- Challenges Faced by Cancer Survivors
- Physical Challenges
- Psychosocial Challenges
- Financial Challenges
- Unique Challenges Faced by Older Adults
- Spotlight: Cancer Survivorship in Childhood and AYAs
- Challenges Faced by Childhood and AYA Cancer Survivors
- Promoting Health in Childhood and AYA Cancer Survivors
- Improving Health-related Quality of Life and Outcomes
- Participating in Physical Activity
- Eating a Healthy Diet and Maintaining a Healthy Weight
- Eliminating Alcohol and Tobacco Use
- Integrating Palliative Care
- Improving Mental Health
- Delivering Care to Cancer Survivors
- Supporting Caregivers
Supporting Cancer Patients and Survivors
In this section, you will learn:
- As of 2022, there were an estimated 18.1 million people living with a history of a cancer diagnosis.
- Cancer patients and survivors face a multitude of physical, emotional, and financial challenges because of their cancer and treatment.
- Childhood, adolescent, and young adult cancer survivors face unique challenges including long-term side effects from cancer and its treatments, difficulty finding work, lower levels of educational attainment, and psychosocial issues.
- Eating a healthy diet, reducing alcohol consumption and tobacco use, and exercising can improve the survivorship experience and outcomes.
- Caregivers of patients with cancer can face the same negative health and social consequences as the family members and loved ones they are caring for.
According to the National Cancer Institute (NCI), a person is considered a cancer survivor from the time of cancer diagnosis through the balance of the person’s life. Each person diagnosed with cancer has a unique experience ranging from successful treatment and living cancer free for the remainder of life to experiencing varying degrees of side effects to a subsequent cancer diagnosis with the same or a different type of cancer.
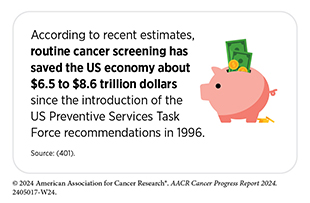
Unprecedented advances in cancer treatments over the past decade have led to more patients living longer and fuller lives after a cancer diagnosis. As of 2022, the most recent year for which such data are available, there were 18.1 million people living with a history of a cancer diagnosis, which equates to about 5 percent of the US population (9)Miller KD, et al. (2022) CA Cancer J Clin, 72: 409. DOI: 10.3322/caac.21731.. This is a significant improvement from 50 years ago when cancer survivors constituted only 1.4 percent of the US population. The number of survivors is expected to grow to 26 million by 2040 (9)Miller KD, et al. (2022) CA Cancer J Clin, 72: 409. DOI: 10.3322/caac.21731..
As more people are living longer and fuller lives after a cancer diagnosis, greater attention is needed to understand survivorship experiences. These experiences include the physical, psychosocial, and economic adversities caused by a cancer diagnosis. Cancer survivors are also at a risk for late effects or secondary health problems due to their cancer treatments and therefore require long-term follow-up care, which includes screening for these late effects. Survivorship care should include secondary cancer prevention counseling and assessment for short-term and late effects, including the increased risk of co-morbidities, recurrence, and development of secondary cancer
A diagnosis of cancer also impacts friends, family members, and caregivers, who are often the main support network for the survivor. This necessitates widening the focus of research, support, and care beyond the cancer patient and survivor to include individuals who make up the support structure,
The following sections highlight the challenges faced by cancer survivors and their support network, strategies to improve quality of life, and approaches that have been shown to deliver care most effectively.
Challenges Faced by Survivors
Cancer survivors often face physical, psychosocial, and financial challenges throughout their survivorship journey. Collectively these challenges contribute to the overall health-related quality of life (HRQOL) experienced by cancer survivors. Overall, HRQOL is lower among cancer survivors compared to those who have never had a diagnosis of cancer. Findings from a recent study show that cancer survivors with the lowest HRQOL were more likely to be unemployed, lacked social support, and were less prepared for survivorship. They also ate a less healthy diet and had more comorbidities, and were more concerned about the risk of cancer recurrence or secondary cancers (619)Manne S, et al. (2023) BMC Cancer, 23: 664. DOI: 10.1186/s12885-023-11098-5.. Cancer survivors also experience higher functional limitations, such as the inability to sit for extended periods of time or participate in social activities. The proportion of survivors who experience these limitations have doubled over the past two decades, with the highest prevalence among survivors of pancreatic cancer and lung cancer (620)Patel VR, et al. (2023) JAMA Oncol, 9: 1001. DOI: 10.1001/jamaoncol.2023.1180..
While research over the years has highlighted many of these challenges, implementation of groundbreaking new treatments such as immunotherapy and cell-based therapies can also present unique short- and long-term challenges. A greater understanding of these challenges and ways to address them is urgently required to support cancer survivors.
Physical Challenges
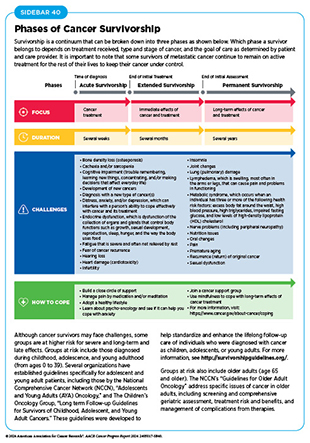
Survivors can experience a wide range of short- and long-term symptoms caused by cancer or its treatments. Short-term effects include hair loss, pain, nausea, vomiting, and loss of smell and appetite with varying severity of symptoms depending on the person, cancer type, and treatment. As cancer survivors are living longer, the development of long-term side effects such as heart damage (cardiotoxicity), lung damage, loss of bone density, and cognitive decline is becoming more common and demands a greater understanding to reduce or manage these conditions (see Sidebar 40).
Of primary concern for cancer survivors is the fear of cancer recurrence or the diagnosis of new cancers (621)Crist JV, et al. (2013) Psychooncology, 22: 978. DOI: 10.1002/pon.3114.(622)Zhang X, et al. (2022) Cancer Nurs, 45: 406. DOI: 10.1097/NCC.0000000000001020.. Rates of cancer recurrence or diagnosis of new cancers is dependent on many factors, including type and stage of cancer, the type of treatment received, and physical and socioeconomic factors. The chance of recurrence is higher for people treated for childhood cancers (see Cancer Survivorship in Childhood and AYAs) and adult survivors of Hodgkin lymphoma, glioblastoma, certain types of soft tissue sarcoma, bladder and pancreas cancer, and cancers caused by tobacco use (623)American Cancer Society. Cancer Treatment and Survivorship Facts and Figures 2022-2024. Accessed: July 10, 2024.. Primary cancers that are caught early have a lower risk of recurrence.
Cachexia is the loss of body weight and muscle mass, and the weakness that may occur in patients with cancer or other chronic diseases. Cachexia is estimated to occur in about 50 percent to 80 percent of patients with cancer and causes about 20 percent of cancer-related deaths (624)Mariean CR, et al. (2023) Cancers (Basel), 15: 5590. DOI: 10.3390/cancers15235590.. The development of cachexia results from multiple factors, including reduced nutrient intake while on active treatment, increased energy demand from cancer cells, reduced physical mobility of cancer patients, as well as inflammation associated with cancer and cancer treatments. Recent evidence has shown that patients with cancer who developed cachexia had higher rates of depression (30.2 percent), anxiety (18.6 percent), severe depression (6.7 percent), and severe anxiety (8.4 percent) compared to those who did not develop cachexia. Cancer survivors who developed cachexia also had lower overall HRQOL (625)Sun H, et al. (2023) BMJ Support Palliat Care, 13: e129. DOI: 10.1136/bmjspcare-2019-002176.. Understanding the biological underpinnings of cancer-related cachexia as well as developing novel therapeutic approaches that prevent cachexia is critical to reduce the loss of muscle mass in patients with cancer and improve their overall survival.
Chemotherapy-related cognitive impairment, often termed “chemo brain,” describes thinking and memory problems before, during, and after cancer treatment and has been reported by many cancer survivors (626)Fleming B, et al. (2023) BMJ, 380: e071726. DOI: 10.1136/bmj-2022-071726.. Cognitive impairment is very common among survivors of childhood cancer (see Cancer Survivorship in Childhood and AYAs). One meta-analysis estimated that chemotherapy-induced cognitive impairment was as high as 65 percent among breast cancer survivors (627)Kim HJ, et al. (2023) Cancer Nurs, 46: E159. DOI: 10.1097/NCC.0000000000001079.. Cognitive impairment among survivors also reduces their HRQOL (627)Kim HJ, et al. (2023) Cancer Nurs, 46: E159. DOI: 10.1097/NCC.0000000000001079.. It is critical that behavioral and therapeutic interventions be in place to reduce the effect of cognitive impairment on survivors.
Emerging evidence shows that cancer survivors have increased incidence of age-related diseases and faster functional decline compared to individuals who do not have a history of cancer (628)Kwan ML, et al. (2022) J Clin Oncol, 40: 1635. DOI: 10.1200/JCO.21.01738.(629)Greenlee H, et al. (2022) J Clin Oncol, 40: 1647. DOI: 10.1200/JCO.21.01736.(630)Hurria A, et al. (2019) J Am Geriatr Soc, 67: 920. DOI: 10.1111/jgs.15493.. This is partly due to changes at the molecular level as a result of certain types of cancer therapies. For instance, researchers who measured age-associated methylation marks on the DNA of women who had breast cancer and were treated with radiation found methylation patterns similar to those individuals who did not have a history of cancer but were much older (631)Kresovich JK, et al. (2023) J Natl Cancer Inst, 115: 1329. DOI: 10.1093/jnci/djad117.. Some examples of age-related diseases associated with cancer treatment include clinical hypertension, coronary artery disease, heart failure, and atrial fibrillation, arising from cardiotoxicity induced by certain types of anticancer therapeutics. In older adult cancer survivors, anti-hormonal treatments, such as tamoxifen, are associated with premature cognitive decline, while androgen deprivation therapy, primarily used to treat prostate cancer, is associated with increased risk of Alzheimer’s disease (632)Kerstens C, et al. (2023) Cancers (Basel), 15: 1215. DOI: 10.3390/cancers15041215..
Psychosocial Challenges
A diagnosis of cancer can pose serious challenges to a person’s psychosocial state and involves both psychological and social adversities. These challenges include uncertainty about the future and the possibility of cancer recurrence, isolation and lack of understanding by peers who do not have a history of a cancer diagnosis, returning to work, quality of care, and potential lack of support and coping strategies (633)R K, et al. (2024) J Cancer Surviv, 18: 84. DOI: 10.1007/s11764-023-01336-x..
According to a recent study in women with breast cancer, psychosocial well-being initially declined after diagnosis; however, their emotional functioning improved over time, with the greatest improvements among women who received breast reconstruction (634)Devarakonda SK, et al. (2023) BMC Womens Health, 23: 153. DOI: 10.1186/s12905-023-02243-0.. Side effects from cancer can also contribute to psychosocial challenges. For example, survivors of gynecologic cancers with lymphedema symptoms, i.e., swelling, numbness, and/or tingling near sites of surgery, had lower quality of life, greater psychosocial distress, and negative views of body image, compared to those without lymphedema symptoms (635)Koehler L, et al. (2023) Gynecol Oncol, 170: 254. DOI: 10.1016/j.ygyno.2023.01.019..
Financial Challenges
Financial toxicity refers to the financial hardship associated with cancer treatment and management. It is well established that cancer patients and survivors are at higher risk of experiencing financial difficulties compared to individuals without a history of cancer. One report estimates that more than 40 percent of cancer patients can spend their entire life savings within the first 2 years of cancer treatment (636)Gilligan AM, et al. (2018) Am J Med, 131: 1187. DOI: 10.1016/j.amjmed.2018.05.020.. The reported total out-of-pocket expenses for prostate cancer treatment ranged from $1700 to $3000. For many, this unexpected expense can lead to financial hardships and distress (637)Herrera CD, et al. (2023) Urol Oncol, 41: 105 e1. DOI: 10.1016/j.urolonc.2022.10.014..
Importantly, the cost of cancer does not end after the completion of treatment. Post-treatment costs include managing the late and long-term effects of cancer and its treatments, mental health care, and treatment of secondary cancers.
Evidence indicates that cancer survivors who experience financial toxicity and subsequently have difficulty paying for prescriptions, mental health care, and other health services, and/or who delay medical care due to cost, are also at greater risk of mortality, regardless of insurance status (639)Yabroff KR, et al. (2022) J Natl Cancer Inst, 114: 863. DOI: 10.1093/jnci/djac044.. To mitigate these financial challenges, survivors often utilize coping behaviors. These include medication underuse or skipping medication doses; cutting back on spending, including for essential items, such as food; and missing payments, including for rent or a mortgage (640)Doherty M, et al. (2021) Support Care Cancer, 29: 5753. DOI: 10.1007/s00520-021-06113-z..
Exacerbating financial toxicity among survivors is the inability to continue working or, after the conclusion of treatment, returning to a previous job. The type of work that a person does prior to their cancer diagnosis also impacts their ability to retain a job or return after treatment concludes. In a study of rural women cancer survivors, those who had less secure jobs, including temporary, part-time, or non-traditional jobs, were less likely to return to work compared to those with secure employment (641)Hallgren E, et al. (2023) J Cancer Surviv, 17: 1338. DOI: 10.1007/s11764-022-01179-y.. This is concerning because research shows that being employed improved HRQOL among cancer survivors (642)Andreu Y, et al. (2023) Health Qual Life Outcomes, 21: 44. DOI: 10.1186/s12955-023-02124-y.. To ensure job security among cancer survivors during and after treatment, employers should create policies, such as modifying the demands of the work environment, in consultation with employees and their health care providers to accomodate the unique needs and challenges faced by cancer survivors.
Unique Challenges Faced by Older Adults
Older adults are defined as those age 65 and over, representing 64 percent of cancer survivors in the United States. This population is also the fastest growing and is projected to increase to 73 percent of cancer survivors by 2040 (643)Mohile SG, et al. (2016) Cancer, 122: 2459. DOI: 10.1002/cncr.30053..
Older cancer patients are susceptible to being malnourished, which can exacerbate muscle wasting (sarcopenia) and weight loss due to cancer (cachexia). One study found that among older adults with cancer, 60 percent were malnourished, 53.3 percent had sarcopenia, and 56.7 percent had cachexia, with 30 percent of adult cancer survivors having all three conditions together (644)Bullock AF, et al. (2024) Eur J Clin Nutr, 78: 486. DOI: 10.1038/s41430-024-01433-9.. These side effects often stem from decreased nutrient intake. The use of certain drugs that improve appetite has been shown to help increase nutritional intake; however, these can also lead to gastrointestinal and cardiovascular complications (645)Ispoglou T, et al. (2024) Clin Nutr, 43: 552. DOI: 10.1016/j.clnu.2024.01.009.. Other strategies have been explored, such as the use of probiotics and low-dose olanzapine, which have shown some promise in boosting survivors’ appetites and reducing weight loss among cancer patients on active treatment (645)Ispoglou T, et al. (2024) Clin Nutr, 43: 552. DOI: 10.1016/j.clnu.2024.01.009.(646)Rodriguez-Arrastia M, et al. (2021) Int J Environ Res Public Health, 18: 4265. DOI: 10.3390/ijerph18084265.(647)Hutchinson AN, et al. (2021) Microorganisms, 9: 1344. DOI: 10.3390/microorganisms9061344..
Although the evidence is still scarce, older adults are also susceptible to adverse mental health events. Of particular concern among this population is loneliness, with some estimates showing that up to 50 percent of older adults experience loneliness (648)Pilleron S, et al. (2023) J Geriatr Oncol, 14: 101519. DOI: 10.1016/j.jgo.2023.101519.. Furthermore, other adverse mental health events, including depression and anxiety, are exacerbated by loneliness (648)Pilleron S, et al. (2023) J Geriatr Oncol, 14: 101519. DOI: 10.1016/j.jgo.2023.101519.. This is concerning because some evidence suggests loneliness among cancer survivors over the age of 50 reduces HRQOL and nearly doubles the risk of mortality (649)Zhao J, et al. (2023) J Clin Oncol, 41: 6531. DOI: 10.1200/JCO.2023.41.16_suppl.6531.. Interventions to reduce loneliness and improve HRQOL among this population include social support, telehealth strategies, and other types of counseling (650)McElfresh JJ, et al. (2021) J Psychosoc Oncol, 39: 509. DOI: 10.1080/07347332.2020.1867690..
As older cancer survivors often have other pre-existing chronic conditions that require regular medication, adding a cancer therapeutic after a diagnosis of cancer can lead to “polypharmacy,” which has been associated with numerous adverse outcomes. Polypharmacy can lead to drug-drug interactions, faster functional decline, falls, hospitalizations, and mortality in older adults (651)Davies LE, et al. (2020) J Am Med Dir Assoc, 21: 181. DOI: 10.1016/j.jamda.2019.10.022.(652)Dhalwani NN, et al. (2017) BMJ Open, 7: e016358. DOI: 10.1136/bmjopen-2017-016358.(653)Jensen GL, et al. (2001) Am J Clin Nutr, 74: 201. DOI: 10.1093/ajcn/74.2.201.(654)Chang TI, et al. (2020) Sci Rep, 10: 18964. DOI: 10.1038/s41598-020-75888-8.(655)Leelakanok N, et al. (2017) J Am Pharm Assoc (2003), 57: 729. DOI: 10.1016/j.japh.2017.06.002.(656)Maggiore RJ, et al. (2010) Oncologist, 15: 507. DOI: 10.1634/theoncologist.2009-0290.(657)Lu-Yao G, et al. (2020) J Geriatr Oncol, 11: 579. DOI: 10.1016/j.jgo.2020.03.001.. The issue is exacerbated when physicians prescribe more medications to counteract the symptoms of polypharmacy. One study of older adult cancer survivors found that 61.3 percent of these individuals were being given five or more medications, with 14.5 percent who were being given 10 or more (658)Ramsdale E, et al. (2022) Oncologist, 27: e580. DOI: 10.1093/oncolo/oyac053.. Of those who were considered to have polypharmacy, 67.1 percent experienced at least one adverse reaction between their cancer drug and other medications they were taking (658)Ramsdale E, et al. (2022) Oncologist, 27: e580. DOI: 10.1093/oncolo/oyac053..
Older adult cancer survivors are also susceptible to financial challenges. While most older adults have insurance, the financial burden of cancer can continue long after conclusion of treatment (659)Shih YT, et al. (2022) J Natl Cancer Inst, 114: 1020. DOI: 10.1093/jnci/djac064.(660)Bradley CJ, et al. (2024) J Cancer Surviv, 18: 499. DOI: 10.1007/s11764-022-01248-2.. After diagnosis, older adults that received a diagnosis of cancer incurred more consumer debt compared to those without a diagnosis of cancer (34.5 vs. 29.9 percent) that persisted 2 years after (659)Shih YT, et al. (2022) J Natl Cancer Inst, 114: 1020. DOI: 10.1093/jnci/djac064..

Cancer Survivorship in Childhood and AYAs
Childhood and adolescent and young adult (AYA) cancer survivors face unique challenges compared to their peers who have never had a diagnosis of cancer. These challenges include long and late-term side effects from cancer and its treatment, financial toxicity, difficulty finding work, lower levels of educational attainment, psychosocial issues, and others. Because of the unique challenges faced by this population, researchers and care providers must pay special attention to ensure the needs of this population are adequately addressed across the spectrum of cancer care.
Challenges Faced by Childhood and AYA Cancer Survivors
In the United States in 2024, an estimated 9,620 new cases of cancer will be diagnosed among children. Thanks to major treatment advances, 85 percent of children are expected to live 5 years or more after a cancer diagnosis. This is a marked improvement compared to the mid-1970s, when only 42 percent of children lived beyond 5 years after a cancer diagnosis (661)Siegel RL, et al. (2021) CA Cancer J Clin, 71: 7. DOI: 10.3322/caac.21654.. Because childhood cancer survivors are diagnosed at a young age, they live longer postdiagnosis than an adult who has been diagnosed with cancer later in life.
Due to this longer lifespan, childhood cancer survivors are more susceptible to late-stage side effects for a variety of reasons, including the type and stage of cancer at the time of diagnosis, the type and dose of treatment, and the age and general health of the patient at the time of treatment. Reports indicate that 60 to 90 percent of childhood survivors develop one or more chronic health conditions following their cancer diagnosis (662)Armstrong GT, et al. (2014) J Clin Oncol, 32: 1218. DOI: 10.1200/Jco.2013.51.1055.(663)Hudson MM, et al. (2013) JAMA, 309: 2371. DOI: 10.1001/jama.2013.6296..
Childhood cancer survivors are at an increased risk of developing a new cancer due to late effects of cancer treatment and/or inherited genetic factors (657)Lu-Yao G, et al. (2020) J Geriatr Oncol, 11: 579. DOI: 10.1016/j.jgo.2020.03.001.. Additionally, children with a cancer diagnosis who receive chemotherapeutics are at an increased risk of developing hearing loss, also called ototoxicity. One study found that 75 percent of children under 5 and 48 percent of children over 5 who were treated with cisplatin had hearing loss related to their treatment (664)Meijer AJM, et al. (2022) Cancer, 128: 169. DOI: 10.1002/cncr.33848.. In September 2022, the US Food and Drug Administration (FDA) approved sodium thiosulfate to reduce the risk of hearing loss associated with the chemotherapeutic cisplatin in childhood patients with cancer 1 month and older. Sodium thiosulfate reduced the risk of cisplatin-associated hearing loss by almost 60 percent compared to those who did not receive the drug (665)Schulte F, et al. (2022) JAMA Netw Open, 5: e2227225. DOI: 10.1001/jamanetworkopen.2022.27225.. Long-term survivors of childhood cancer are also at an elevated risk for late-onset cognitive impairment, which are declines in memory, thinking, and psychomotor tasks. In one study of childhood cancer survivors, researchers found that memory impairment was as much as 34 percent higher in survivors who were treated for cancers of the central nervous system, compared to siblings who did not undergo cancer treatment (666)Phillips NS, et al. (2023) JAMA Netw Open, 6: e2316077. DOI: 10.1001/jamanetworkopen.2023.16077..
Premature aging, which refers to the early onset of aging-related health issues, is common among childhood cancer survivors (667)Kruseova J, et al. (2023) Oncol Lett, 25: 43. DOI: 10.3892/ol.2022.13629.. These include chronic conditions such as cardiovascular disease, endocrinopathies, and other cancers. According to one study, daily functional limitations, psychosocial symptoms, and health conditions of a 30-year-old survivor of a childhood cancer are similar to those of a 63-year-old healthy individual (668)Williams AM, et al. (2023) J Natl Cancer Inst, 115: 200. DOI: 10.1093/jnci/djac209..
Adolescent and young adult (AYA) cancer survivors are those diagnosed between the ages of 15 and 39. Based on estimates of new cancer cases in 2024, 4.2 percent of all new cases will be in AYA and 85.9 percent of AYAs diagnosed with cancer will live 5 years or more after their diagnosis (3)NCI Surveillance, Epidemiology, and End Results Program. NCI SEER*Explorer. Accessed: March 17, 2024.. This population group faces unique personal, social, and emotional challenges as highlighted in the personal story of Lourdes Monje.
Many AYA survivors experience long-term side effects and are at a two- to three-fold higher risk of premature ovarian failure, chronic liver disease, renal failure, and cardiovascular disease, compared to those with no diagnosis of cancer (670)Chao C, et al. (2020) J Clin Oncol, 38: 3161. DOI: 10.1200/Jco.20.00722.. A recent study reported that 40 percent of AYA survivors had more than one chronic condition (e.g., cardiomyopathy, hearing loss, stroke, diabetes) 10 years after their cancer diagnosis, compared to only 20 percent of those who did not have cancer (670)Chao C, et al. (2020) J Clin Oncol, 38: 3161. DOI: 10.1200/Jco.20.00722..
Similar to childhood cancer survivors, AYA cancer survivors also have a higher risk of secondary cancer, which is partly due to premature aging (671)Chao C, et al. (2019) JAMA Netw Open, 2: e195536. DOI: 10.1001/jamanetworkopen.2019.5536.(672)Bright CJ, et al. (2019) Lancet Oncol, 20: 531. DOI: 10.1016/S1470-2045(18)30903-3.(673)van der Meer DJ, et al. (2024) Oncologist, 29: e526. DOI: 10.1093/oncolo/oyad307.. AYA cancer survivors are twice as likely to die from the development of a new primary cancer as those who have never had a diagnosis of cancer (674)Sung H, et al. (2022) J Natl Cancer Inst, 114: 1095. DOI: 10.1093/jnci/djac091..
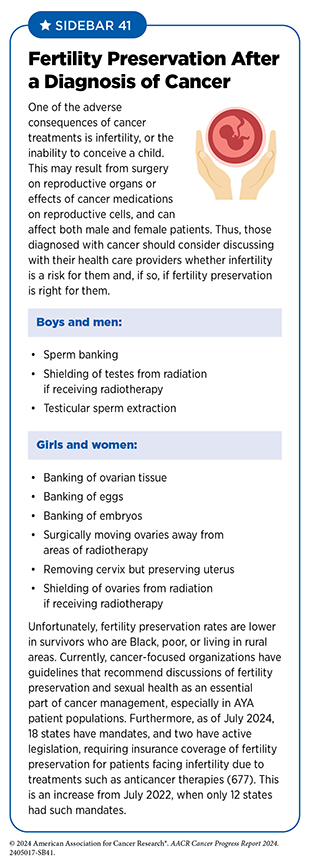
Between 44 percent and 86 percent of AYA survivors have concerns regarding how treatments for cancer, including surgery, radiotherapy, and cytotoxic chemotherapy, may lead to infertility, which is the inability to conceive a child (676)Xie J, et al. (2022) Cancer Med, 11: 3508. DOI: 10.1002/cam4.4708.. The possibility of impaired reproductive abilities may lead some patients to store reproductive material through the process of fertility preservation (see Sidebar 41). Participation in fertility preservation and the type of preservation should be decided by individuals after discussions with their health care providers.
Intrathecal therapies in children, for instance in children treated with methotrexate for medulloblastoma, can lead to impairments in cognition, executive functioning and short-term memory (678)Riva D, et al. (2002) Neurology, 59: 48. DOI: 10.1212/wnl.59.1.48.. AYA survivors also experience cancer-related cognitive impairment, which is more common in survivors of central nervous system cancers, Hodgkin lymphoma, and testicular and breast cancers (679)McGrady ME, et al. (2024) J Clin Oncol, 42: 707. DOI: 10.1200/JCO.23.01465.. Although research in cancer-related cognitive impairment among AYA is lacking, it has been estimated that 22 percent of AYA cancer survivors experience problems with memory (680)Prasad PK, et al. (2015) J Clin Oncol, 33: 2545. DOI: 10.1200/JCO.2014.57.7528..
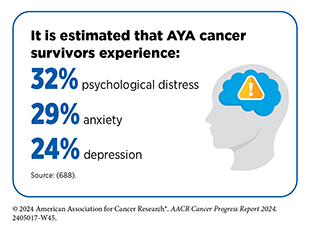
The psychosocial impact of a cancer diagnosis on a child can be traumatizing and have a lasting effect on the mental health of childhood survivors of cancer. Research on the social aspects of cancer in children have shown that they harbor negative perceptions of their appearance, leading to problems with academics, social interactions, and psychological well-being, resulting in low self-esteem and depression, all of which can be exacerbated by bullying and ridicule from peers(681)O’Donnell N, et al. (2024) BMJ Open, 14: e082779. DOI: 10.1136/bmjopen-2023-082779.(682)Fuemmeler BF, et al. (2002) Clin Psychol Rev, 22: 547. DOI: 10.1016/s0272-7358(01)00120-9.(683)Currier JM, et al. (2009) J Trauma Stress, 22: 28. DOI: 10.1002/jts.20382..
The quality of mental health among survivors of childhood cancers is also concerning. When compared to their healthy siblings, young adult survivors of childhood cancers reported increased loneliness that subsequently increased anxiety, depression, and the likelihood of smoking. Long-term follow-up with these patients found higher levels of suicidal thoughts, as well as heavy/risky alcohol consumption (684)Papini C, et al. (2023) Cancer, 129: 1117. DOI: 10.1002/cncr.34633.. This population is also more susceptible to major mental health illnesses, including autism, attention-deficit disorder, bipolar disorder, major depressive disorder, obsessive-compulsive disorder, and posttraumatic stress disorder, with the greatest number of mental health illnesses experienced by survivors of brain and blood cancers (685)Hsu TW, et al. (2023) J Clin Oncol, 41: 2054. DOI: 10.1200/Jco.22.01189..
Similar to survivors of childhood cancers, AYA cancer survivors also have worse mental health outcomes compared to those without a diagnosis of cancer. AYA cancer survivors had an 80 percent increased risk of hospitalizations for mental health illnesses and were 4.5 times more likely to purchase antidepressants compared to their siblings (686)Ryder-Burbidge C, et al. (2021) Cancers (Basel), 13: 4870. DOI: 10.3390/cancers13194870.(687)Berkman AM, et al. (2023) J Natl Cancer Inst, 115: 447. DOI: 10.1093/jnci/djac206..
Financial toxicity is prevalent among survivors of childhood cancer (689)Nathan PC, et al. (2023) J Clin Oncol, 41: 1000. DOI: 10.1200/JCO.22.00572.. The reasons for financial toxicity among this population are multifaceted and include continuing medical expenses associated with long- and late-term side effects; difficulty finding and retaining employment because of cancer- and treatment-related disabilities; and lower-paying jobs, partially as a result of lower educational attainment (690)Fauer AJ, et al. (2024) JNCI Cancer Spectr, 8: pkae033. DOI: 10.1093/jncics/pkae033.(691)Bhatt NS, et al. (2024) JAMA Netw Open, 7: e2410731. DOI: 10.1001/jamanetworkopen.2024.10731.(692)Ruiz S, et al. (2023) Pediatrics, 152: e2022059951. DOI: 10.1542/peds.2022-059951.(693)Kyronlahti A, et al. (2023) Cancer Med, 12: 16455. DOI: 10.1002/cam4.6218..
Also concerning is the decline in employment among childhood cancer survivors over time, with full- or part-time employment declining by 6.5 percent and 8 percent among female and male childhood cancer survivors, respectively, over 10 years after diagnosis (691)Bhatt NS, et al. (2024) JAMA Netw Open, 7: e2410731. DOI: 10.1001/jamanetworkopen.2024.10731..
Financial toxicity among AYA cancer survivors is also higher compared to those with no diagnosis of cancer (695)Di Giuseppe G, et al. (2023) Crit Rev Oncol Hematol, 183: 103914. DOI: 10.1016/j.critrevonc.2023.103914.. One study reported that the costs associated with a diagnosis of cancer are substantial, reaching an average of $259,324 per person over their lifetime (64)Parsons SK, et al. (2023) J Clin Oncol, 41: 3260. DOI: 10.1200/JCO.22.01985.. One reason is that a cancer diagnosis often affects these individuals when they are just beginning higher levels of education or starting careers, potentially impacting productivity and well-being (64)Parsons SK, et al. (2023) J Clin Oncol, 41: 3260. DOI: 10.1200/JCO.22.01985..
In one study, researchers examined how a diagnosis of cancer as an AYA led to hardships into adulthood across three domains, which were material (e.g., paying bills, medical care), psychological (e.g., distress), and behavioral (forgoing medical care). Those adults with a diagnosis of cancer as an AYA were 38 percent more likely to report hardship across all three domains compared to those without a diagnosis of cancer as AYA (696)Lu AD, et al. (2021) J Natl Cancer Inst, 113: 997. DOI: 10.1093/jnci/djab013..
As childhood and AYA survivors of cancer are living longer, thanks to improved treatments, greater attention should be given to follow-up care and continued surveillance strategies should be implemented for cancer recurrence or the development of new cancers. A particular concern is that medical records may not be transferred when childhood cancer survivors grow up and transition to adult health care settings (697)Ryan D, et al. (2021) CMAJ Open, 9: E309. DOI: 10.9778/cmajo.20200134.. The Childhood Cancer STAR Reauthorization Act was signed into law in January 2023, reauthorizing the program for an additional 5 years at its fully authorized level of $30 million. This legislation hopes to not only improve treatments for childhood and AYA cancer survivors, but also improve cancer surveillance, and enhance resources for survivors and families (see Accelerating Progress Against Childhood Cancer) (698)National Cancer Institute. Division of Cancer Control and Population Sciences. Pediatric and Adolescent and Young Adult (AYA) Cancer Survivorship. Accessed: July 31, 2024..
Health care systems, policymakers, and other stakeholders must recognize the adverse effects of financial toxicity among AYA cancer survivors to design interventional strategies necessary to address the underlying causes.
Promoting Health in Childhood and AYA Cancer Survivors
A healthy diet, maintaining a healthy weight, and regular exercise are important for any child or AYA to stay healthy and curtail obesity, while AYA populations should abstain from smoking cigarettes and tobacco, as well as limit alcohol consumption. For children and AYA individuals who receive a cancer diagnosis, adhering to a healthy diet and exercise can be a challenge. A key focus for these patients should be not only maintaining a healthy weight and participating in regular physical activity but also escalating these goals for continued growth and development. One of the side effects that accompany cancer is a lack of appetite, which can lead to unintended weight loss. Studies show that higher treatment intensities among children with cancer increase the likelihood of weight loss, especially in younger children (699). Studies have shown that a registered dietitian or nutritionist, who can intervene before, during, and after treatment, can help children stay on a healthy diet and maintain weight (700)Napartuk M, et al. (2023) Children (Basel), 10: 667. DOI: 10.3390/children10040667..
Eating a healthy diet, particularly one based on fruits, vegetables, and whole grains and low in processed foods and red meats, can reduce long-term side effects and mortality from cancer. In long-term studies of survivors of childhood cancers, individuals who consumed dark green vegetables and nuts/seeds saw a reduction in premature aging (701)Wang M, et al. (2024) J Clin Oncol, 42: 1553. DOI: 10.1200/JCO.23.01260.. Strategies that increase consumption of healthy foods are paramount to reducing the development of chronic conditions, obesity, and adverse side effects among AYA cancer survivors.
Exercise can help survivors of childhood and AYA cancer minimize adverse long-term outcomes, such as chronic health conditions, and treatment-related side effects (702)Munsie C, et al. (2022) Support Care Cancer, 30: 8159. DOI: 10.1007/s00520-022-07217-w.(703)Zhi X, et al. (2019) Integr Cancer Ther, 18: 1534735419895590. DOI: 10.1177/1534735419895590.. Although data are limited in this area, interventions that are digitally based worked best for these individuals (704)Vasilopoulou M, et al. (2024) Support Care Cancer, 32: 342. DOI: 10.1007/s00520-024-08516-0.. Among AYA cancer survivors, participating in moderate- to vigorous-intensity physical activity led to a 40 percent reduction in cardiovascular disease, a common chronic condition among this population (705)Berkman AM, et al. (2023) Cancer, 129: 450. DOI: 10.1002/cncr.34505.. Designing interventions that help children and AYA individuals with a history of a cancer diagnosis maintain the recommended physical activity guidelines is necessary to reduce the adverse effects of cancer in these populations (see Sidebar 11).
Smoking among cancer survivors is associated with poor outcomes and greater treatment-related complications, higher risk of secondary cancers, lower HRQOL, and greater mortality (706)Centers for Disease Control and Prevention. The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General. Accessed: July 6, 2024.(707)Nolazco JI, et al. (2023) Front Oncol, 13: 1261041. DOI: 10.3389/fonc.2023.1261041.. It is therefore concerning that an estimated 20 percent to 22 percent of survivors of pediatric cancer smoke (708)Gibson TM, et al. (2015) Cancer, 121: 4035. DOI: 10.1002/cncr.29609.(709)Marjerrison S, et al. (2016) Pediatr Blood Cancer, 63: 1254. DOI: 10.1002/pbc.25943. and 33 percent of AYA cancer survivors smoke (710)Kaul S, et al. (2016) Cancer, 122: 2895. DOI: 10.1002/cncr.30086.. Evidence regarding interventional strategies that are directed toward childhood or AYA cancer survivors is insufficient. Cessation strategies that are tailored to the unique needs of this population are necessary to reduce the burden of smoking among this population.
Mental health care among childhood and AYA cancer patients and survivors requires collaboration among health professionals, school administrators, parents, and survivors. Because cancer is rare in children, there is a dearth of widespread policies and procedures to effectively deal with a diagnosis of cancer. However, a few strategies can be employed to help this population find the support they need to help deal with a cancer diagnosis (see Sidebar 42).
The challenges in those aged 40 to 49 are of increasing concern because cases of early-onset cancers in this age group are rising compared to early-onset cancers in younger ages. Like survivors of other ages, this population faces similar challenges including reduced quality of life, sexual dysfunction, negative body image, financial and career impacts, and social and family impacts (712)Waddell O, et al. (2023) BJS Open, 7. DOI: 10.1093/bjsopen/zrad030..
Improving Health-related Quality of Life and Outcomes
Healthy behaviors, such as physical activity, a healthy diet, reduced alcohol consumption, and smoking cessation, can significantly improve both health outcomes and HRQOL for cancer survivors. In fact, it is increasingly appreciated that adopting healthy behaviors after a diagnosis of cancer, but prior to beginning cancer treatment, can significantly improve outcomes for patients (713)Giles C, et al. (2019) BMJ, 366: l5120. DOI: 10.1136/bmj.l5120.(714)Molenaar CJL, et al. (2023) JAMA Surg, 158: 572. DOI: 10.1001/jamasurg.2023.0198.. A patient who is healthy at the start of treatment can undergo treatment with higher doses of drug, is less susceptible to certain side effects, and has an immune system that is primed to fight cancer better (715)Loewen I, et al. (2021) J Otolaryngol Head Neck Surg, 50: 2. DOI: 10.1186/s40463-020-00486-7..
Participating in Physical Activity
Physical activity has been shown to increase survival and lower recurrence of cancers (716)Brown JC, et al. (2023) Br J Sports Med, 57: 965. DOI: 10.1136/bjsports-2022-106445.(717)Lavery JA, et al. (2023) J Clin Oncol, 41: 4982. DOI: 10.1200/JCO.23.00058.. Research shows that cancer patients and survivors who participated in the recommended physical activity guidelines (see Sidebar 11) had lowered rates of mortality compared to those who did not participate in physical activities (718)Kenfield SA, et al. (2023) J Clin Oncol, 41: 4965. DOI: 10.1200/JCO.23.01528.. Emerging evidence suggests that physical activity can improve the immune system’s ability to detect and remove cancer cells (719)Deng N, et al. (2023) Clin Cancer Res, 29: 4361.. This can be beneficial to individuals who are predisposed to cancer, such as patients with Lynch syndrome, who develop certain types of cancers, including colorectal cancer, more frequently than those without Lynch syndrome (719)Deng N, et al. (2023) Clin Cancer Res, 29: 4361.. With a more active and effective immune system, pre-cancerous cells that are more common in patients with Lynch syndrome can be intercepted before they develop into cancer.
Other types of interventions such as low-impact, meditative movement can improve outcomes among cancer patients and survivors (721)Soltero EG, et al. (2023) J Cancer Surviv: 10.1007/s11764. DOI: 10.1007/s11764-023-01430-0.(722)Buro AW, et al. (2023) Int J Environ Res Public Health, 20: 3355. DOI: 10.3390/ijerph20043355.. Mindfulness interventions can also reduce the severity of cognitive impairment among cancer survivors (723)Melis M, et al. (2023) Cancer, 129: 1105. DOI: 10.1002/cncr.34640.(724)Melis M, et al. (2023) Cancers (Basel), 15: 3632. DOI: 10.3390/cancers15143632.(725)Melis M, et al. (2023) J Cancer Surviv: 10.1007/s11764. DOI: 10.1007/s11764-023-01484-0.. Mind-body interventions, for example yoga, which are often low impact, can also help cancer patients and survivors transition into more physically strenuous exercises (721)Soltero EG, et al. (2023) J Cancer Surviv: 10.1007/s11764. DOI: 10.1007/s11764-023-01430-0..
Eating a Healthy Diet and Maintaining a Healthy Weight
Consuming a healthy diet that incorporates whole grains, fruits, and vegetables can increase survival from cancer and reduce the risk of cancer recurrence (726)Morice P, et al. (2012) Lancet, 379: 558. DOI: 10.1016/S0140-6736(11)60829-5.. In fact, it has been reported that eating a healthy diet can lower overall mortality and cancer-specific mortality by 20 percent and 14 percent, respectively, in an analysis of cancer survivors globally (727)Trauchburg A, et al. (2023) Nutrients, 15: 3151. DOI: 10.3390/nu15143151..
Plant-based diets reduce mortality among cancer patients and lead to weight loss and improved cardiovascular health (728)Wang DD, et al. (2022) Public Health Nutr, 26: 381. DOI: 10.1017/S1368980022000659.(729)Campbell TM, et al. (2024) Breast Cancer Res Treat, 205: 257. DOI: 10.1007/s10549-024-07266-1.. Certain diets that emphasize plants and healthy fats, such as the Mediterranean diet, have been associated with reduced overall mortality in cancer patients and survivors (730)Chen G, et al. (2023) Nutrients, 15. DOI: 10.3390/nu15092099.(731)Monllor-Tormos A, et al. (2023) Maturitas, 178: 107841. DOI: 10.1016/j.maturitas.2023.107841.(732)Castro-Espin C, et al. (2023) BMC Med, 21: 225. DOI: 10.1186/s12916-023-02934-3.(733)Pavlidou E, et al. (2023) Med Sci (Basel), 11: 74. DOI: 10.3390/medsci11040074..
Conversely, consumption of unhealthy foods such as ultra-processed products, red meat, and sugar-sweetened beverages increased fatigue and chemotherapy-induced peripheral neuropathy while reducing HRQOL among cancer survivors (734)Kenkhuis MF, et al. (2023) Br J Nutr, 130: 114. DOI: 10.1017/S0007114522003051.(735)Davis EW, et al. (2023) Nutrients, 15: 275. DOI: 10.3390/nu15020275..
Emphasizing a healthier diet can help improve HRQOL, reduce side effects, and decrease mortality in cancer patients and survivors. Interventions that improve access to these types of foods while lowering their cost, especially because of financial concerns among cancer patients and survivors, are paramount to improving outcomes among these populations.
Eliminating Alcohol and Tobacco Use
It has been estimated that 1.4 percent of adult cancer survivors smoked cigarettes in 2022 (265)Centers for Disease Control and Prevention. National Health Interview Survey. Accessed: July 5, 2023.. Smoking among cancer survivors is associated with poor outcomes and greater treatment-related complications, higher risk of secondary cancers, lower HRQOL, and greater mortality (706)Centers for Disease Control and Prevention. The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General. Accessed: July 6, 2024.(707)Nolazco JI, et al. (2023) Front Oncol, 13: 1261041. DOI: 10.3389/fonc.2023.1261041.. Cigarette smoking is also associated with greater cancer-related symptoms including fatigue, pain, and emotional problems among adults with cancer (736)Price SN, et al. (2023) Cancer, 129: 2385. DOI: 10.1002/cncr.34746..
The use of e-cigarettes among cancer survivors has been on the rise. In 2017, 10.7 percent of cancer survivors used e-cigarettes compared to only 8.5 percent in 2014 (737)Bjurlin MA, et al. (2022) Cancer Epidemiol, 78: 102037. DOI: 10.1016/j.canep.2021.102037.. Currently, the rates of e-cigarette use among cancer survivors are estimated at 15 percent in 2024, with 63 percent of survivors who smoke traditional cigarettes also using e-cigarettes (738)Lopez-Olivo MA, et al. (2024) J Cancer Surviv, 18: 1059. DOI: 10.1007/s11764-023-01357-6..
Smoking cessation can have immediate and long-term positive effects for cancer survivors. For instance, after smoking cessation, researchers observed a dramatic change in the immune properties of cancer patients and survivors toward a non–cancer-promoting profile (739)Lu Y, et al. (2023) Sci Rep, 13: 2745. DOI: 10.1038/s41598-023-27624-1..
It is concerning that cancer patients who are on active treatment are less likely to stop smoking or abstain from it, compared to those who have completed treatment (740)Cottrell-Daniels C, et al. (2024) Am J Prev Med, 66: 1049. DOI: 10.1016/j.amepre.2024.02.004.. Decreasing dependence on smoking traditional cigarettes and e-cigarettes through smoking cessation programs can help to alleviate the increased burden that comes from using these products. Smoking cessation programs that include both behavioral counseling and pharmacologic interventions have been shown to be the most effective in reducing smoking among cancer survivors (741)Yingst JM, et al. (2023) Psychooncology, 32: 1147. DOI: 10.1002/pon.6171.. Further research is needed to identify effective methods to help cancer patients and survivors reduce dependence on tobacco products.
Consumption of alcohol can lead to adverse health and treatment outcomes among cancer patients and survivors, including increasing the risk of cancer recurrence. Unfortunately, 77.7 percent of individuals with a history of cancer report consuming alcohol (742)Shi M, et al. (2023) JAMA Netw Open, 6: e2328328. DOI: 10.1001/jamanetworkopen.2023.28328.. Among those who drink, 23.8 percent engage in binge drinking (greater than 6 drinks in one sitting), whereas 38.3 percent engage in hazardous drinking, as measured by the Alcohol Use Disorders Identification Test (742)Shi M, et al. (2023) JAMA Netw Open, 6: e2328328. DOI: 10.1001/jamanetworkopen.2023.28328.. While there are few interventions specifically developed for cancer survivors, cancer care providers should refer their patients with alcohol use disorder to evidence-based treatments, including behavioral counseling and/or pharmacotherapy, that have been developed for general populations. As heavy drinking among this population is associated with poor mental health and posttraumatic stress disorder, addressing the root causes of drinking is necessary. More research on intervention strategies specifically to reduce alcohol abuse in cancer survivors is warranted.
Integrating Palliative Care
Palliative care is an approach to prevent or treat the symptoms and side effects of any disease, including cancer, by addressing the physical, psychosocial, financial, and spiritual needs that arise from the disease and treatments (see Sidebar 43). Palliative care is facilitated by multidisciplinary teams of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers and has been shown to improve quality of life for patients, families, and caregivers (743)Radbruch L, et al. (2020) J Pain Symptom Manage, 60: 754. DOI: 10.1016/j.jpainsymman.2020.04.027..
Research shows that palliative care approaches improve pain management and reduce depression and functional limitations, improving the survivorship experience (744)Morgan B, et al. (2023) Curr Probl Cancer, 47: 101019. DOI: 10.1016/j.currproblcancer.2023.101019..
Cancer-focused organizations recommend integrating palliative care services early on in treatment (745)Sanders JJ, et al. (2024) J Clin Oncol: JCO2400542. DOI: 10.1200/JCO.24.00542.(746)Smith CB, et al. (2017) Am Soc Clin Oncol Educ Book, 37: 714. DOI: 10.1200/EDBK_175474.(747)Dans M, et al. (2021) J Natl Compr Canc Netw, 19: 780. DOI: 10.6004/jnccn.2021.0033.. This ensures that the physical, psychosocial, and/or spiritual concerns of patients are addressed early, reducing negative outcomes and improving HRQOL.
Improving Mental Health
The psychological challenges faced by survivors of cancer necessitate approaches that improve the mental well-being of this population (see Challenges Faced by Survivors). Several approaches can be utilized, including mind-body interventions, support groups, improved mental health screening, physical activity, and community engagement (748)Liska TM, et al. (2020) Health Qual Life Outcomes, 18: 197. DOI: 10.1186/s12955-020-01448-3.(749)Shani P, et al. (2022) Integr Cancer Ther, 21: 15347354221103275. DOI: 10.1177/15347354221103275.(750)Smith SK, et al. (2018) Am Soc Clin Oncol Educ Book, 38: 813. DOI: 10.1200/EDBK_201307.(751)Flores NJ, et al. (2021) Cureus, 13: e14158. DOI: 10.7759/cureus.14158..
One approach is the use of “stepped care,” which consistently evaluates how a patient is responding to both psychotherapy and medication every few weeks, emphasizing individualized treatment plans tailored for each patient. In one clinical trial that looked at outcomes of patients who participated in a stepped care program, researchers found that compared to those in a standard care group, patients in the stepped care model had more clinically meaningful improvements in HRQOL (752)Steel JL, et al. (2024) Lancet, 403: 1351. DOI: 10.1016/S0140-6736(24)00015-1.. This clinical trial also found that health care systems benefit from providing stepped care at no cost to the patient, as underscored by the findings that this type of intervention led to savings of $16,000 per patient per year. This was due to shorter hospital stays, fewer emergency room visits, and fewer readmissions (752)Steel JL, et al. (2024) Lancet, 403: 1351. DOI: 10.1016/S0140-6736(24)00015-1..
Researchers are also investigating how survivors of cancer experience posttraumatic growth, which describes positive life changes that can develop because of traumatic and stressful events, such as a diagnosis of cancer. Posttraumatic growth may lead to perceptions of new possibilities, closer relationships with family and friends, development of personal strength, spiritual development, and a greater appreciation for life (753)Fu X, et al. (2022) Front Public Health, 10: 927370. DOI: 10.3389/fpubh.2022.927370.. Although the concept of posttraumatic growth is not new, its potential in helping cancer survivors tackle the challenges of survivorship is only now being appreciated within the cancer care community. The most influential factors that affect posttraumatic growth include the level of social support and the use of various coping strategies among survivors of cancer (see Sidebar 44).
Delivering Care to Cancer Survivors
Coordinating Care
The multifaced approach to treating cancer necessitates providing survivors with appropriate care to address their many needs, including transitioning from active treatment, coordinating follow-up appointments, addressing financial needs, and gaining access to other survivorship resources. Even when these resources are available, understanding how or where to find them can be challenging. Coordination of care is required to help patients identify and gain access to such resources.
Coordinating cancer care is most effective when a designated individual or a team of people helps a cancer patient or survivor to gain access to the resources they need. A systematic review of studies conducted over 30 years found that coordination approaches led to improvements among 81 percent of survivors across multiple domains of cancer care, including screening, patient experience, and quality of end-of-life care (758)Gorin SS, et al. (2017) Ann Behav Med, 51: 532. DOI: 10.1007/s12160-017-9876-2..
Patient navigators and clinical care coordinators are individuals who help cancer patients and survivors access resources more effectively (see Sidebar 45). Patient advocates, who are often cancer survivors themselves, are uniquely positioned to bridge critical gaps between patients, survivors, and the health care system.
Leveraging Patient Reported Outcomes
Patient reported outcomes (PROs), which are reports given by patients on their status that have not been interpreted by a clinician, are becoming more common, especially in clinical trials, because they provide an unbiased, contextualized view of the patient experience (see Sidebar 46). Incorporating the patient’s perspective to understand treatment tolerability and efficacy in clinical trials will improve the cancer treatment experience for patients in the real world (765)Basch E, et al. (2023) J Clin Oncol, 41: 3724. DOI: 10.1200/jco.23.00903.. Patient reported outcomes are collected through questionnaires, which alert clinicians to the status of the patient regarding HRQOL, symptoms, and health-related behaviors (e.g., smoking, diet, physical activity) (766)Friends of Cancer Research. Broadening the Definition of Tolerability in Cancer Clinical Trials to Better Measure the Patient Experience. Accessed: July 31, 2023.. Patients engaged in monitoring their symptoms may have improved clinical outcomes and reduced risk of emergency room and hospital visits compared to those who do not complete these questionnaires (767)Natori A, et al. (2023) J Clin Oncol, 41: 285. DOI: 10.1200/Jco.22.01038.(768)Thanarajasingam G, et al. (2022) Lancet Haematol, 9: e374. DOI: 10.1016/S2352-3026(22)00045-X.. Integration of real-world electronic health records with PRO assessments that provide automated alerts to clinicians may help improve patient outcomes.
Use of patient reported outcomes in the Patient-Reported Outcomes Measurement Information System (PROMIS) study helped researchers identify issues surrounding psychosocial and quality of life matters among lung cancer survivors. The PROMIS study found that the most common issue faced by these individuals was reduced physical function and the interference of pain in their life. To improve patient-provider interactions and the quality of care that patients and survivors receive, the use of a screening program to identify patients with mental and physical issues as a result of their care is essential to alleviate these challenges (769)Hensley A, et al. (2023) J Dr Nurs Pract, 16: 22. DOI: 10.1891/JDNP-2022-0018..
Supporting Caregivers
Caregivers comprise family members or friends who help patients with long-term chronic illness and manage any and all aspects of their care. One in five US adults (ages 18 to 64), accounting for over 53 million people, provided care for another person in 2020, a significant increase from 43.5 million in 2015 (770)National Partnership for Women and Families. Paid Leave Could Keep More Than 6 Million Caregivers Connected to the Labor Force by 2030. Accessed: March 26, 2024.. It is further estimated that four million of these caregivers are caring for an adult cancer patient. More evidence of the challenges faced by caregivers is becoming clear and there are many opportunities to assist this vulnerable population.
In a study of cancer caregivers—specifically, informal caregivers—the average age of a caregiver was 58 years old. For many of these caregivers, helping a family member or friend with cancer takes a significant amount of time, with 40 percent of caregivers providing more than 40 hours of care per week, with most of that care devoted to activities, such as helping patients in and out of bed or chairs and help with using the restroom (771)Abazari A, et al. (2023) AMIA Annu Symp Proc, 2023: 243.. Compared to other age groups, caregivers who are 65 and over experienced the highest level of physical, emotional, and financial burden (771)Abazari A, et al. (2023) AMIA Annu Symp Proc, 2023: 243.. Compounding this issue is the lack of support for caregivers, with one study finding that only 16 percent of cancer clinics screened caregivers for distress and only 13 percent of those clinics had resources in place to assist caregivers (772)Nightingale CL, et al. (2024) J Natl Cancer Inst, 116: 324. DOI: 10.1093/jnci/djad198.. Survivors require many resources that are often provided by their caregivers, including arranging transportation, helping with day-to-day activities such as doctor visits, providing medical care or other clinical tasks, coordinating care, and giving emotional support. This often leads to burnout, which negatively impacts caregivers’ psychological and emotional well-being. Identifying caregiver burnout is critical for providing early interventions and support to these individuals.
Financial toxicity among caregivers of family with chronic conditions including cancer has been well documented (773)Bradley CJ, et al. (2022) J Natl Cancer Inst, 114: 1431. DOI: 10.1093/jnci/djac156.(774)Bradley CJ (2019) Semin Oncol Nurs, 35: 333. DOI: 10.1016/j.soncn.2019.06.003.(775)Bradley CJ, et al. (2023) J Clin Oncol, 41: 2939. DOI: 10.1200/Jco.22.02537.(776)Shi Y, et al. (2024) Support Care Cancer, 32: 146. DOI: 10.1007/s00520-024-08349-x.. A study of financial toxicity among patients with head and neck cancers and their caregivers found that while 26 percent of patients reported financial toxicity, 44.4 percent of caregivers reported financial toxicity (776)Shi Y, et al. (2024) Support Care Cancer, 32: 146. DOI: 10.1007/s00520-024-08349-x..
Legislative efforts including the Caregiver Advise, Record, and Enable (CARE) Act of 2016 requires hospitals to identify a caregiver for every patient and provide them with resources and training prior to releasing the loved one from the hospital. In 2022, the US Department of Health and Human Services released their National Strategy to Support Family Caregivers, which is a collaboration between federal and private partners to address the national need for comprehensive family caregiver support (777)Administration for Community Living. 2022 National Strategy to Support Family Caregivers. Accessed: June 21, 2024.. Efforts to increase support for family cancer caregivers are urgently needed because nearly a quarter of Commission on Cancer–accredited US cancer centers do not have a family caregiver program (778)Odom JN, et al. (2023) JAMA Netw Open, 6: e2337250. DOI: 10.1001/jamanetworkopen.2023.37250..
Next Section: Envisioning the Future of Cancer Science and Medicine Previous Section: Inspiring Science. Fueling Progress. Revolutionizing Care.