- Research: Driving Progress against Cancer
- Cancer: An Ongoing Public Health Challenge
- Variable Progress among Types of Cancer and Stages of Diagnosis
- Disparities in Progress for Certain Population Groups
- The Growing Population Burden of Cancer
- The Challenges Associated with Survivorship
- Cancer: A Costly Disease Research: A Vital Investment
Cancer in 2019
- In the United States, the overall cancer death rate is decreasing, and the number of cancer survivors is increasing.
- In the past 3 years, the number of cancer survivors living in the United States increased by 1.4 million, reaching more than 16.9 million on January 1, 2019.
- Since the 1990s, the age-adjusted overall cancer death rate has decreased more rapidly among African Americans than among whites; however, the African American population still disproportionately shoulders the burden of overall cancer mortality.
- The economic burden of cancer is enormous, both in the United States and globally.
Research: Driving Progress against Cancer
Research is the backbone of progress against cancer because it is the driving force behind every clinical advance that improves survival and quality of life, and every new policy designed to advance public health.
Every clinical advance and every policy that spurs progress against cancer is the culmination of a complex process that requires collaboration over the course of many years among numerous different stakeholders committed to fundamentally changing the face of this devastating disease (see sidebar on Driving Progress against Cancer Together).
The remarkable progress being made against cancer – in particular, advances in reducing smoking rates, and in early detection, interception, and treatment of the disease – is causing cancer death rates to fall and the number of children and adults who survive a cancer diagnosis to rise (2). In fact, the age-adjusted overall U.S. cancer death rate declined by 27 percent from 1991 to 2016, a reduction that translates into more than 2.6 million cancer deaths avoided (2). In addition, in the past 3 years, the number of adults and children living in the United States with a history of cancer rose by an estimated 1.4 million, reaching more than 16.9 million on January 1, 2019 (3) (4).
Among the advances in cancer treatment that occurred during the 12 months covered by this report, August 1, 2018 to July 31, 2019, are the 17 new anticancer therapeutics approved by the U.S. Food and Drug Administration (FDA) for introduction into the clinic (see Progress across the Clinical Cancer Care Continuum). In addition, during this period, the uses of 10 previously approved anticancer therapeutics were expanded to include additional types of cancer.
Cancer: An Ongoing Public Health Challenge

Although we have made incredible progress against cancer, it continues to be an enormous public health challenge in the United States and around the world (see sidebar on Cancer: A Global Public Health Challenge) (2)(5). In the United States alone, it is predicted that 1,762,450 new cases of cancer will be diagnosed in 2019 and that 606,880 people will die from the disease (2) (see Table 1).
Variable Progress among Types of Cancer and Stages of Diagnosis
Among the challenges we face is that progress against cancer has not been uniform for all types of cancer (8) or for all stages of a given type of cancer (8).
These challenges are illustrated by the fact that the 5-year relative survival rates for U.S. patients vary widely depending on both the type of cancer diagnosed and the stage at diagnosis (8). For example, the overall 5-year relative survival rates of 90 percent for women with breast cancer and 98 percent for men with prostate cancer stand in stark contrast to the overall 5-year relative survival rates of 18 percent for people with liver cancer and 19 percent for those with lung cancer. In addition, among women with breast cancer and people with colorectal cancer, those whose cancer is confined to the breast, or to the colon or rectum, have 5-year relative survival rates of 99 percent and 90 percent, respectively, while those whose cancer has metastasized have 5-year relative survival rates of 27 percent and 14 percent, respectively.
Developing new and effective tests for early detection of more types of cancer could help address the challenge of variable progress between types of cancer because patients diagnosed when cancer is at an early stage, before it has spread to other parts of the body, have a much higher likelihood of long-term survival than those diagnosed when the disease has spread to distant sites, an occurrence known as metastasis.
Disparities in Progress for Certain Population Groups
Cancer health disparities are another pressing challenge.
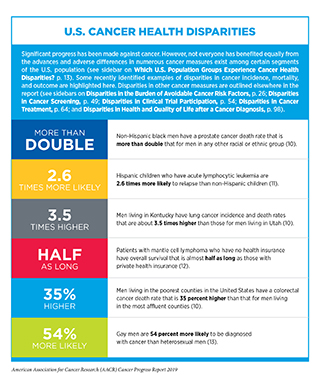
The National Cancer Institute (NCI) defines cancer health disparities as adverse differences in cancer measures such as number of new cases, number of deaths, cancer-related health complications, survivorship and quality of life after cancer treatment, screening rates, and stage at diagnosis that exist among certain population groups (9) (see sidebars on Which U.S. Population Groups Experience Cancer Health Disparities? and U.S. Cancer Health Disparities).
The African American population is one group that has long experienced cancer health disparities (14). For example, in 1990, the overall cancer death rates for African American men and women were 47 percent and 19 percent higher than they were for white men and women, respectively. In recent years, these disparities have narrowed to 19 percent and 13 percent higher for African American men and women, respectively, because overall cancer death rates have decreased more rapidly among African American men and women than they have among white men and women. However, the African American population still disproportionately shoulders the burden of overall cancer mortality compared with other racial/ethnic groups (10).
A significant proportion of the U.S. population is affected by cancer health disparities. Thus, it is important that we intensify research efforts designed to improve our understanding of the relative contributions of different factors that cause U.S. cancer health disparities (see sidebar on Why Do U.S. Cancer Health Disparities Exist?). Only with new insights obtained through research, including basic research using samples from all U.S. population groups, and through the participation of individuals from all these groups in clinical trials will we develop and implement interventions that will eliminate cancer for all.
The Growing Population Burden of Cancer

Unless we develop and effectively implement more effective strategies for cancer prevention, early detection, and treatment, the public health challenge posed by cancer will grow considerably in the United States and around the world in the coming decades (see sidebar on Cancer: A Global Public Health Challenge) (2)(5).
In the United States, it is predicted that the number of new cancer cases and the number of cancer deaths will rise year after year, reaching more than 2.3 million and almost 1 million, respectively, in 2040 (16). These sharp increases over the current numbers are anticipated largely because of overall population growth and because the segment of the U.S. population that accounts for the majority of cancer diagnoses – those age 65 and older (8) – is expected to grow from 49 million in 2016 to 81 million in 2040 (2)(17). Also contributing to the projected increase in the number of U.S. cancer cases are the high rates of obesity among adults and children – which are nearly 40 percent and 20 percent, respectively – and the continued use of cigarettes by 14 percent of adults (18)(19).
Providing optimal care to the rapidly growing number of patients with cancer will require a substantially larger health care workforce than there is currently. For example, one recent study estimated that the number of patients worldwide requiring initial treatment with chemotherapy each year will increase from 9.8 million in 2018 to 15 million in 2040 and that the number of physicians required to optimally deliver this chemotherapy will rise from 65,000 to 100,000 (20).
The Challenges Associated with Survivorship
The rapidly expanding population of cancer survivors, which encompasses all living people who have ever been diagnosed with cancer, is a testament to the significant progress we are making against the disease. However, this situation poses new challenges for all stakeholders committed to reducing the morbidity and mortality of cancer in the United States and around the world.
One challenge posed by the growing population of cancer survivors is that most of these people have poorer health and quality of life than other individuals of a similar age (21). For example, one study found that individuals who have been successfully treated for childhood cancer have experienced an average of 17 chronic health conditions by age 50, five of which were serious or disabling, life threatening, or fatal (22). In comparison, individuals in the general population have experienced an average of nine chronic health conditions by the same age, only two of which are serious or disabling, life threatening, or fatal.
As more and more people survive longer after a cancer diagnosis in the coming decades, the totality of their health care needs will grow significantly. Adding to the growing burden on the health care system is the fact that the proportion of cancer survivors who are age 65 or older is expected to increase from 64 percent in 2019 to 73 percent in 2040 and individuals in this age group tend to have more chronic health conditions than younger individuals (23).
Much work is needed to make sure that the health care system can withstand the impact of caring for the burgeoning population of cancer survivors (24). We also need to identify ways to improve quality of care and optimize quality of life for cancer survivors, as discussed in Supporting Cancer Patients and Survivors.
Cancer: A Costly Disease
Research: A Vital Investment
The immense global toll of cancer is felt through both the number of lives it affects each year and its economic impact. One study estimated that the direct costs related to the prevention and treatment of cancer and the economic value of lives lost and disability caused, cost the world about $1.16 trillion in 2010 (25).
In the United States, the direct medical costs of cancer care are estimated to have been $80.2 billion in 2015, the last year for which these data are currently available (2). This number does not include the indirect costs of lost productivity due to cancer-related morbidity and mortality, which are also extremely high. In fact, one recent study estimated that cancer deaths among Americans ages 16 – 84 resulted in $94.4 billion in lost earnings in 2015 (26).
The cost of cancer care stands in stark contrast to the amount of money the federal government invests in medical research, most of which is administered through the 27 institutes and centers of the National Institutes of Health (NIH). The largest of these institutes and centers is the NCI, which is the federal government’s principal agency for cancer research and training. In 2015, the same year that the direct medical costs of cancer care were $80.2 billion, the budget for the NIH was just $30.36 billion, of which $4.93 billion went to the NCI.
With the number of cancer cases projected to increase in the coming decades, we can be certain that both the direct and indirect costs will also escalate.
The rising personal and economic burden of cancer underscores the urgent need for more research so that we can accelerate the pace of progress against cancer. Recent advances, some of which are highlighted in this report, were made as a direct result of the cumulative efforts of researchers from across the spectrum of research disciplines. Much of their work, as well as the federal regulatory agency that assures the safety and efficacy of medical devices and therapeutic advances – the FDA’is supported by funds from the federal government. The consecutive multibillion dollar increases for the NIH budget in fiscal year (FY) 2016, FY 2017, FY 2018, and FY 2019 have helped (see Sustaining the Momentum with Annual Funding Increases for Medical Research). To keep up with the pace of scientific innovation, it is imperative, however, that Congress continue to provide sustained, robust, and predictable increases in investments in the federal agencies that are vital for fueling progress against cancer, in particular, the NIH, NCI, FDA, and Centers for Disease Control and Prevention (CDC), in the years ahead (see The AACR Call to Action).