- Research: Driving Progress Against Cancer
- Cancer: An Ongoing Public Health Challenge in the United States and Worldwide
- Variable Progress Among Stages at Diagnosis and Types of Cancer
- Disparities in Progress for Certain Population Groups
- The Growing Burden of Cancer
- The Global Challenge of Cancer
- Funding Cancer Research: A Vital Investment
Cancer in 2022
In this section, you will learn:
- In the United States, the age-adjusted overall cancer death rate has been steadily declining since the 1990s, with the reductions between 1991 and 2019 translating into nearly 3.5 million cancer deaths avoided.
- In the past three years, the number of cancer survivors living in the United States increased by more than a million, reaching greater than 18 million as of January 1, 2022.
- Certain U.S. populations have not benefited equally from the advances against cancer.
- The personal burden of cancer and its economic toll both on individuals and the U.S. health care system are expected to rise in the coming decades, highlighting the urgent need for more research to accelerate the pace of progress against cancer.
Research: Driving Progress Against Cancer
Medical research is the foundation of progress against the collection of many diseases we call cancer. Research improves survival and quality of life for people around the world because it is the driving force behind every advance in cancer science and medicine and every legislative action designed to improve public health. Each breakthrough against cancer is the culmination of a complex, multifaceted process that takes long-term commitment and years of effort by individuals from all segments of the medical research community (see sidebar on The Medical Research Community: Driving Progress Together).
The remarkable progress being made against cancers—in particular, improvements in reducing smoking rates and developments in early detection and treatment—is resulting in cancer death rates falling steadily and in a rising number of people who survive a cancer diagnosis. In fact, the age-adjusted overall cancer death rate has declined by 32 percent between 1991 and 2019 in the United States, a reduction that translates into nearly 3.5 million cancer deaths avoided (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE]. Among children and adolescents with cancer, overall death rates have declined by more than half between 1970 and 2019, largely due to advances in treatment (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE]. In addition, in the past three years, the number of adults and children living in the United States with a history of cancer rose by more than a million, exceeding an estimated 18 million on January 1, 2022 (2)Miller KD, et al. Cancer Treatment and Survivorship Statistics, 2022. CA Cancer J Clin 2022;0:1-28. [LINK NOT AVAILABLE].
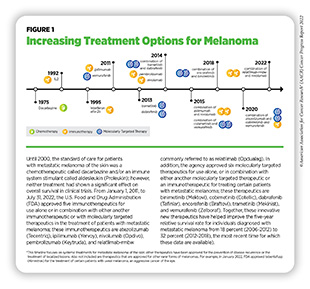
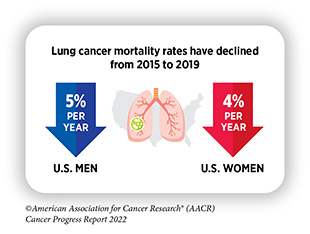
The steady decline in the overall cancer death rate can be attributed mainly to the unprecedented progress against lung, colorectal, breast, and prostate cancer, the four most common cancer types in the United States. In fact, during the past three decades, age-adjusted death rates from lung, female breast, and colorectal cancers have decreased by 44, 42, and 53 percent, respectively (3)Kratzer TB, et al. Progress against cancer mortality 50 years after passage of the National Cancer Act. JAMA Oncol 2022;8:156-9. [LINK NOT AVAILABLE]. Furthermore, there have been significant developments against previously intractable cancers, such as melanoma, the deadliest form of skin cancer, fueled by a range of innovative new therapeutics that have moved rapidly from the bench to the clinic and received approval by the U.S. Food and Drug Administration (FDA) (see Figure 1). Collectively, these advances have led to the increase in five-year relative survival rate for all cancers combined from 49 percent in the mid-1970s to nearly 70 percent from 2011 to 2017, which are the most recent data available (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE].
Among the major advances made across the clinical cancer care continuum from August 1, 2021, to July 31, 2022, are the eight new anticancer therapeutics approved for use by FDA (see Table 4). During this period, FDA also approved two new imaging agents to help visualize cancerous cells, several artificial intelligence-based tools to improve detection and diagnosis of cancers, and new uses for 10 previously approved anticancer therapeutics.
The research that drives progress against cancer is made possible by investments from governments, philanthropic individuals and organizations, and the private sector. In the United States, government investments in medical research are administered mostly through the 27 institutes and centers of the National Institutes of Health (NIH). The largest component of NIH is the National Cancer Institute (NCI), which is the federal government’s principal agency for cancer research and training. Medical research funded by the public sector contributes significantly to novel drug development, which is critical to saving and improving lives (6)Nayak RK, et al. Public-sector contributions to novel biologic drugs. JAMA Intern Med 2021;181:1522-5. [LINK NOT AVAILABLE] (7)Galkina Cleary E, et al. Contribution of NIH funding to new drug approvals 2010-2016. Proc Natl Acad Sci U S A 2018;115:2329-34. [LINK NOT AVAILABLE]. Federal investments in government agencies conducting research, such as FDA and the Centers for Disease Control and Prevention (CDC), are also of particular importance.
Cancer: An Ongoing Public Health Challenge in the United States and Worldwide
Although we have made incredible progress against cancers, this group of devastating diseases continues to be an enormous public health challenge in the United States and around the world. In the United States alone, it is predicted that 1,918,030 new cases of cancer will be diagnosed in 2022 and that 609,360 people will die from the disease (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE] (see Table 1). These estimates do not account for the consequences of COVID-19, which has proven to have an adverse impact across the spectrum of cancer research and patient care including significant declines in cancer screening and diagnosis (8)American Association for Cancer Research. AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care. Accessed: June 30, 2022.[cited 2020 Jul 15].. In addition, data from the past two years have clearly shown the heightened risks of SARS-CoV-2 infection and severe COVID-19 among patients with cancer, albeit COVID-19-related mortality among this population has decreased over time (8)American Association for Cancer Research. AACR Report on the Impact of COVID-19 on Cancer Research and Patient Care. Accessed: June 30, 2022.[cited 2020 Jul 15].(9)Dieci MV, et al. Clinical profile and mortality of Sars-Cov-2 infection in cancer patients across two pandemic time periods (Feb 2020-Sep 2020; Sep 2020-May 2021) in the Veneto Oncology Network: The ROVID study. Eur J Cancer 2022;167:81-91. [LINK NOT AVAILABLE]. Ongoing research will uncover the long-term effects of COVID-19 on cancer outcomes (10)National Cancer Institute. NCI COVID-19 in Cancer Patients Study (NCCAPS). Accessed: Nov 27, 2021.[cited 2020 Jul 15]..
Variable Progress Among Stages at Diagnosis and Types of Cancer
Progress against cancers has not been uniform for all stages of a given type of disease (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. This issue is illustrated by the fact that the five-year relative survival rates for U.S. patients vary widely depending on the stage at diagnosis (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. As one example, among women with breast cancer and people with colorectal cancer, those whose cancer is confined to the breast, or to the colon or rectum, have five-year relative survival rates of 99 percent and 92 percent, respectively, while those whose cancer has spread to a distant site have five-year relative survival rates of 30 percent and 16 percent, respectively (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15]..
An additional challenge that we face is the uneven progress against various cancer types (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. For example, the overall five-year relative survival rates of nearly 91 percent for women with breast cancer and 97 percent for men with prostate cancer stand in stark contrast to the overall five-year relative survival rates of 21 percent for people with liver cancer and less than 12 percent for those with pancreatic cancer (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. While some of these differences could be attributed to early detection of breast and prostate cancers through population level screening (see sidebar on Ways to Screen for Cancer), disparities in five-year relative survival rates hold true for patients with these four cancer types even when their diseases are diagnosed at an advanced stage. The five-year relative survival rates of greater than 30 percent for advanced-stage female breast and male prostate cancers are significantly higher than the five-year relative survival rates of less than five percent for those with advanced-stage liver or pancreatic cancer (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15]..
Among children ages one to 14 years, cancer is the second-leading cause of death, and the most diagnosed cancers are leukemia and brain tumors (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE]. Thanks to extraordinary advances in treatments for childhood leukemia, the age-adjusted mortality rate from the disease has almost halved in the past two decades. Unfortunately, mortality rates from childhood brain and other central nervous system tumors have essentially remained unchanged (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15]..
Developing new and effective tests for early detection of more types of cancer as well as better treatment options for all cancer types and for all stages of diagnosis could help address the challenges of variable progress against different types of cancer.
Disparities in Progress for Certain Population Groups
Cancer health disparities are one of the most pressing public health challenges in the United States. NCI defines cancer health disparities as adverse differences in cancer such as number of new cases, number of deaths, cancer-related health complications, survivorship and quality of life after cancer treatment, screening rates, and stage at diagnosis that exist among certain population groups (12)Cancer health disparities definitions and examples. Accessed: April 22, 2022.[cited 2020 Jul 15]. (see sidebar on Which U.S. Population Groups Experience Cancer Health Disparities?).
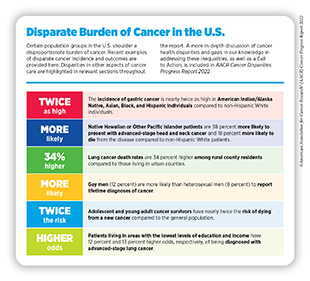
As outlined in the AACR Cancer Disparities Progress Report 2022, racial and ethnic minorities and other medically underserved U.S. populations shoulder a disproportionately higher burden of cancer (see sidebar on Disparate Burden of Cancer in the U.S.) (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2022.[cited 2020 Jul 15].. As one example, the U.S. Black population has long experienced cancer health disparities.
In 1990, the overall cancer death rates for Black people were 33 percent higher than for White people (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. There has been some progress in recent years as evidenced by the narrowing of the gap in cancer death rates between the Black and White populations to 13 percent in 2019, a 60 percent decline in the disparities since 1990 (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].(14)Lawrence WR, et al. Trends in cancer mortality among black individuals in the US from 1999 to 2019. JAMA Oncol 2022. [LINK NOT AVAILABLE]. However, even in 2019, overall cancer death rates were higher among Black men and women compared to all other U.S. racial and ethnic groups (14)Lawrence WR, et al. Trends in cancer mortality among black individuals in the US from 1999 to 2019. JAMA Oncol 2022. [LINK NOT AVAILABLE].
Sexual and gender minorities (SGM) are another U.S. population that experiences cancer health disparities. According to a new report, gay men are more likely than heterosexual men to report lifetime diagnoses of cancers, and gay men and lesbian women are more frequently unable to afford many types of health care services compared to heterosexual men and women (15)Heslin KC, et al. Sexual orientation differences in access to care and health status, behaviors, and beliefs: Findings from the National Health and Nutrition Examination Survey, National Survey of Family Growth, and National Health Interview Survey. Natl Health Stat Report 2022:1-16. [LINK NOT AVAILABLE]. Unfortunately, there are limited data on the epidemiology of cancer incidence and outcomes among SGM individuals making it difficult to evaluate the true burden of cancer in this underserved population. It is imperative that researchers collect disaggregated data by sexual orientation and gender identity, as well as within sexual minority groups (e.g., gay versus bisexual) and gender minority groups (e.g., transgender versus nonbinary) to accurately capture cancer epidemiology in these heterogeneous populations (13)American Association for Cancer Research. AACR Cancer Disparities Progress Report 2022. Accessed: June 30, 2022.[cited 2020 Jul 15]..
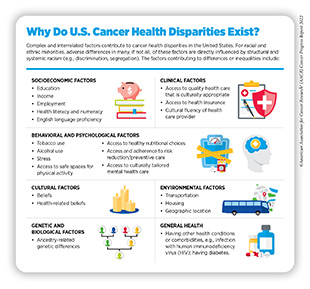
Research has identified complex and interrelated factors, often referred to as the social determinants of health, including socioeconomic, cultural, behavioral, environmental, and clinical factors that contribute to cancer health disparities.
It is increasingly evident that structural racism and systemic injustices cause adverse differences in social determinants of health, creating conditions that perpetuate health inequities, including cancer health disparities (see sidebar on Why Do U.S. Cancer Health Disparities Exist?).
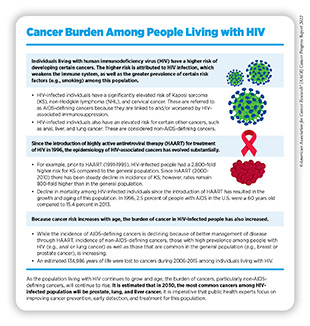
One of the drivers of cancer health disparities is general health of a population group. For instance, individuals with underlying health conditions, such as diabetes, or those infected with certain pathogens, such as human immunodeficiency virus (HIV), experience a greater burden of cancer (see sidebar on Cancer Burden Among People Living with HIV). It should be noted that individuals with intersectional identities often experience multilevel barriers to optimal health care that adversely impact cancer incidence and outcomes. As one example, among individuals living with HIV, those who are from racial and ethnical minority populations may experience worse cancer health disparities (20)Elizabeth Read-Connole, et al. Basic/Translational research on Health Disparities in HIV/AIDS and cancer (Clinical trial optional). 2022. [LINK NOT AVAILABLE]. Understanding the biological drivers of cancer health disparities in marginalized populations with an underlying HIV/AIDS diagnosis is an area of active investigation (20)Elizabeth Read-Connole, et al. Basic/Translational research on Health Disparities in HIV/AIDS and cancer (Clinical trial optional). 2022. [LINK NOT AVAILABLE].
Considering that a significant proportion of the U.S. population is affected by cancer health disparities, it is important that public health experts intensify research efforts designed to improve our understanding and mitigating of these disparities. Only with new insights obtained through innovative research, including basic science using biospecimens from diverse populations, clinical trials involving participants from all sociodemographic backgrounds, and health care delivery research, will we develop and implement interventions that may eventually eliminate cancers for all populations.
The Growing Burden of Cancer
The public health challenge posed by cancer is predicted to grow considerably in the coming decades unless we develop and implement more effective strategies for cancer prevention, early detection, and treatment (26)International Agency for Research on Cancer. Global Cancer Observatory. Accessed: July 15, 2022.[cited 2020 Jul 15].. In the United States alone, the number of new cancer cases diagnosed each year is expected to reach nearly 2.3 million by 2040 (26)International Agency for Research on Cancer. Global Cancer Observatory. Accessed: July 15, 2022.[cited 2020 Jul 15].. This is largely because cancer is primarily a disease of aging; 80 percent of U.S. cancer diagnoses occur among those who are 55 or older; 57 percent of diagnoses occur among those 65 and older (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE], and this segment of the U.S. population is expected to grow from 54.1 million in 2019 to nearly 81 million in 2040 (27)U.S. Department of Health and Human Services. Administration for Community Living. 2020 Profile of Older Americans. Accessed: Jul 6, 2022.[cited 2020 Jul 15].. Also contributing to the projected increase in the number of U.S. cancer cases are high rates of obesity and physical inactivity, which are both linked to some common types of cancer, and the continued use of tobacco products among certain U.S. populations.
Progress has been made toward reducing cancer incidence in the United States; new cancer cases have declined 10 percent from their peak in 1992 to 2019, the year for which the most recent data are reported (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. However, overall cancer incidence has been rising among the U.S. adolescent and young adult (AYA) population (ages 15 to 39), which has seen nearly a 20 percent increase in cancer incidence from 2000 to 2019 (5)National Cancer Institute. Surveillance, Epidemiology, and End Results program explorer. Accessed: June 30, 2022.[cited 2020 Jul 15].. In addition, the incidence of certain cancer types is steadily increasing, specifically among people younger than 50. As one example, many recent studies have reported an increase in the incidence of early-onset colorectal cancer among those age 49 and younger (28)Sinicrope FA. Increasing incidence of early-onset colorectal cancer. N Engl J Med 2022;386:1547-58. [LINK NOT AVAILABLE] (29)Calip GS, et al. Colorectal cancer incidence among adults younger than 50 years-understanding findings from observational studies of lower gastrointestinal endoscopy. JAMA Oncol 2022;8:981-3. [LINK NOT AVAILABLE]. The reasons behind rising cases of early-onset colorectal cancers are not completely understood but is presumed to be multifactorial, including contributions of modifiable lifestyle factors such as unhealthy diet and physical inactivity as well as factors that alter the gut microbiome such as use of antibiotics. To reduce the burden of early-onset colorectal cancer, many professional societies have modified their screening guidelines to recommend starting colorectal cancer screening at an earlier age. Additionally, researchers are evaluating new and improved strategies including genetic testing and others for prevention and early detection of colorectal cancer in the younger population (28)Sinicrope FA. Increasing incidence of early-onset colorectal cancer. N Engl J Med 2022;386:1547-58. [LINK NOT AVAILABLE].
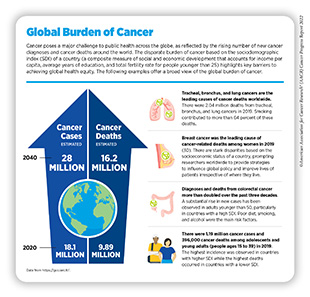
The Global Challenge of Cancer
Beyond the United States, cancer is an ongoing global challenge (see sidebar on Global Burden of Cancer). According to a new analysis, there were an estimated 17.2 million new cancer cases (excluding nonmelanoma skin cancer) and 10 million cancer deaths globally, in 2019 (30)Kocarnik JM, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol 2022;8:420-44. [LINK NOT AVAILABLE]. The study evaluated cancer burden from 204 countries and territories as indicated by cancer-related deaths, as well as disability-adjusted life years (DALYs) and years of life lost (YLLs), which are two measures of cancer morbidity. Researchers found that among the 22 groups of diseases and injuries analyzed, cancer was second only to cardiovascular disease in the number of deaths, DALYs, and YLLs (30)Kocarnik JM, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol 2022;8:420-44. [LINK NOT AVAILABLE]. The five leading causes of cancer-related morbidity among men and women combined were lung cancer, colorectal cancer, stomach cancer, breast cancer, and liver cancer.
The study also indicated that, although there were increases in the absolute numbers of both global cancer deaths and new cases from 2010 to 2019, the age-standardized mortality and incidence rates decreased by six percent and one percent, respectively (30)Kocarnik JM, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol 2022;8:420-44. [LINK NOT AVAILABLE]. These trends, however, precede the setbacks in cancer care and outcomes that have been caused by the COVID-19 pandemic. Global health experts are also concerned about the consequences of the ongoing wars that have displaced populations, further destroying health care systems, disrupting social services, and increasing risk of infectious disease transmission (31)The ASCO Post Staff. War is hell. It’s also a public health disaster, especially for people with cancer. Accessed: July 6, 2022.[cited 2020 Jul 15].. Considering the devastating impact of these global crises on the entire continuum of cancer research and patient care as well as the growth of the global population age 65 and older (32)United Nations. Ageing. Accessed: July 6, 2022.[cited 2020 Jul 15]., researchers caution that the burden of cancer worldwide may rise significantly in the coming decades.
Another concern among global public health experts is that, while age-standardized mortality and incidence rates are declining overall, the reduction in rates appears to be driven by countries with a higher sociodemographic index (SDI)—a composite measure of the social and economic development of a country that considers income per capita, average years of education, and total fertility rate for people younger than 25. The data indicate that age-standardized cancer incidence and mortality rates are increasing in countries with lower SDI (33)Pramesh CS, et al. Priorities for cancer research in low- and middle-income countries: a global perspective. Nat Med 2022;28:649-57. [LINK NOT AVAILABLE].
To ensure that progress against cancer is equitable worldwide, it is imperative that the global medical research community work together and share best practices to implement newer and more effective strategies that incorporate local needs and knowledge into tailored national cancer control plans. Public health experts have identified several priorities based on present and future needs of low resource countries, including reducing the burden of advanced cancers; improving access, affordability, and outcomes of treatment, utilizing value-based care; fostering implementation research; and leveraging technology to improve cancer control (33)Pramesh CS, et al. Priorities for cancer research in low- and middle-income countries: a global perspective. Nat Med 2022;28:649-57. [LINK NOT AVAILABLE].
Funding Cancer Research: A Vital Investment
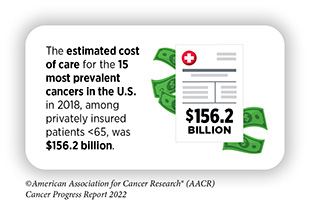
Cancer exerts an immense toll because of the number of lives it affects each year and through its significant economic impact. The direct medical costs of cancer care are one measure of the financial impact of cancer, and in the United States alone, they were estimated to be $183 billion in 2015, the last year for which these data are currently available; this cost is projected to increase to $246 billion by 2030 (1)Siegel RL, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [LINK NOT AVAILABLE]. These numbers do not include the indirect costs of lost productivity due to cancer-related morbidity and mortality, which are also extremely high. Notably, cancer patients in the United States shouldered an economic burden of $21 billion in 2019 from out-of-pocket costs and other related expenses, which is nearly 3.5 times the amount of approximately $6 billion in NCI funding for cancer research in the same year (38)Yabroff KR, et al. Annual Report to the Nation on the Status of Cancer, part 2: Patient economic burden associated with cancer care. J Natl Cancer Inst 2021;113:1670-82. [LINK NOT AVAILABLE].
With the number of cancer cases projected to increase in the coming decades, we can be certain that both the direct and indirect costs will also escalate. The rising personal and economic burden of cancer underscores the urgent need for more research so that we can accelerate the pace of progress against cancer.
Recent advances in cancer prevention, detection, and treatment, many of which are highlighted in this report, were made as a direct result of the cumulative efforts of researchers from across the spectrum of cancer science and medicine. Much of their work, as well as that of FDA—the federal regulatory agency that assures the safety and efficacy of medical devices and therapeutic advances—is supported by funds from the federal government. The consecutive increases for the NIH budget in the last seven fiscal years have helped maintain the momentum of progress (see Investments in Research Fuel a Healthier Future). To keep up with the pace of scientific and technological innovation, it is imperative, however, that Congress continue to provide sustained, robust, and predictable increases in investments in the federal agencies that are vital for fueling progress against cancer, in particular, NIH, NCI, FDA, and CDC, in the years ahead (see AACR Call to Action).
Next Section: A Snapshot of a Year of Progress