GLP-1 receptor agonists found that both interventions similarly reduced the risk of developing obesity-related cancers (242)Wolff Sagy Y, et al. (2025) EClinicalMedicine, 83: 103213.. While these findings are promising, it is important to note that no long-term studies of the effects of GLP-1 receptor agonists have been done in the non-diabetic patient population. It will be important to continue monitoring the long-term effects of these weight loss medications in non-diabetic patients, as well as their ability to reduce obesity-related cancers.
A poor diet—high in red and processed meat, low in calcium, fiber, fresh fruits, and vegetables—is attributable to the development of more than 4.2 percent of all cancer cases in the United States. Numerous studies have shown an association between the consumption of highly processed foods and the increased risk of cancer (163)Islami F, et al. (2024) CA Cancer J Clin.(243)Morales-Berstein F, et al. (2024) Eur J Nutr, 63: 377.(244)Jin Q, et al. (2023) Br J Cancer, 129: 1978.(245)Chang K, et al. (2023) EClinicalMedicine, 56: 101840..
Between 2001–2002 and 2017–2018, the consumption of ultra-processed foods among US adults increased significantly, rising from 53.5 percent to 57.0 percent of total dietary intake. During the same period, the consumption of minimally processed foods declined from 32.7 percent to 27.4 percent (246)Juul F, et al. (2022) Am J Clin Nutr, 115: 211.. Approximately 73 percent of the US food supply now consists of ultra-processed products (247)Ravandi B, et al. (2025) Nat Food, 6: 296.. Higher consumption of these foods has been linked to accelerated biological aging—characterized by the gradual accumulation of molecular and cellular damage that impairs physiologic function and increases vulnerability to diseases, such as cancer. Reducing or eliminating ultra-processed foods from the diet may slow biological aging and lower cancer risk (248)Cardoso BR, et al. (2024) Age Ageing, 53..
Excessive red meat consumption can increase cancer risk. Intake of red meat specifically should be limited to no more than three servings a week (12 to 18 ounces a week) and should not include processed meats (e.g., hot dogs, bacon, and salami), because these foods can increase the risk of colorectal cancers and potentially other cancers including those of the lung, prostate, esophagus, and pancreas (249)Sivasubramanian BP, et al. (2023) Cureus, 15: e45324.(250)Di Y, et al. (2023) BMC Cancer, 23: 782.
(251)Kim Y (2023) Cancer Causes Control, 34: 569.(252)Meine GC, et al. (2024) Am J Gastroenterol, 119: 1056.(253)Caceres-Matos R, et al. (2024) Gastrointestinal Disorders, 6: 164(254)Visioli F, et al. (2024) Lancet Reg Health Eur, 38: 100863.(255)Ungvari Z, et al. (2025) Geroscience.(256)Yang J, et al. (2024) Antioxidants (Basel), 13.(257)Ghosn B, et al. (2025) Clin Nutr ESPEN, 67: 265.(258)Poorolajal J, et al. (2024) PLoS One, 19: e0305994.(259)Zhang X, et al. (2025) BMC Gastroenterol, 25: 332..
Sugar-sweetened beverages (SSB), which include any drink that contains added sugars, such as soda, fruit and sports drinks, and energy drinks, or coffee and tea with added sugars, have also been associated with increased risk of several cancers, such as liver and colon cancers (260)Zhao L, et al. (2023) JAMA, 330: 537.(261)Feng L, et al. (2023) Eur J Clin Nutr, 77: 941.(262)de Lorgeril M, et al. (2020) Transl Cancer Res, 9: 3172.(263)McCullough ML, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31: 1907.(264)Tseng TS, et al. (2021) World J Diabetes, 12: 1530.(265)Heo GY, et al. (2024) JAMA Netw Open, 7: e2356885.(266)Cai XY, et al. (2022) Clin Kidney J, 15: 718.. Recent data from the Nurses’ Health Study found that the consumption of one or more SSB daily has been associated with a four-fold increased risk of oral cavity cancers (267)Gomez-Castillo L, et al. (2025) JAMA Otolaryngol Head Neck Surg, 151: 450.. Further research is needed to assess the relationship of SSB consumption and cancer risk across a more diverse population.
One strategy to lower consumption of SSB is to implement taxes, such as those introduced in several cities in the United States. In cities with such taxes, significant reductions were made in the consumption of SSB compared to cities that did not implement these types of taxes (268)Hua SV, et al. (2023) Jama Network Open, 6: e2323200.(269)Kaplan S, et al. (2024) JAMA Health Forum, 5: e234737.(270)Bleich SN, et al. (2021) JAMA Netw Open, 4: e2113527.. As of 2022, eight US jurisdictions and more than 50 counties have implemented tax on SSB (269)Kaplan S, et al. (2024) JAMA Health Forum, 5: e234737.. However, preliminary data from these counties shows a varying response on the impact the tax has had on BMI and obesity prevalence. As one example, a study examining changes in BMI and obesity prevalence in California cities with SSB taxes—Albany, Berkeley, Oakland, and San Francisco—found no overall change in either measure. However, modest improvements were observed in specific subgroups, particularly among White individuals, women, and individuals ages 20 to 39 (271)Liu EF, et al. (2025) JAMA Netw Open, 8: e2456170.. Similarly, data from a study of children ages 2 to 18 in Philadelphia showed no significant reduction in BMI or obesity following the implementation of the tax (272)Gregory EF, et al. (2025) JAMA Pediatr, 179: 46.. Ongoing evaluation will be essential to understand the long-term effect of these policies on diet, obesity, and cancer risk.
Consumption of a diet rich in fresh fruits and vegetables, nuts, whole grains, and fish can help lower the risk of developing certain cancers and many other chronic conditions (258)Poorolajal J, et al. (2024) PLoS One, 19: e0305994.(273)Bui LP, et al. (2024) Am J Clin Nutr, 120: 80.(274)Cai Y, et al. (2024) Am J Clin Nutr, 119: 406.. A recent review consisting of over 5 million individuals found that high consumption of fish reduced the chance of developing colorectal cancer by 15 percent (258)Poorolajal J, et al. (2024) PLoS One, 19: e0305994.. One way to increase access to healthy foods is to eliminate food deserts, geographic areas with limited access to grocery stores, to make healthy foods more available. Another strategy is to educate the public about the benefits of nutritious foods in reducing the risk of developing cancer and other chronic illnesses, much like the successful campaigns used for tobacco control. Finally, shifting government subsidies away from commodity crops like corn and soy, which are used to produce added sugars in highly processed foods, toward whole food, minimally processed crops, is essential for promoting healthier diets and reducing the risk of cancer and other chronic diseases.
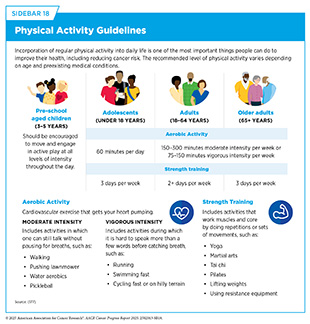
Engaging in regular physical activity at the levels recommended by the Centers for Disease Control and Prevention (CDC) can reduce the risk of nine different types of cancer, with research indicating that over 46,000 US cancer cases annually could potentially be avoided if everyone met the recommended CDC guidelines for physical activity (see Sidebar 18) (276)Lopez-Bueno R, et al. (2023) JAMA Intern Med, 183: 982.(277)Minihan AK, et al. (2022) Med Sci Sports Exerc, 54: 417.. One study involving 85,000 participants found that engaging in light-intensity or moderate to vigorous physical activity, lowered the risk of developing cancer by 6 percent and 13 percent, respectively; with sedentary behavior offering no benefit (278)Shreves AH, et al. (2025) Br J Sports Med, 59: 839.. In addition to reducing the risk of developing cancer, incorporating exercise after a cancer diagnosis can improve outcomes (see Supporting Cancer Patients and Survivors). In a recent study of colorectal cancer patients who received surgery and chemotherapy, 80 percent of those assigned to an exercise program had no evidence of disease, recurrence, or a new cancer diagnosis, compared to 74 percent of patients who received health education alone (279)Courneya KS, et al. (2025) N Engl J Med, 393: 13..
Developing widespread public health campaigns to increase physical activity is essential to reversing the growing trend of sedentary lifestyles in the United States. One example is the Active People, Healthy Nation initiative, which aims to help 27 million Americans become more physically active by 2027. This program focuses on creating activity-friendly communities, promoting physical activity in schools, and partnering with local leaders to implement tailored, community-based programs. On a global scale, WHO’s Global Action Plan on Physical Activity offers policy recommendations to encourage active living. These include expanding walking and cycling infrastructure, increasing opportunities for physical activity in schools and workplaces, and enhancing access to recreational spaces. By adopting these strategies, countries can reduce physical inactivity, and the associated health risks.
Reduce Alcohol Consumption
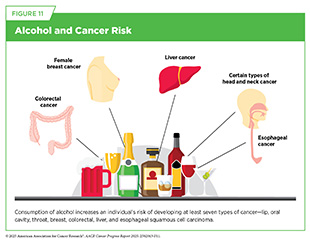
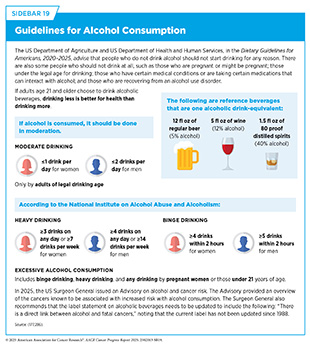
Excessive alcohol consumption increases the risk for at least seven different types of cancer (see Figure 11), and is linked to more than 200 diseases. Ongoing research continues to link alcohol consumption to various cancers; however, larger and more collaborative studies are needed to confirm a causal relationship. In the United States, about 5 percent of cancer cases were attributed to alcohol consumption in 2019, the most recent year for which data are available (31)Bandi P, et al. (2025) Cancer Epidemiol Biomarkers Prev, 34: 836.(163)Islami F, et al. (2024) CA Cancer J Clin.. This translates to about 97,000 cancer cases and 20,000 deaths. It is concerning that according to a recent nationally representative survey, 59.4 percent of Americans did not know that the consumption of alcohol increases the risk of cancer (281)Fokom Domgue J, et al. (2025) JAMA Oncol..
Limiting alcohol intake has been shown to reduce the risk against developing certain cancers. As an example, an international study consisting of data from 2.5 million patients from Asia, Australia, Europe, and North America found that with each additional alcoholic drink consumed daily, the risk of pancreatic cancer increased by 3 percent compared to not consuming alcohol daily or at all (282)Naudin S, et al. (2025) PLoS Med, 22: e1004590.. Alcohol consumption has also been associated with estrogen receptor–positive (ER+) breast cancers, the most common form of breast cancer. A recent review of alcohol consumption and breast cancer found that women who were not current drinkers were 12 percent less likely to develop an ER+ breast cancer (283)Terry MB, et al. (2024) Breast Cancer Res, 26: 179..
Public messaging campaigns (such as cancer-specific warning labels displayed on alcoholic beverages) along with effective clinical strategies must be considered to reduce the burden of alcohol-related cancers (see Sidebar 19) (284)Alcohol and Cancer Risk: The US Surgeon General’s Advisory. Alcohol and Cancer Risk: The US Surgeon General’s Advisory. Washington (DC)2025. One intervention in Canada showed that cancer risk warnings led to a decrease in alcohol sales for labeled products and an overall reduction in alcohol sales by 6.31 percent, indicating that proper labeling can reduce alcohol consumption (285)Zhao J, et al. The effects of alcohol warning labels on population alcohol consumption: An interrupted time series analysis of alcohol sales in Yukon, Canada. Journal of Studies on Alcohol and Drugs. Volume 81: Alcohol Research Documentation Inc.; 2020. p 225.
Protect Skin From UV Exposure
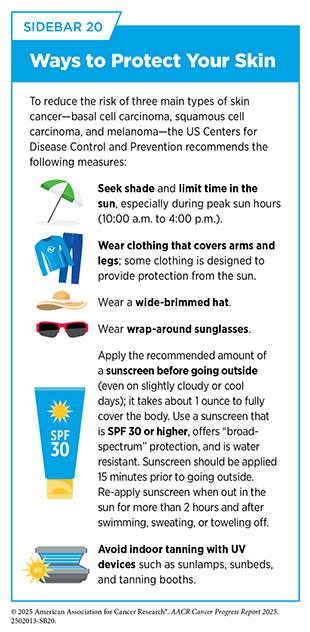
NCI defines ultraviolet (UV) radiation as invisible rays that are part of the energy released by the sun. UV radiation can also come from artificial sources such as sunlamps and tanning beds. There are three types of UV rays: UVA, which primarily contribute to skin aging and wrinkling; UVB, which are more likely to cause sunburn; and UVC, which are mostly absorbed by the Earth’s atmosphere and do not typically reach the surface. Exposure to any source of UV radiation can lead to skin cancers, including basal cell carcinoma, squamous cell carcinoma, and melanoma, the most aggressive form of skin cancer. In 2025, there will be an estimated 104,960 new diagnoses of melanoma of the skin and 8,430 deaths (see Table 1).
UV radiation accounts for 92 percent of skin melanoma cases and 4.6 percent of all cancer cases (163)Islami F, et al. (2024) CA Cancer J Clin.. UV radiation can damage cellular DNA, with continued exposure leading to cancer. Anyone can develop skin cancer, but some individuals are at a higher risk, especially those who are light skinned and those who are sunburned easily. A recent analysis of nationally collected health behavior data found that individuals with a history of severe sunburn—characterized by blistering or peeling—had 3.94 to 4.67 times higher odds of developing melanoma, respectively (287)Hosseinpour Z, et al. (2025) J Racial Ethn Health Disparities..
A common misconception is that people cannot get sunburned on cloudy days. However, up to 80 percent of harmful UV sunrays can penetrate clouds. It is recommended that individuals practice sun-safe habits anytime they are outside to limit exposure to harmful UV radiation (see Sidebar 20).
Indoor tanning exposes individuals to the same harmful UV radiation as sunlight, but in an artificial setting. Among US adults, indoor tanning decreased significantly between 2007 and 2018, from 10 percent to 4 percent. This decline has been largely attributed to legislation aimed at restricting youth access to indoor tanning. As of June 30, 2025, 44 states have legislation regulating tanning bed use by minors (290)Bowers JM, et al. (2020) Am J Public Health, 110: 823.. Of these, only 20 states and the District of Columbia have complete bans, while the remainder allow use with parental consent. To sustain and accelerate this downward trend, especially among adolescents, states with minimal to no legislation should consider enacting laws that ban indoor tanning for minors.
Prevent and Eliminate Infection From Cancer-causing Pathogens
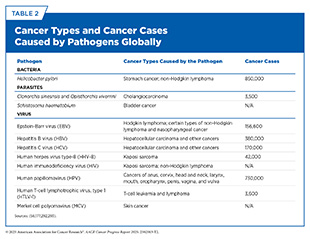
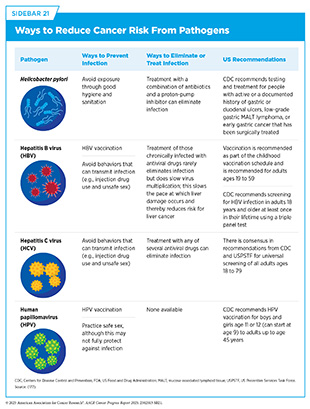
Cancer-causing pathogens (bacteria, viruses, and parasites) increase a person’s risk for several types of cancer (see Table 2). These pathogens may alter cellular function, suppress the immune system, and trigger chronic inflammation, all of which can contribute to cancer development. In the United States, about 3.4 percent of all cancer cases are attributable to infection with pathogens (163). Globally, an estimated 12 percent (2.3 million) of all cancer cases in 2020 were attributable to pathogenic infections, with more than 90 percent of these cases attributable to just four pathogens: human papillomavirus (HPV), hepatitis B (HBV), hepatitis C (HCV), and Helicobacter pylori (H. pylori) (291).
Individuals can significantly lower their risks by protecting themselves from infection through preventive measures such as vaccination or by seeking treatment to eliminate an infection (see Sidebar 21).
HPV, a group of more than 200 related viruses, is responsible for almost all cervical cancers, 90 percent of anal cancers, and 70 percent of oropharyngeal cancers, as well as most penile, vaginal, and vulvar cancers. While most HPV infections do not cause cancer, infection with high-risk strains of HPV for long periods (i.e., persistent infection) can lead to cancer. There are at least 15 high-risk HPV types, of which HPV 16 and 18 are responsible for most HPV-related cancers (294). In the United States, these high-risk HPV strains cause 1.2 percent and 2.5 percent of all cancers in men and women, respectively (163)Islami F, et al. (2024) CA Cancer J Clin.. Globally, HPV-related cancers make up about 4.5 percent of all cancers (295)de Martel C, et al. (2017) Int J Cancer, 141: 664..
The HPV vaccine is approved for males and females ages 9 to 45, with recommendations for the first doses beginning at ages 11 to 12. The HPV vaccine currently used in the United States, Gardasil 9, can protect against nine of the cancer-causing HPV strains. To eliminate HPV and its related cancer burden, the national goal is for 80 percent of adolescents to be completely vaccinated for HPV by receiving at least two doses of the vaccine (see Advancing Policies to Strengthen Cancer Prevention and Screening Programs). Individuals who initiate HPV vaccination at ages 15 to 45 years are recommended to receive three doses.
As of 2023, the most recent year for which data are available, only 61.4 percent of adolescents ages 13 to 17 had completed the recommended two dose vaccination series (296)Pingali C, et al. (2024) MMWR Morb Mortal Wkly Rep, 73: 708.. Encouragingly, this number continues to rise because of targeted public health campaigns aimed at increasing awareness and uptake. Reinforcing the value of early vaccination, cervical precancer incidence decreased by 79 percent in individuals ages 20 to 24 (297)Anderer S (2025) JAMA, 333: 1385.(298)Gargano JW, et al. (2025) MMWR Morb Mortal Wkly Rep, 74:96., the group most likely to have been vaccinated when the vaccine was first introduced. However, in adults ages 30 to 44 years, the completion rate for HPV vaccination was only 6.5 percent in 2023 (299)Gallagher TJ, et al. (2024) Otolaryngol Head Neck Surg, 171: 1780., indicating the need for targeted interventions for this age group.
Chronic infection from HBV and HCV can lead to liver cancer and has also been identified as a risk factor for other malignancies, such as non-Hodgkin lymphoma. Globally, chronic HBV and HCV infection is the most common risk factor for liver cancer and accounts for 55 percent and 21 percent of liver cancer deaths, respectively (164)American Cancer Society. The Cancer Atlas. Accessed: June 30, 2025.. In the United States, after new reported cases of HBV remained stable from 2013 to 2019, there was a sharp 32 percent decline in 2020, followed by additional decreases of 14 percent in 2021 and 6 percent in 2022 (300)Centers for Disease Control and Prevetion. Cancer Statistics At a Glance. Accessed: March 17, 2025.. Although this initial drop was believed to be due to a decrease in health care–seeking behaviors, that is, any action undertaken by individuals who perceive themselves to have a health problem or to be ill, for the purpose of finding an appropriate remedy, and decreased testing during the COVID-19 pandemic, the continued downward trend in 2023 suggests that reductions in HBV transmission may be occurring independently of pandemic-related disruptions (291)Centers for Disease Control and Prevention. 2025 Viral Hepatitis National Progress Report Overview | Viral Hepatitis. Accessed: June 30, 2025..
After a decade of increasing rates from 2011 to 2020, HCV rates have stabilized from 2020 to 2023 (301). However, disparities are notable. While acute HCV rates remained steady among NH White individuals between 2022 and 2023, rates among NH American Indian/Alaska Native (AI/AN) individuals rose by 22 percent and were 2.4 times higher than those among NH White individuals in 2023. To eliminate viral hepatitis as a public health threat, the US Department of Health and Human Services (HHS) released the Viral Hepatitis National Strategic Plan for the United States: A Roadmap to Elimination (2021–2025) in 2022. The primary goals are to prevent new infections, improve health outcomes for infected individuals, reduce disparities and health inequities, increase surveillance, and bring together all relevant constituents in coordinating efforts to address the hepatitis epidemic.
H. pylori is a type of bacteria. If left untreated, H. pylori infection can lead to gastric cancer. The infection causes chronic inflammation of the stomach lining, which over time increases the risk of developing gastric adenocarcinoma and gastric mucosa-associated lymphoid tissue (MALT) lymphoma—a rare form of non-Hodgkin lymphoma.
Rates of H. pylori infection are disproportionately higher among AI/AN communities. A recent study of over 750,000 individuals tested for H. pylori between 2000 and 2019 found that positive results were also more likely among older adults; men; individuals who identified as Asian, Black, or Hispanic; those with a non-English language preference; people living in areas with lower levels of college attainment; and individuals who were overweight (302)Li D, et al. (2024) Gastro Hep Adv, 3: 749.. These findings highlight the need for tailored screening and treatment strategies, particularly in underserved communities who face elevated risk and barriers to health care.
A substantial body of evidence supports the association between chronic H. pylori infection and cancer risk. Epidemiologic studies show that people with chronic H. pylori infection have increased risk of developing non-cardia gastric adenocarcinoma and that treatment of H. pylori infection decreases gastric cancer risk (303)Kumar S, et al. (2020) Gastroenterology, 158: 527.. Additionally, nearly all patients who develop MALT lymphoma show signs of H. pylori infection, and when these patients are treated with antibiotics, their tumors shrink (304)Parsonnet J, et al. (1994) N Engl J Med, 330: 1267.(305)Stathis A, et al. (2009) Ann Oncol, 20: 1086.(306)Kiesewetter B, et al. (2013) Blood, 122: 1350.. Globally the proportion of cancer cases caused by H. pylori infections is highest in South–Central and Eastern Asia, accounting for 69.7 percent of all cases, due to the high prevalence of the infection in these regions (293)American Cancer Society. Global Cancer Facts and Figures 5th Edition. Accessed: June 30, 2025..
Among those diagnosed with H. pylori infection, racial and ethnic minority populations and individuals who smoke are at an even greater risk for developing gastric cancer (307)Garman KS, et al. (2024) Gastric Cancer, 27: 28.. In the United States, the overall incidence of H. pylori-associated gastric cancer declined by 1 percent annually between 2010 and 2019. However, this decline was not consistent across all demographic groups.
Limit Exposure to Environmental Risk Factors
Environmental carcinogens are a class of pollutants that can lead to cancer and are present in the environment, including arsenic, asbestos, radon, lead, radiation, and other chemical pollutants. Exposure to higher than acceptable levels of environmental carcinogens without appropriate protection can increase the risk of cancer. The International Agency for Research on Cancer (IARC) and the US National Toxicology Program are both responsible for evaluating substances and exposures and classifying them as carcinogens at the global and national level, respectively.
Environmental pollutants are encountered in the air, drinking water, and food, making them nearly impossible to avoid. Federal government agencies, including the Environmental Protection Agency (EPA) and HHS, set guidelines for the acceptable exposure limits allowed in the environment (see Supplementary Table 1). However, some individuals experience higher levels of exposure to certain pollutants due to their living conditions and/or daily activities.
Hazardous materials present in both indoor and outdoor air, as well as in drinking water, can elevate the risk of developing cancer. Air pollution is the contamination of indoor or outdoor environments by chemical, physical, or biological agents that alter the natural characteristics of the atmosphere. Major air pollutants include carbon monoxide, ozone, nitrogen dioxide, sulfur dioxide, and particulate matter (PM), a mixture of solid particles and liquid droplets found in the air. Exposure to these substances has been consistently associated with an increased risk of cancers of the lung (33)Luo G, et al. (2025) The Lancet Respiratory Medicine.(35)LoPiccolo J, et al. (2024) Nat Rev Clin Oncol, 21: 121.(308)Zhang Y, et al. (2025) BMC Public Health, 25: 1260.(309)Hill W, et al. (2023) Nature, 616: 159., breast (310)Wu AH, et al. (2025) J Clin Oncol, 43: 273., and, more recently, skin (311)Chan FY, et al. (2025) PLOS Glob Public Health, 5: e0004357..
Drinking water can also contain contaminants including asbestos, arsenic, radon, agricultural chemicals, hazardous waste (316)Morris RD (1995) Environ Health Perspect, 103 Suppl 8: 225.(317)Levin R, et al. (2024) J Expo Sci Environ Epidemiol, 34: 3., and per- and poly-fluoroalkyl substances (PFAS), a group of endocrine-disrupting chemicals (EDCs) that have been shown to increase the risk of certain cancers, such as thyroid, ovarian, and breast cancers (see Sidebar 22) (318)van Gerwen M, et al. (2023) EBioMedicine, 97: 104831.(319)Liu B, et al. (2024) JAMA Netw Open, 7: e243127.(320)Rhee J, et al. (2024) Environ Int, 192: 109058..
In addition to outdoor air pollution and waterborne contaminants, exposure to indoor pollutants also poses a significant cancer risk. Radon is a naturally occurring radioactive gas formed from the breakdown of uranium in soil, rock, and water that can seep into homes through cracks in floors, walls, and gaps around pipes, wires, or pumps. Its levels vary by location and tend to be highest in areas rich in radioactive ore. Moreover, byproducts from previous mining of uranium, for example in the US Southwest, have led to increased levels of radon in nearby areas (323)Yazzie SA, et al. (2020) Int J Environ Res Public Health, 17: 2813., which disproportionately affect AI/AN tribal communities who live in these areas (324)Centers for Disease Control and Prevention. Raising Radon Awareness in Tribal Communities | Radon. Accessed: June 30, 2025..
Radon is the number one cause of lung cancer among people who have never smoked, and is the second leading cause of lung cancer overall, contributing to approximately 12 percent of lung cancers in the United States annually (325)Riudavets M, et al. (2022) Cancers (Basel), 14: 3142.(326)Liu Y, et al. (2024) Crit Rev Oncol Hematol, 198: 104363.(327)United States Environmental Protection Agency. Health Risk of Radon. Accessed: June 7, 2025.. To mitigate exposure, individuals should test for radon using approved test kits, which can be obtained, often for free or low cost, through resources listed on the EPA website.
Finally, the effects of climate change, defined as long-term shifts in temperature and weather patterns due to human activity, are an increasing concern among public health experts. Strong scientific evidence confirms that climate change is occurring and suggests that it intensifies exposure to carcinogens via air and water contamination. For example, wildfires in the Western United States and Canada have grown more frequent and severe in recent years due to climate change (328)US Global Change Research Program. Fourth National Climate Assessment. Volume II: Impacts, Risks, and Adaptation in the United States. Accessed: March 17, 2025.(329)Hvidtfeldt UA, et al. (2023) Cancer Epidemiol Biomarkers Prev, 32: 105.(330)Smotherman C, et al. (2023) Breast Cancer Res, 25: 83. and have led to greater exposure to toxic metals and chemicals (see Supplementary Table 1). These compounds, found in flame retardants, fire extinguishants, and pesticides, have been linked to cancer risk. A recent study found that firefighters exposed to one such class of compounds, haloalkanes, developed gliomas with tumor signatures associated with this exposure (331)Cannataro VL, et al. (2025) Cancer, 131: e35732..
As rates of lung cancer continue to rise among individuals who have never smoked, growing evidence suggests that air pollution is a contributing factor (33)Luo G, et al. (2025) The Lancet Respiratory Medicine.(332)Chartres N, et al. (2024) Environ Sci Technol, 58: 22843.(333)Jani CT, et al. (2025) EClinicalMedicine, 79: 103033.(334)Myers R, et al. (2021) J Thorac Oncol, 16: 1850.. One study attributed 1,100 lung cancer cases to air pollution exposure in the United Kingdom in 2022 (33)Luo G, et al. (2025) The Lancet Respiratory Medicine.. Another study found that individuals with lung cancer who have never smoked had significantly higher exposure to air pollution compared to those who were ever smokers (334)Myers R, et al. (2021) J Thorac Oncol, 16: 1850.. New laws, regulations, and policies to reduce the release of pollutants into the atmosphere are urgently needed to reduce the adverse health effects of environmental pollution, including cancer (see Environmental Justice and Cancer).
Where You Live Matters
Where individuals live can have a big impact on their health, especially when it comes to exposure to harmful chemicals in the air and water. Individuals living near industrial areas may have increased exposure to toxic chemicals and metals. These exposures can increase the risk for certain types of cancer, such as hematologic malignancies as well as thyroid, lung, breast, and uterine cancers (310)Wu AH, et al. (2025) J Clin Oncol, 43: 273.(318)van Gerwen M, et al. (2023) EBioMedicine, 97: 104831.(319)Liu B, et al. (2024) JAMA Netw Open, 7: e243127.(335)West M, et al. (2024) J Occup Environ Hyg, 21: 741.(336)Jephcote C, et al. (2020) Environ Health, 19: 53.(337)Cheng I, et al. (2022) Am J Respir Crit Care Med, 206: 1008.(338)Carroll R, et al. (2023) Environ Res, 239: 117349..
Disproportionate levels of exposure to air pollution based on geographic location is another major concern. In 2025, an estimated 156.1 million people were living in geographic areas with unhealthy levels of PM and 77.2 million people living in the United States were exposed to daily, unhealthy spikes in PM. This equates to 12.1 million more people exposed to daily, unhealthy spikes than in 2024 (339)American Lung Association. State of the Air 2023 Report. Accessed: March 17, 2025.. Low-income populations and racial and ethnic minority groups are among those who often experience higher exposure to pollutants (340)Bradley AC, et al. (2024) Environ Sci Technol, 58: 4226.(341)Tessum CW, et al. (2021) Sci Adv, 7: eabf4491..
Those who live in urban areas, particularly those with low socioeconomic status, are exposed to higher levels of certain traffic-related air pollutants, which are associated with an increased risk of breast and lung cancer (337)Cheng I, et al. (2022) Am J Respir Crit Care Med, 206: 1008.(338)Carroll R, et al. (2023) Environ Res, 239: 117349.. Public water systems are also a growing concern. In the United States, more than 97 million people are served by public water systems with detectable levels of unregulated contaminants. Notably, these public water systems disproportionately serve counties with higher proportions of Black and Hispanic residents, even after accounting for differences in socioeconomic status and neighborhood disadvantage (342)Maruzzo AJ, et al. (2025) Environ Health Perspect, 133: 17002.. These findings underscore the urgent need to investigate both regulated and unregulated drinking water contaminants and address disparities in exposure to environmental carcinogens that can have long-term effects.
Where You Work Matters
Because of elevated exposure to carcinogens, certain occupations—such as firefighting, industrial painting, and jobs in environments like iron and steel foundries or around welding fumes—have been classified by IARC as Group 1 carcinogens, indicating they are known to cause cancer in humans (343)Baan R, et al. (2009) Lancet Oncol, 10: 1143.. To reduce risk, workers should consistently use personal protective equipment (PPE) and ensure it is properly decontaminated after exposure to carcinogens and other hazardous substances.
Other risk factors associated with a person’s occupation, including lack of sleep and night-shift work, have also been shown to increase the risk of developing certain types of cancers and other chronic diseases, including diabetes and obesity (344)McDermott JE, et al. (2024) J Proteome Res, 23: 1547.. CDC reports that about 11 million adults in the United States frequently work night shifts. Certain segments of the population are more likely to work these shifts, including men, Black individuals, non Hispanic individuals, and those with only a high school education (345)National Toxicology Program. NTP Cancer Hazard Assessment Report on Night Shift Work and Light at Night. NTP Cancer Hazard Assessment Report on Night Shift Work and Light at Night. Research Triangle Park (NC): National Toxicology Program; 2021(346)National Toxicology Program. National Toxicology Program Cancer Hazard Assessment Report on Night Shift Work and Light at Night. Accessed: June 5, 2025..
The body of research on environmental and occupational exposures that increase cancer risk is steadily growing. Collaborative efforts like those led by the Cohorts for Environmental Exposures and Cancer Risks initiative are building the infrastructure to integrate scientific findings and better understand how environmental exposures, along with genetic, behavioral, and structural factors, affect cancer risk across diverse populations. Such efforts are vital to ensuring that interventions to reduce these exposures are implemented equitably.
Be Cognizant of Hormonal Factors
Family Planning, Pregnancy, and Breastfeeding
Studies have shown that a woman’s risk of developing certain gynecologic cancers is influenced by reproductive factors, such as oral contraceptive use, pregnancy, and breastfeeding, all of which affect exposure to estrogen and progesterone, hormones produced by the ovaries. Research on oral contraceptive use has found a slightly increased risk of breast and cervical cancer, but a reduced risk of endometrial and ovarian cancer. More recently, one study linked hormonal contraceptive use to an approximately 30 percent increased risk of breast cancer among women who carries mutations in the BRCA1 gene (347)Phillips KA, et al. (2025) J Clin Oncol, 43: 422.. Additionally, evidence indicates that women who have given birth have a lower risk of developing ER+ tumors compared to women who have never given birth. However, this protective effect is only observed a decade or more after a woman’s last pregnancy (348)Nichols HB, et al. (2019) Ann Intern Med, 170: 22.(349)Ambrosone CB, et al. (2020) Cancer Res, 80: 4871.(350)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706..
During the period immediately following pregnancy, women are at an elevated risk of developing pregnancy-associated breast cancers, which are the breast cancers diagnosed during gestation, lactation, and within 5 years postpartum (351)Proussaloglou EM, et al. (2023) Pathol Res Pract, 244: 154413.. Evidence has demonstrated that both estrogen receptor–negative tumors and triple-negative breast cancer are the most common subtypes of pregnancy-associated cancers (348)Nichols HB, et al. (2019) Ann Intern Med, 170: 22.(350)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706.(352)Vohra SN, et al. (2022) Cancer Epidemiol Biomarkers Prev, 31:561.. In the United States, there are about 3,500 cases of pregnancy-associated breast cancer each year (351). Furthermore, the mother’s age at pregnancy also influences breast cancer risk. Women who are older when they become pregnant are at increased risk of certain types of breast cancer (353)John EM, et al. (2024) Breast Cancer Res, 26: 88..
Breastfeeding, specifically lactation, has been linked to a reduced risk of breast and ovarian cancers (354)Millikan RC, et al. (2008) Breast Cancer Res Treat, 109: 123.(355)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723.(356)Fortner RT, et al. (2019) Breast Cancer Res, 21: 40.(357)Masi AC, et al. (2024) Microb Biotechnol, 17: e14520., with increased duration of breastfeeding associated with a further decrease in risk (350)Jung AY, et al. (2022) J Natl Cancer Inst, 114: 1706.(355)Lord SJ, et al. (2008) Cancer Epidemiol Biomarkers Prev, 17: 1723.(358)Anstey EH, et al. (2017) Am J Prev Med, 53: S40.(359)Palmer JR, et al. (2014) J Natl Cancer Inst, 106: dju237.(360)World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project. Expert Report 2018. Lactation and the Risk of Cancer. Accessed: June 6, 2025.. For example, breastfeeding for 1 to 3 months reduced the risk of ovarian cancer by 18 percent; breastfeeding for more than a year reduced the risk of ovarian cancer by 34 percent (361)Babic A, et al. (2020) JAMA Oncol, 6: e200421..
A full understanding of how oral contraceptive use, pregnancy, and breastfeeding influence the risk of female cancers is essential for developing effective risk-reduction interventions.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) refers to treatments that aim to relieve the common symptoms of menopause and the long-term biological changes, such as bone density loss, that take place after menopause. These changes occur owing to the decline in levels of the hormones estrogen and progesterone. HRT usually involves treatment with estrogen and progestin or estrogen alone in women who have undergone a hysterectomy, which is the surgery to remove all or part of the uterus. This approach is used because when estrogen is given alone, but not in combination with progestin, it is associated with an increased risk of endometrial cancer, a type of cancer that forms in the tissue lining of the uterus.
Data show that women who use the estrogen and progestin combination have an increased risk of developing breast cancer (363)Chlebowski RT, et al. (2020) JAMA, 324: 369.(364)Chlebowski RT, et al. (2008) Arch Intern Med, 168: 370.. The risk is greater with longer duration of use and is nearly two-fold higher among women who have used estrogen and progestin in combination for 10 years or longer compared to those who never used HRT (365)Chlebowski RT, et al. (2009) N Engl J Med, 360: 573.(366)Collaborative Group on Hormonal Factors in Breast Cancer. (2019) Lancet, 394: 1159.(367)Wang Y, et al. (2025) J Natl Cancer Inst, 117: 1260.. Women who are no longer using HRT have a lower risk than current users but remain at an elevated risk for more than a decade after they have stopped taking the drugs (366)Collaborative Group on Hormonal Factors in Breast Cancer. (2019) Lancet, 394: 1159.. Individuals who seek HRT should discuss with their health care providers the advantages and possible risks before deciding what is right for them.
One area of ongoing investigation in hormone replacement therapy is the differential cancer risks among individuals undergoing gender-affirming hormonal therapy (GAHT) (368)Jackson SS, et al. (2022) Trends Cancer, 8: 273.. Although current data are limited, emerging evidence suggests an increased risk of breast cancer—but a decreased risk of prostate cancer—among transgender women receiving GAHT, compared to age-matched cisgender men (369)de Blok CJM, et al. (2019) BMJ, 365: l1652.(370)de Nie I, et al. (2020) J Clin Endocrinol Metab, 105: e3293.. In contrast, transgender men who received testosterone for at least 5 years showed no increased risk of endometrial, ovarian, vaginal, or vulvar cancers (371)Vestering A, et al. (2025) EClinicalMedicine, 80: 103037.. While long-term follow-up studies are needed to more fully understand cancer risks in these understudied and medically underserved populations, current findings provide preliminary guidance for sexual and gender minority individuals considering GAHT (371)Vestering A, et al. (2025) EClinicalMedicine, 80: 103037..
Next Section: Cancer Screening for Early Detection Previous Section: Understanding the Path to Cancer Development