- Addressing the Challenges Faced by Survivors
- Addressing the Unique Challenges Faced by Vulnerable Populations
- Challenges Faced by Children
- Challenges Faced by Adolescents and Young Adults
- Challenges Faced by Older Adults
- Improving Quality of Life and Health Outcomes
- Participating in Physical Activity
- Eating a Healthy Diet and Maintaining a Healthy Weight
- Eliminating Alcohol and Tobacco Use
- Integrating Palliative Care
- Improving Mental Health
- Delivering Care to Cancer Survivors
- Supporting Caregivers
Supporting Cancer Patients and Survivors
In this section, you will learn:
- As of January 1, 2025, there were an estimated 18.6 million people living with a history of a cancer diagnosis in the United States.
- Cancer patients and survivors face a multitude of physical, emotional, and financial challenges because of their cancer and treatment.
- Eating a healthy diet, reducing alcohol consumption and tobacco use, and exercising can improve the survivorship experience and cancer outcomes.
- Caregivers of patients with cancer can face the same negative health and social consequences as the family members and loved ones they care for.
According to the National Cancer Institute (NCI), a person is considered a cancer survivor from the time of cancer diagnosis through the balance of the person’s life. Each person diagnosed with cancer has a unique experience ranging from successful treatment and living cancer-free for the remainder of life to experiencing varying degrees of side effects to a subsequent cancer diagnosis with the same or a different type of cancer.
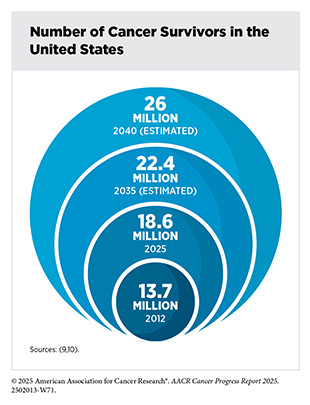
Unprecedented advances in cancer treatments over the past decade have led to more patients living longer and fuller lives after a cancer diagnosis. As of January 1, 2025, more than 18.6 million adults and children with a history of cancer were living in the United States (US), representing 5.5 percent of the population (9)Wagle NS, et al. (2025) CA Cancer J Clin.. This reflects a substantial increase since the release of the first AACR Cancer Progress Report in 2011, when there were an estimated 12 million cancer survivors in the United States. Importantly, most cancer survivors today are living many years beyond their initial diagnosis. In 2025, nearly 50 percent of cancer survivors in the United States had lived 10 or more years since their diagnosis and 22 percent had lived 20 or more years (9)Wagle NS, et al. (2025) CA Cancer J Clin.. Looking ahead, the number of survivors is projected to exceed 22 million by 2035 and reach 26 million by 2040 (9)Wagle NS, et al. (2025) CA Cancer J Clin.(10)Tonorezos E, et al. (2024) J Natl Cancer Inst, 116: 1784..
As more people are living longer and fuller lives after a cancer diagnosis, greater understanding of survivorship experiences is needed. These experiences include the physical, psychosocial, and economic adversities caused by a cancer diagnosis. Cancer survivors are also at risk for late effects or secondary health problems due to their cancer treatments and therefore require long-term follow-up care.
A diagnosis of cancer also impacts friends, family members, and other caregivers, who are often the main support network for the survivor. As a result, survivorship research, support, and care must extend beyond the cancer patient and survivor to include individuals who make up the support structure. The following sections highlight the challenges faced by cancer survivors and their support network, strategies to improve survival and quality of life, and approaches that have been shown to deliver care most effectively.
Addressing the Challenges Faced by Survivors
Depending on the type and stage of cancer, as well as the age at which an individual is diagnosed, cancer survivorship can encompass a wide range of unique experiences of living with, through, and beyond cancer (see Sidebar 48). Physical, psychosocial, and financial stresses can deprive individuals diagnosed with cancer of meaningful life experiences regardless of which phase of survivorship they are experiencing. These challenges can also disrupt the lives of family members, friends, and other caregivers. It is important to note that the challenges discussed here are interrelated and may collectively contribute to the burden of cancer faced by cancer patients and survivors. For example, limited physical mobility because of cancer treatment and/ or difficulties paying for medical bills can lead to distress and/or depression.
Physical Challenges
Survivors can experience a wide range of short- and long-term symptoms caused by cancer and/or its treatments. Short-term effects include hair loss, pain, nausea, vomiting, and loss of smell and appetite with varying severity of symptoms depending on the person, cancer type, and treatment regimen. As cancer survivors are living longer, the development of long-term side effects such as heart damage (cardiotoxicity), lung damage, loss of bone density, and cognitive decline is becoming more common and demands a greater understanding to reduce or manage these conditions (see Sidebar 48).
Adult survivors in the United States experience higher rates of physical disability compared to those without a history of cancer. According to a recent study, cancer survivors were 21 percent more likely to report a mobility disability (i.e., difficulty walking or climbing stairs) and 19 percent more likely to report a self-care disability (i.e., difficulty dressing or bathing), compared to those without a history of cancer (870)Cao C, et al. (2024) J Clin Oncol, 42: 2257.. These functional limitations were more common among survivors who were undergoing active treatment, those who belonged to racial and ethnic minorities, and those with comorbidities or lower socioeconomic status.
A major concern for cancer survivors is the risk of recurrence or the development of a new, biologically distinct, second cancer. The likelihood of recurrence or a second cancer diagnosis is influenced by a variety of factors, including the type and stage of the initial cancer, treatments received, genetic predisposition, lifestyle behaviors (e.g., smoking), obesity, and socioeconomic status (871)Zeng M, et al. (2025) J Transl Med, 23: 115.. Compared with the general population, cancer survivors face an estimated 16 percent increased risk of developing a second primary cancer (872)Wang Y, et al. (2025) J Transl Med, 23: 355.(873)Warkentin MT, et al. (2025) Cancer Epidemiol Biomarkers Prev, 34: 174.. This risk is particularly elevated among individuals with a history of childhood cancer, as well as adult survivors of Hodgkin lymphoma, and cancers linked to obesity and tobacco use (see Reducing the Risk of Cancer Development) (874)American Cancer Society. Cancer Treatment and Survivorship Facts and Figures 2022-2024. Accessed: June 10, 2025.(875)Bodelon C, et al. (2024) JAMA Netw Open, 7: e2433132.(876)Sung H, et al. (2022) J Natl Cancer Inst, 114: 1095..
Chemotherapy-induced peripheral neuropathy (CIPN) is a common and often debilitating adverse effect of cancer treatment that affects up to 85 percent of patients receiving chemotherapy. Symptoms of CIPN include numbness, tingling, burning, or electric shock–like sensations in the hands and feet, leading to functional impairment and reduced quality of life (877)McNeish BL, et al. (2024) J Geriatr Oncol, 15: 101765.(878)Tao Z, et al. (2024) Cancer Lett, 611: 217433.. While some symptoms resolve over time, nearly one-third of survivors experience persistent, painful neuropathy lasting 6 months or longer after treatment completion (879)Lemanska A, et al. (2023) ESMO Open, 8: 102063.. A recent analysis of global data found that more than 40 percent of individuals with CIPN suffer from chronic pain (880)D’Souza RS, et al. (2025) Reg Anesth Pain Med..
Currently, treatment options for CIPN remain limited, as there are no FDA-approved medications specifically for its treatment or prevention. Duloxetine is recommended by some cancer-focused organizations for treating CIPN, but its effects are modest (881)Jordan B, et al. (2020) Ann Oncol, 31: 1306.(882)Loprinzi CL, et al. (2020) J Clin Oncol, 38: 3325.. However, a recent study showed that hand cooling using frozen gloves or hand compression using snug-fitting surgical gloves can reduce the risk of high-grade CIPN in breast cancer patients receiving taxane-based chemotherapy. While hand cooling and compression show promise for mitigating CIPN, more research is needed to validate these findings and determine their effectiveness across broader patient populations (883)Michel LL, et al. (2025) JAMA Oncol, 11: 408..
Cachexia is a serious condition characterized by unintentional loss of body weight and muscle mass, weakness, and progressive functional decline in individuals with cancer or other chronic diseases. It is estimated to affect 50 percent to 80 percent of cancer patients and is associated with reduced treatment tolerance, diminished quality of life, and shorter survival. Cachexia accounts for approximately 20 percent of all cancer-related deaths and is widely recognized as an indicator of poor prognosis (884)Stone BV, et al. (2024) Eur Urol Oncol, 7: 563.(885)Setiawan T, et al. (2023) J Hematol Oncol, 16: 54.. Despite its severity, there are currently no FDA-approved treatments for cachexia. However, emerging research has provided important insights into the biological mechanisms underlying the condition and opened the door to potential therapies.
A recent clinical trial found that ponsegromab, a drug designed to block a protein linked to weight loss in cancer, significantly improved body weight, appetite, and physical activity in patients with advanced cancer (886)Groarke JD, et al. (2024) N Engl J Med, 391: 2291.. In addition, new evidence has shown that inflammation-related changes in the brain may play a central role in fatigue and loss of motivation often seen in patients with cachexia. Specifically, researchers found that elevated levels of the inflammatory molecule interleukin-6 can disrupt brain functions involved in motivation and energy and leading to symptoms like apathy and fatigue (887)Zhu XA, et al. (2025) Science, 388: eadm8857.. These findings suggest that targeting inflammation in the brain may improve quality of life for patients living with cachexia.
Cancer-related cognitive impairment (CRCI), often referred to as “chemo brain,” includes difficulties with memory, attention, response time, and executive function that can occur before, during, or after cancer treatment. According to a recent analysis, nearly 70 percent of cancer patients reported cognitive symptoms of any severity, and more than 30 percent reported moderate to severe cognitive difficulties. Furthermore, cognitive difficulties were strongly associated with fatigue, depression, anxiety, and other debilitating symptoms (888)Mayo SJ, et al. (2024) JAMA Netw Open, 7: e2430833.. CRCI is often considered a consequence of psychological distress related to cancer or its treatment. Emerging evidence suggests that CRCI may contribute to the development and persistence of various psychiatric conditions, including mood or anxiety disorders (889)Haywood D, et al. (2024) Support Care Cancer, 32: 480..
Immune checkpoint inhibitors (ICIs) are a form of immunotherapy that are increasingly used to treat a wide range of cancers (see Releasing the Brakes on the Immune System). While ICIs have revolutionized cancer care and improved patient survival, their use has been associated with a distinct range of side effects known as immune-related adverse events (irAEs). These irAEs result from overactivation of the immune system and can affect any organ system. A recent analysis found that irAEs occur in approximately 40 percent of patients receiving ICI therapy, with commonly affected systems including the skin, endocrine organs, gastrointestinal tract, lungs, heart, and kidneys (625)Jayathilaka B, et al. (2025) Br J Cancer, 132: 51.. IrAEs can occur shortly after treatment begins or even months to years after treatment initiation (890)Durbin SM, et al. (2025) JAMA Netw Open, 8: e252668.. While many irAEs are mild and manageable, others, such as myocarditis (inflammation of the heart), can be severe or life-threatening and may require treatment discontinuation (891)Johnson DB, et al. (2022) Nat Rev Clin Oncol, 19: 254.. With the increased use of ICIs leading to long-term survival, a better understanding of their long-term and late effects is necessary.
Psychosocial Challenges
A cancer diagnosis can pose serious challenges to an individual’s mental and emotional well-being. Survivors commonly face a range of psychological challenges, including anxiety, fear of recurrence, uncertainty about the future, difficulty resuming work or daily routines, changes in relationships, and social isolation (892)Ge MW, et al. (2025) Psychooncology, 34: e70077..
Loneliness is an increasingly common and concerning issue among cancer survivors. Recent research indicates that more than one in three survivors in the United States experience moderate to severe loneliness, particularly those with poor physical or mental health, financial hardship, or limited social support (893)Wheldon CW, et al. (2025) Sci Rep, 15: 3914..
Survivors are particularly vulnerable to emotional distress, especially in the early years following diagnosis. Many report concerns about the physical symptoms of cancer and its treatment, their emotional well-being, communication with the care team, as well as challenges about intimacy and relationships (894)Brick RS, et al. (2024) J Cancer Surviv.. Anxiety and depression are highly prevalent among cancer survivors, who also face a greater risk of suicide than the general population (895)Hu X, et al. (2023) JAMA Netw Open, 6: e2251863.. Encouragingly, a recent analysis found that suicide rates among individuals with cancer have declined steadily over the past several decades, with the largest decrease occurring within the past decade (896)Liu Q, et al. (2024) Transl Psychiatry, 14: 213.. The decline in suicide deaths among survivors may be attributable to advances in cancer treatments, increased availability and integration of psychosocial support and palliative care services, and more effective management of cancer-related symptoms and distress. However, these trends have not been uniform across all groups, as suicide rates among adolescents and young adults (AYAs) have increased in recent years (897)Matsuo K, et al. (2024) JAMA Netw Open, 7: e2442964..
Financial Challenges
Financial toxicity, the economic hardship resulting from cancer diagnosis and treatment, remains one of the most pressing challenges facing cancer survivors today. One analysis found that more than half (56 percent) of individuals with cancer experience catastrophic health expenditures, defined as out-of-pocket medical costs that exceed a substantial portion of household income (898)Kitaw TA, et al. (2025) BMJ Glob Health, 10.. These financial burdens often persist for years after treatment ends, significantly impacting long-term survivorship.
Many survivors face ongoing out-of-pocket expenses for follow-up care, prescription medications, and medical equipment. A recent analysis found that US cancer survivors incur an average of $644 annually in out-of-pocket expenses for medical services, such as prescription drugs, medical equipment, outpatient care, occupational therapy, hospitalizations, and other related costs (899)Jafri FI, et al. (2025) JAMA Netw Open, 8: e2455941.. These costs are compounded by income loss, reduced work capacity, and difficulty returning to employment. According to a recent survey of long-term survivors, 75 percent reported income loss and/or extra expenses. The percentage of respondents who said they were unable to make ends meet increased from 2 percent before diagnosis to 13 percent after diagnosis (900)Klok JM, et al. (2024) J Cancer Surviv..
The financial burden of cancer is not experienced equally; certain groups are disproportionately affected. A recent study found that cancer survivors from lower-wealth households incurred higher financial debt and refinanced their homes more often compared with those without cancer (901)Hussaini SMQ, et al. (2024) JCO Oncol Pract: OP2400116.. Another study found that survivors residing in socioeconomically disadvantaged communities were more likely to report financial hardship, regardless of insurance status (902)Dhir A, et al. (2024) JAMA Netw Open, 7: e2429286..
Cancer-related financial hardship is associated with numerous adverse health consequences, including delayed or foregone care, decreased adherence to medications, poorer mental health, and higher mortality risk (903)Chen MH, et al. (2025) JCO Oncol Pract, 21: 78.. In response, oncology practices are increasingly implementing screening processes to identify financial distress and unmet social needs. However, many practices lack the capacity to adequately address patients’ financial needs. A recent survey of US community oncology practices found that while most practices had a financial screening process, only half had a financial navigator dedicated to assisting cancer patients. Notably, practices serving higher proportions of racial and ethnic minority patients were less likely to screen for financial concerns and less likely to have a financial navigator (904)McLouth LE, et al. (2021) Cancer Epidemiol Biomarkers Prev, 30: 669..
One promising approach to address these challenges is the Financial Toxicity Tumor Board (FTTB), first implemented at a large health care system in 2019 (905)Raghavan D, et al. (2021) JCO Oncol Pract, 17: e1433. Modeled after traditional tumor boards—which convene multidisciplinary teams of physicians and specialists to collaboratively review complex cancer cases—the FTTB brings together clinical, administrative, and supportive services to identify and resolve financial barriers to care. The FTTB includes a pharmacy-led patient assistance program, which systematically evaluates patients for eligibility in copay assistance and free drug programs, helping to reduce or eliminate out-of-pocket costs for cancer treatment. Over its first 5 years, the FTTB resolved 94 percent of cases presented and facilitated more than $400 million in patient financial assistance through its pharmacy-based program (906)Knight TG, et al. (2025) J Natl Compr Canc Netw, 23: 164.. Given its success, the FTTB offers a replicable model that can be adapted by other cancer centers to reduce financial hardship and improve equity in cancer care.
Addressing the Unique Challenges Faced by Vulnerable Populations
Challenges Faced by Children
In 2025, an estimated 9,950 US children under the age of 15 will be diagnosed with cancer. Thanks to advances in treatment, the 5-year survival rate for children diagnosed with cancer now exceeds 85 percent (2)Siegel RL, et al. (2025) CA Cancer J Clin, 75: 10.(9)Wagle NS, et al. (2025) CA Cancer J Clin.. This is a marked improvement compared to the mid-1970s, when only 58 percent of children lived beyond 5 years after a cancer diagnosis. Because childhood cancer survivors are diagnosed at a young age, they live longer after diagnosis than an adult who has been diagnosed with cancer.
The type and severity of long-term and late effects experienced by childhood cancer survivors depend on several factors, including the cancer type and stage at diagnosis, the specific type of treatment and doses received, and the survivor’s age and overall health at the time of treatment. Among these late effects, the development of new, secondary cancers is of particular concern (872)Wang Y, et al. (2025) J Transl Med, 23: 355.. For example, childhood cancer survivors are more than twice as likely to develop melanoma in adulthood compared to individuals without a cancer history (907)Rotz SJ, et al. (2025) J Clin Oncol, 43: 1219..
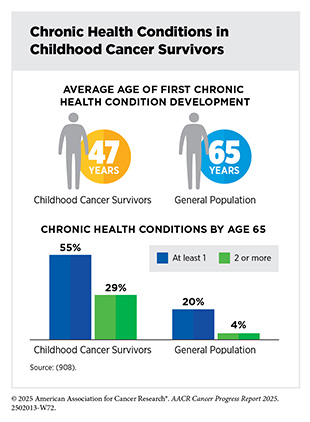
Survivors of childhood cancers are also at an increased risk of developing chronic, age-related health conditions earlier in life. These include cardiovascular disease, stroke, and other cancers. Some of these risks are influenced by inherited genetic mutations and by treatment-related changes to how genes function over time (see Genetic Alterations and Epigenetic Changes) (872)Wang Y, et al. (2025) J Transl Med, 23: 355.. A recent study estimated that childhood cancer survivors are nearly three times more likely to develop a serious age-related chronic health condition before age 65, with onset of these conditions appearing nearly 18 years earlier than in the general population (908)Yeh JM, et al. (2025) JAMA Oncol, 11: 535..
Despite these risks, some long-term complications may be mitigated through protective strategies. For instance, anthracyclines, chemotherapy drugs commonly used in childhood cancer treatment, are known to increase the risk of cardiomyopathy, a disease of the heart muscle that makes it harder for the heart to pump blood effectively. However, new research shows that dexrazoxane, a cardioprotective agent given alongside anthracyclines, may help preserve heart function for up to 20 years following treatment (909)Chow EJ, et al. (2023) J Clin Oncol, 41: 2248..
Cancer and its treatments can also disrupt cognitive development and academic performance. A recent study found that individuals diagnosed with central nervous system tumors in early childhood experienced slower development of academic readiness skills, particularly in reading, which was associated with poorer academic outcomes later in life (910)Somekh MR, et al. (2024) J Natl Cancer Inst, 116: 1952..
Childhood cancer survivors also experience lasting psychological and emotional challenges that persist well into adulthood. Fear of cancer recurrence is common. A recent study found that nearly one-third of adult survivors of childhood cancer reported elevated fear that their cancer could return or that they could develop a new cancer. This fear was strongly associated with symptoms of anxiety and depression, as well as reduced quality of life (911)Pizzo A, et al. (2024) JAMA Netw Open, 7: e2436144.. Mental health concerns also include a heightened risk of suicidal ideation, or suicidal thoughts. According to one analysis, approximately 10 percent of childhood cancer survivors reported experiencing suicidal thoughts, especially during active treatment. Although childhood cancer survivors were more likely to report suicidal thoughts, their risk of suicide death was comparable to that of individuals without a cancer history (912)Tan JY, et al. (2025) JAMA Netw Open, 8: e2457544..
Challenges Faced by Adolescents and Young Adults
AYA cancer survivors are those diagnosed between the ages of 15 and 39. An estimated 2.1 million AYA cancer survivors were living in the United States as of 2020 (874)American Cancer Society. Cancer Treatment and Survivorship Facts and Figures 2022-2024. Accessed: June 10, 2025.. On the basis of estimates of new cancer cases in 2025, AYAs will account for 4.2 percent of all new cases, and approximately 87 percent are expected to live 5 years or more after their diagnosis (2)Siegel RL, et al. (2025) CA Cancer J Clin, 75: 10.(916)NCI Childhood Cancer Data Initiative. NCI NCCR*Explorer. Accessed: June 15, 2025..
Many AYA survivors experience long-term and late effects, including increased risks of cardiovascular disease, metabolic disorders, cardiomyopathy, diabetes, and other chronic conditions (917)Armenian SH, et al. (2024) J Clin Oncol, 42: 735.(918)Cromie KJ, et al. (2025) Diabetes Care, 48: 519.. One study found that 40 percent of AYA cancer survivors had two or more chronic health conditions 10 years after their cancer diagnosis, compared to only 20 percent among those without a cancer history (919)Chao C, et al. (2020) Journal of Clinical Oncology, 38: 3161.. Similar to childhood cancer survivors, AYA cancer survivors also have a higher risk of secondary cancers, likely due to accelerated aging (876)Sung H, et al. (2022) J Natl Cancer Inst, 114: 1095.(917)Armenian SH, et al. (2024) J Clin Oncol, 42: 735.(920)van der Meer DJ, et al. (2024) Oncologist, 29: e526..
Recent evidence also highlights reduced kidney function as a significant long-term risk in children and AYAs who receive certain treatments, such as chemotherapy or abdominal radiation. International guidelines now recommend routine surveillance for kidney dysfunction in children and AYA survivors to enable early detection and reduce the risk of chronic kidney disease (921)Kooijmans ECM, et al. (2025) J Clin Oncol: JCO2402534..
Fertility and reproductive health remain significant concerns for AYA survivors. Depending on the cancer type and treatment regimen, risks of infertility can be high, prompting many to consider fertility preservation options before treatment (see Sidebar 49). Participation in fertility preservation and the type of preservation should be decided by individuals after discussions with their health care providers. Among those who do become parents, AYA survivors face increased risks of adverse birth outcomes, including having children born preterm and/or with low birth weight (922)Anderson C, et al. (2024) JNCI Cancer Spectr, 8.(923)Murphy CC, et al. (2025) J Natl Cancer Inst, 117: 1008..
Mental health challenges among AYA survivors are a growing area of concern. Studies consistently show that this population experiences higher rates of depression, anxiety, post-traumatic stress, and other psychiatric disorders, not only in the years immediately following diagnosis but well into adulthood (926)McGrady ME, et al. (2024) J Clin Oncol, 42: 707.(927)Zhang A, et al. (2025) JAMA Netw Open, 8: e2511430.. Alarmingly, suicide rates among AYA survivors have increased significantly over the past two decades, with male AYAs experiencing the steepest rise compared to survivors in other age groups (897)Matsuo K, et al. (2024) JAMA Netw Open, 7: e2442964..
For AYAs, a cancer diagnosis often coincides with a time in life when many are completing their education or establishing careers, making them particularly vulnerable to the economic disruptions caused by cancer. Nearly half of AYA blood cancer survivors report severe or high levels of financial distress, including difficulty paying bills and delaying or forgoing medical care due to cost (928)Parsons SK, et al. (2024) JNCI Cancer Spectr, 8.. A recent study found that about one in six AYAs with cancer experienced moderate to severe financial difficulty persisting for several years after diagnosis, suggesting these financial hardships can be long-lasting (929)Myers SP, et al. (2024) JAMA Netw Open, 7: e2446091.. Psychosocial challenges are also common among AYA survivors, who often report difficulty maintaining friendships, returning to school or work, and achieving key developmental milestones (926)McGrady ME, et al. (2024) J Clin Oncol, 42: 707..
Barriers to high-quality survivorship care and support services further compound these challenges. AYAs with cancer often face discontinuity in care as they transition between pediatric and adult-focused health care settings, neither of which is fully equipped to meet their unique developmental needs. As a result, many AYA survivors experience fragmented care, inconsistent follow-up, and poor continuity during care transitions (930)Marchak JG, et al. (2023) J Cancer Surviv, 17: 342.. Knowledge gaps about treatment history and late-effect risks, coupled with provider unfamiliarity with risk-based surveillance protocols, further impede access to appropriate long-term care (931)Ehrhardt MJ, et al. (2024) J Clin Oncol, 42: 743..
Despite considerable challenges, many AYA survivors demonstrate notable resilience, defined as the capacity to adapt and recover in the face of adversity. Interventions focused on mindfulness, stress management, and positive coping have been shown to foster psychosocial growth and improve mental health outcomes among AYA cancer survivors (932)Salsman JM, et al. (2024) Cancer, 130: 1031.. However, access to evidence-based psychosocial care for AYAs remains limited. Childhood and AYA cancer survivors continue to need developmentally tailored survivorship care that addresses the full range of physical, psychological, financial, and social challenges they may face during and long after treatment.
Challenges Faced by Older Adults
Older adults, defined as individuals age 65 and over, currently represent 64 percent of cancer survivors in the United States, and this proportion is projected to rise to 73 percent by 2040 (933)Bluethmann SM, et al. (2016) Cancer Epidemiol Biomarkers Prev, 25: 1029.. As the population of older adults with cancer grows, so does the need to understand and address the unique physical health challenges they face.
Among older individuals with cancer, frailty is commonly recognized as an early marker of accelerated aging and is strongly associated with poor health outcomes. In a recent study of older women with breast cancer, those who experienced persistent or worsening frailty following chemotherapy were more than twice as likely to die within 5 years as those with stable or improving strength (934)Duchesneau ED, et al. (2025) JAMA Netw Open, 8: e250614.. Cancer treatments can also accelerate bone loss, increasing the risk of falls and fractures. In a large population-based study, older adults with cancer had significantly higher rates of major osteoporotic and hip fractures than those without cancer (935)Rees-Punia E, et al. (2023) JAMA Oncol, 9: 79.. Recent evidence indicates that the Fracture Risk Assessment Tool—a widely used and validated fraction prediction tool—can accurately predict incident fractures in individuals with cancer, providing a valuable resource for early identification of skeletal health in this population (936)Ye C, et al. (2024) JAMA Oncol, 10: 1554..
It is estimated that over 90 percent of older adults with cancer have one or more chronic conditions, such as cardiovascular disease, hypertension, obesity, and diabetes, and over 30 percent have three or more comorbidities (937)Kleckner AS, et al. (2022) JCO Oncol Pract, 18: e9.(938)Williams GR, et al. (2018) Oncologist, 23: 433.. In the context of older survivors, pre-existing comorbidities can impact cancer treatment decisions and are associated with increased mortality and poor health outcomes (938)Williams GR, et al. (2018) Oncologist, 23: 433.(939)Chen W, et al. (2024) J Natl Cancer Inst, 116: 1730.. The presence of certain comorbidities also contributes to the elevated risk of developing second primary cancers. Diabetes, for example, affects nearly one-third of older breast cancer survivors and has been associated with an increased risk of developing second primary cancers of the liver, thyroid and brain (940)Hardell KNL, et al. (2024) JNCI Cancer Spectr, 8..
The high prevalence of comorbidities among older survivors often leads to polypharmacy, defined as the regular use of five or more medications. Polypharmacy affects up to 88 percent of older adults with cancer and is associated with adverse drug reactions, treatment toxicity, functional decline, hospital admissions, increased health care expenditures, and mortality (939)Chen W, et al. (2024) J Natl Cancer Inst, 116: 1730.(941)Mohamed MR, et al. (2023) Cancer, 129: 1096.(942)Oliveira RF, et al. (2024) BMC Geriatr, 24: 557..
While modern treatments have improved survival, they can damage healthy tissues and disrupt biological systems, leading to the premature onset of chronic age-related diseases, such as osteoporosis, cardiac dysfunction, secondary cancers, and frailty. This earlier onset of chronic diseases is often referred to as accelerated aging (943)Bhatia R, et al. (2022) Curr Oncol Rep, 24: 1401.(944)Guida JL, et al. (2019) J Natl Cancer Inst, 111: 1245.(945)Wang M, et al. (2024) J Clin Oncol, 42: 1553.. Although the concept of accelerated aging has been well-documented in childhood cancer survivors, a smaller but expanding body of literature is now focusing on older adults. Unlike younger populations, older adults are more likely to present with multiple comorbidities at diagnosis, making it challenging to disentangle the effects of aging, cancer, and its treatment on long-term health outcomes (944)Guida JL, et al. (2019) J Natl Cancer Inst, 111: 1245.(946)Locquet M (2025) Arch Gerontol Geriatr, 134: 105858.(947)Sedrak MS, et al. (2021) J Am Geriatr Soc, 69: 3077..
Researchers are investigating the therapeutic potential of anti-aging agents, such as senolytics and senomorphics, as clinical strategies to mitigate the effects of treatment-induced accelerated aging among survivors. In addition to pharmacologic strategies, incorporating geriatric assessments and aging biomarkers into survivorship research and clinical care could improve early detection of accelerated aging and inform supportive care interventions tailored to the unique needs of older survivors (948)Magnuson A, et al. (2024) CA Cancer J Clin, 74: 496.(949)Wang S, et al. (2024) Int J Mol Sci, 25..
Mental health conditions are common but often underrecognized in older adults with cancer. According to a recent report, one in three Medicare beneficiaries with cancer had a diagnosis of anxiety or depression (950)Birch K, et al. (2023) JCO Oncol Pract, 19: e660.. Social isolation also contributes to poor outcomes in this population. Research shows that older survivors experiencing severe loneliness face a 67 percent higher risk of death compared to those with little or no loneliness (951)Zhao J, et al. (2024) J Natl Compr Canc Netw, 22: 244..
Older cancer survivors are also vulnerable to financial challenges, even though most have health insurance through Medicare. Among older survivors treated with surgery, more than one in four reported financial hardship, such as borrowing money, going into debt, and/or delaying care due to cost. Notably, those experiencing financial hardship were also more likely to face transportation barriers that limited access to care, highlighting the compounding challenges older survivors face in navigating both the financial and logistical burdens of survivorship (952)Myers S, et al. (2025) Support Care Cancer, 33: 339.. The high and rising costs of cancer care further exacerbate these challenges. For example, Medicare beneficiaries receiving high-cost immunotherapy are more likely to report financial hardship than those receiving lower-cost treatments (824)Owsley KM, et al. (2025) J Cancer Surviv..
Financial strain can also affect basic needs. While the overall prevalence of food insecurity among older survivors is relatively low, those who incur catastrophic health expenditures are significantly more likely to experience food insecurity. For example, older survivors who spent more than 10 percent of their household income on out-of-pocket medical costs had 1.5 times higher odds of being food insecure (953)Pak TY (2025) Health Econ Rev, 15: 22.. These challenges highlight the urgent need to develop effective strategies to alleviate the financial burdens faced by older cancer survivors.
Improving Quality of Life and Health Outcomes
Maintaining a healthy lifestyle—through regular physical activity, a healthy diet, and eliminating alcohol and tobacco use—is one of the most effective strategies for reducing the risk of developing cancer and other chronic diseases (see Reducing the Risk of Cancer Development). These behaviors can also improve health outcomes and quality of life for cancer survivors. In fact, a growing body of evidence shows that adopting healthy behaviors after a diagnosis of cancer can significantly improve outcomes for patients (955)Giles C, et al. (2019) BMJ, 366: l5120.(956)Molenaar CJL, et al. (2023) JAMA Surg, 158: 572..
Participating in Physical Activity
Participating in physical activity is strongly associated with improved outcomes for cancer patients and survivors (957)Bai XL, et al. (2025) Br J Sports Med.. According to a recent study, those who met recommended physical activity guidelines (approximately 150 to 300 minutes of moderate activity per week) had a significantly lower risk of death across 10 cancer types (see Sidebar 18) (958)Rees-Punia E, et al. (2025) J Natl Cancer Inst.. Notably, even modest levels of activity may offer meaningful health benefits. For example, one analysis found that as little as 1 hour of aerobic exercise per week was associated with a 25 percent reduction in all-cause mortality among breast cancer survivors, while the greatest benefits were observed among those who met physical activity guidelines (959)Wilson OW, et al. (2025) Cancer Epidemiol Biomarkers Prev..
Physical activity can improve the immune system’s ability to detect and eliminate cancer cells. For example, a recent study in patients with esophageal cancer found that those who exercised while receiving chemotherapy had higher levels of immune cells within their tumors, indicating a stronger anti-tumor immune response (960)Rayner CJ, et al. (2025) J Sport Health Sci: 101063.. Engaging in physical activity during treatment may enhance the body’s ability to fight cancer, potentially improving treatment outcomes and reducing the risk of recurrence.
Physical activity can also help manage common treatment-related adverse effects. For example, neuromuscular training—a type of exercise that helps the nerves and muscles work together to enhance balance, coordination, and strength—has been shown to lower the incidence and severity of CIPN (962)Streckmann F, et al. (2024) JAMA Intern Med, 184: 1046.. Regular physical activity has also been associated with a reduced risk of lower extremity lymphedema among endometrial cancer survivors (963)Engh A, et al. (2025) Gynecol Oncol, 195: 82.. Lymphedema is a common late effect of cancer treatment that occurs when fluid builds up in the body, leading to swelling, usually in the legs and feet.
Tailored exercise programs are proving particularly effective in managing late effects. In a recent study, a personalized, remotely monitored exercise intervention improved physical function and reduced fatigue among individuals undergoing surgery for lung cancer (964)Ulrich CM, et al. (2025) JAMA Surg, 160: 495.. Similarly, prostate cancer survivors who participated in a supervised aerobic and resistance training program experienced significant improvements in both sexual function and muscle strength (965)Galvao DA, et al. (2025) JAMA Netw Open, 8: e250413..
Eating a Healthy Diet and Maintaining a Healthy Weight
Healthy diets that include fresh, minimally processed, plant-based foods are associated with improved outcomes among cancer patients and survivors. Among men with prostate cancer, adherence to a plant-based diet has been linked to reduced overall mortality, with greater benefits observed among Black survivors (967)Wang A, et al. (2025) JAMA Netw Open, 8: e2460785.. In contrast, diets high in ultra-processed foods and added sugars have been linked to worse outcomes. Colorectal cancer survivors who consumed higher levels of ultra-processed foods had a significantly increased risk of cardiovascular disease mortality, with specific foods like ice cream linked to higher colorectal cancer–specific mortality (968)Hang D, et al. (2024) EClinicalMedicine, 71: 102572.. Similarly, adult survivors of childhood cancer who regularly consumed sugar-sweetened beverages faced a greater risk of accelerated aging, reflected in a higher burden of chronic health conditions (969)Lan T, et al. (2024) Br J Cancer, 131: 1169..
Food insecurity, which is characterized by limited or uncertain access to adequate food, is a widespread issue that affects millions of Americans, including patients with cancer. A recent study found that approximately 10 percent of cancer survivors report food insecurity. Moreover, survivors with food insecurity have an increased risk of all-cause mortality compared to their food-secure counterparts (970)Lin JC, et al. (2025) JAMA Health Forum, 6: e251381.. Cancer survivors living in food deserts, or geographic areas with limited access to healthy and affordable food, face additional barriers to maintaining a healthy diet. Among cancer survivors residing in the US South, those with low socioeconomic status were more likely than higher-income individuals to live in food deserts and had to travel greater distances to access nutritious food options (971)Patel KB, et al. (2024) Gynecol Oncol, 188: 8..
Promoting healthy dietary patterns can help reduce treatment-related side effects, improve quality of life, and lower mortality risk among cancer survivors. For example, older cancer survivors who participated in a year-long, home-based vegetable gardening intervention—with monthly visits from professional gardeners and regular planting and maintenance activities—significantly increased their fruit and vegetable intake and experienced improvements in physical performance and perceived health compared to survivors who did not participate (972)Demark-Wahnefried W, et al. (2024) JAMA Netw Open, 7: e2417122..
Eliminating Alcohol and Tobacco Use
Smoking among cancer survivors is associated with adverse health outcomes, including increased risks of recurrence and secondary cancers, greater treatment-related complications, reduced quality of life, and higher mortality (973)Nolazco JI, et al. (2023) Front Oncol, 13: 1261041.(974)US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress A Report of the Surgeon General. Accessed: March 17, 2025.. However, 15 percent of cancer patients in the United States report being current smokers at the time of their diagnosis (196)Caturegli G, et al. (2025) JAMA Oncol, 11: 564.. The use of electronic cigarettes (e-cigarettes) has been on the rise in recent years, especially among younger cancer survivors (see Reducing the Risk of Cancer Development). In 2017, 27 percent of cancer survivors under age 50 used e-cigarettes compared to just 8 percent among survivors age 50 or older (975)Sanford NN, et al. (2019) JAMA Oncol, 5: 426.. Notably, over half of survivors who currently smoke traditional cigarettes also report using e-cigarettes (976)Lopez-Olivo MA, et al. (2024) J Cancer Surviv, 18: 1059.. According to one study, pain may be a contributing factor. Cancer survivors experiencing greater Group 8574, Grouped objectpain are significantly more likely to smoke cigarettes, including e-cigarettes (977)Powers JM, et al. (2025) Cancer, 131: e35701..
Given these patterns, promoting smoking cessation is critical. Quitting smoking can have immediate and long-term positive effects for cancer survivors. According to one study, individuals who stopped smoking within 6 months of a cancer diagnosis experienced significantly improved survival, gaining nearly two additional years of life compared to those who continued smoking (197)Cinciripini PM, et al. (2024) JAMA Oncol, 10: 1689..
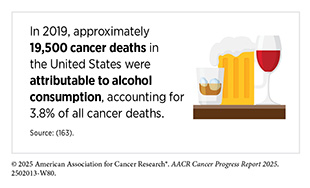
Consumption of alcohol can lead to adverse health and treatment outcomes among cancer patients and survivors, including increased risk of cancer recurrence, new malignancies, and mortality (978)Avancena ALV, et al. (2025) J Natl Compr Canc Netw, 23: 156.. Unfortunately, 71 percent of individuals with a history of cancer report consuming alcohol. Among those who drink, 46 percent exceed the upper limits defined in the guidelines (more than 1 drink per day for women or 2 for men; see Sidebar 19) and 32 percent engage in hazardous drinking (i.e., alcohol consumption that increases a person’s risk of harm) (979)Heffner JL, et al. (2024) Cancer Epidemiol Biomarkers Prev, 33: 600..
Although few alcohol interventions have been developed specifically for cancer survivors, care providers should refer patients with alcohol use disorder (AUD) to evidence-based treatments, such as behavioral counseling and/or medication. Despite their availability, treatment for AUD remains underutilized among cancer patients and survivors. A recent study found that among survivors newly diagnosed with AUD, only 14 percent initiated any form of treatment and fewer than 3 percent received FDA-approved AUD medications (980)Avancena ALV, et al. (2025) Ann Intern Med.. Integrating routine alcohol use screening into cancer care could significantly reduce the burden of avoidable cancer-related complications. As such, more research on intervention strategies specifically to reduce alcohol abuse in cancer survivors is warranted.
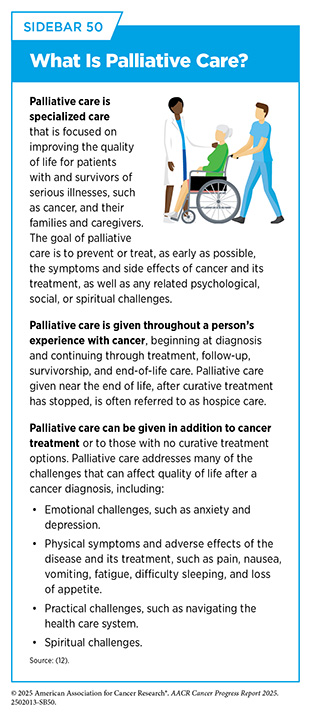
Integrating Palliative Care
Palliative care is an approach to prevent or manage the symptoms and side effects of any disease, including cancer, by addressing the physical, psychosocial, financial, and spiritual needs that arise from the disease and treatments (see Sidebar 50). Palliative care is facilitated by multidisciplinary teams of doctors, nurses, dieticians, pharmacists, therapists, spiritual leaders, and social workers, and has been shown to improve quality of life for patients, families, and caregivers (981)Kang E, et al. (2024) JAMA Netw Open, 7: e2426304.. Importantly, palliative care is appropriate at any stage of disease and can be provided alongside curative or life-prolonging therapies.
A growing body of evidence supports the early integration of palliative care, which has been associated with better symptom management, reduced depression and anxiety, improved coping, and better emotional well-being for both patients and families (982)Mah SJ, et al. (2024) JAMA Netw Open, 7: e2440977.(983)Petrillo LA, et al. (2024) Am Soc Clin Oncol Educ Book, 44: e100038.. Early palliative care can also help patients and caregivers navigate the uncertainty of modern cancer therapies, improve understanding of disease prognosis, and support care planning that aligns with patients’ goals, values, and preferences (983)Petrillo LA, et al. (2024) Am Soc Clin Oncol Educ Book, 44: e100038..
Individuals living with advanced or metastatic cancer face distinct survivorship challenges that require dedicated standards of care, including integrated models that reflect the reality of living longer with an incurable disease (984)Hart NH, et al. (2024) Support Care Cancer, 32: 313.(985)Jefford M, et al. (2025) Am Soc Clin Oncol Educ Book, 45: e471752.. Early referral to specialized palliative care is recommended for this population and has been shown to enhance quality of life, improve symptom management, and increase the likelihood of discussing and documenting end-of-life preferences (986)Sanders JJ, et al. (2024) J Clin Oncol: JCO2400542..
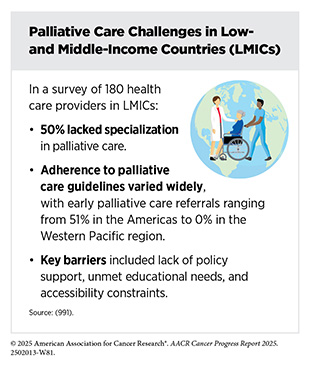
Despite these benefits, many patients with cancer still receive aggressive treatment near the end of life, which may not reflect their preferences, can compromise quality of life, and often contributes to emotional distress for both patients and their families. According to a recent study, nearly half of Medicare beneficiaries with advanced cancer received potentially aggressive care in the last 30 days of life, while only a minority received timely palliative care or participated in advance care planning (987)Kwon Y, et al. (2025) JAMA Health Forum, 6: e245436.. Early palliative care remains underutilized, in part due to a shortage of palliative care clinicians, underscoring the need for scalable, flexible models that expand access.
Stepped-care models are increasingly being used in oncology settings to deliver scalable, personalized care that is tailored to each survivor’s level of need. In general, the stepped-care model is an adaptive treatment framework in which all patients receive a baseline level of care, and treatment intensity is adjusted over time based on clinical need, treatment response, and patient preferences (988)Temel JS, et al. (2024) JAMA, 332: 471.. Research has shown that a stepped-care model for delivering palliative care to patients with advanced lung cancer can effectively improve patient outcomes and quality of life, while using fewer health care resources (988)Temel JS, et al. (2024) JAMA, 332: 471..
Recent national data from Commission on Cancer (CoC)–accredited institutions further highlight the need for integrated survivorship and palliative care models. In 2021, CoC introduced Standard 4.8, which requires accredited cancer centers to establish a structured survivorship program with a designated leadership team and dedicated services for patients who have completed treatment. A survey of over 380 CoC-accredited programs found that while most institutions offer core survivorship services, such as cancer screening, nutritional counseling, and specialist referrals, services addressing sexual health, fertility, and psychosocial needs remain underutilized (989)Stal J, et al. (2024) JAMA Netw Open, 7: e2418736..
Adult survivorship care is typically delivered by the cancer treatment team rather than through dedicated clinics, and only a minority of patients receive these services due to low referral rates and limited patient awareness. Experts emphasize embedding survivorship care into electronic health records (EHR), automating symptom alerts, and ensuring institutional commitment to sustainable staffing and funding (990)Nekhlyudov L, et al. (2024) JAMA Netw Open, 7: e2418686.. These efforts reinforce the broader imperative to treat survivorship and palliative care as continuous, complementary components of high-quality cancer care.
Improving Mental Health
The psychological challenges faced by survivors of cancer necessitate approaches that improve the mental well-being of this population. Several approaches can be utilized, including mind–body interventions, mental health screening, physical activity, and community engagement (966)Soong RY, et al. (2025) JAMA Netw Open, 8: e2457859.(992)Hahn EE, et al. (2022) JAMA, 327: 41.(993)Kulchycki M, et al. (2024) JAMA Netw Open, 7: e2437964..
A recent study outlined a stepped-care model for managing fear of cancer recurrence, in which all survivors receive universal psychoeducation (e.g., general information about recurrence risk, the nature of fear of recurrence, and basic coping strategies), followed by more intensive interventions (e.g., clinician-delivered psychotherapy) for patients with moderate or severe symptoms. The model emphasizes regular screening to guide care decisions, as well as flexible delivery formats (e.g., in-person, digital, or hybrid) to accommodate diverse survivor needs and health care settings (994)Smith A, et al. (2024) J Cancer Surviv..
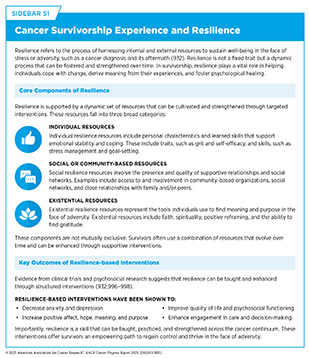
Despite the substantial distress associated with a cancer diagnosis and treatment, many survivors report experiencing personal growth or positive psychological change as a result of their diagnosis. Resilience, defined as the capacity to adapt and recover in the face of adversity, has emerged as a key protective factor for individuals facing cancer (932)Salsman JM, et al. (2024) Cancer, 130: 1031. (see Sidebar 51). Research has shown that resilience can mitigate the negative effects of depression and enhance quality of life for individuals with cancer (995)Caldiroli CL, et al. (2025) Sci Rep, 15: 8599..
Psychosocial interventions that focus on enhancing resilience by teaching skills, such as mindfulness, gratitude, goal-setting, and cognitive reframing, have shown promise in reducing distress and promoting long-term psychological well-being among individuals with cancer. Among AYAs with advanced cancer, resilience-focused interventions have been associated with increased hope and greater engagement in meaningful health care discussions, including those related to care preferences and goals (996)Rosenberg AR, et al. (2025) JCO Oncol Pract: OP2500161.. Importantly, these benefits were not only evident shortly after the intervention but were also sustained over time, suggesting a long-term impact on quality of life and mental health.
These findings underscore the importance of leveraging resilience in survivorship care. By integrating resilience-building strategies into routine oncology practice, providers can offer more holistic, patient-centered support that empowers individuals to navigate the emotional complexities of cancer with greater confidence and psychological strength.
Delivering Care to Cancer Survivors
Coordinating Care
The multifaceted approach to treating cancer necessitates providing survivors with appropriate care to address their many needs, including transitioning from active treatment, coordinating follow-up appointments, addressing financial and psychosocial challenges, and gaining access to other survivorship resources. While many of these services exist, survivors often face difficulties navigating the health care system to find and utilize them. Effective coordination of care is essential to help survivors identify and access the resources they need to maintain their health and well-being.
Coordinating cancer care is most effective when a designated individual or a team of people helps a cancer patient or survivor gain access to the resources they need. Patient navigators and clinical care coordinators are individuals who help cancer patients and survivors access resources more effectively (see Sidebar 52). Evidence from a recent study found that community-focused patient navigation programs helped increase trust in health care providers, reduced system-level barriers, and improved continuity of care, particularly among medically underserved populations (999)Ver Hoeve ES, et al. (2024) BMC Health Serv Res, 24: 550.. One such program, the Integrated Cancer Care Access Network (ICCAN), is a multidisciplinary initiative that provides one-on-one, culturally- and linguistically-tailored navigation and assistance with essential needs, such as food, housing, and financial support, for underserved cancer patients. Research on ICCAN demonstrated that patients who received these services experienced significantly higher treatment completion rates and greater improvements in quality of life, depression, and stress compared to those receiving standard care (1000)Gany F, et al. (2025) J Natl Compr Canc Netw: 1..
Survivorship care plans (SCPs) are another effective tool for improving care coordination. SCPs typically include a summary of the patient’s diagnosis and treatment, follow-up care recommendations, and guidance on managing long-term effects. SCPs serve as a critical bridge between oncology and primary care settings, promoting coordinated, continuous care as survivors transition out of active treatment. Recent studies have shown that patients who receive SCPs are more likely to adhere to recommended cancer screening guidelines across a range of cancer types (1001)Santos-Teles M, et al. (2024) Support Care Cancer, 32: 798.(1002)Tsai MH, et al. (2024) J Cancer Surviv, 18: 781.. Incorporating SCPs into EHRs can further improve care continuity by making survivorship information accessible across clinical teams. Several studies recommend integrating SCP templates into EHR systems to foster care coordination among oncologists, primary care providers (PCPs), and patients (1003)Atlas SJ, et al. (2025) JCO Oncol Pract, 21: 123.(1004)Singh AP, et al. (2025) JCO Oncol Pract, 21: 128..
Recognition of the critical role that PCPs play in cancer survivorship is growing, as they are well-positioned to manage comorbidities, deliver preventive care, and support long-term health and well-being. However, a recent study found that only 43 percent of cancer survivors maintained regular PCP visits 5 to 7 years after diagnosis (1005)Birken SA, et al. (2025) JCO Oncol Pract, 21: 766.. Younger survivors and those diagnosed with advanced-stage cancers were less likely to maintain PCP engagement compared to older survivors and those diagnosed at earlier stages, suggesting that these groups may be especially vulnerable to gaps in survivorship care and unmet health needs. Notably, survivors who remained engaged with an oncologist during this period were more than twice as likely to maintain regular PCP visits as those without ongoing oncology care, suggesting that stronger integration between oncology and primary care may help close critical gaps in long-term survivorship care.
Despite increasing recognition of survivorship as a distinct phase of the cancer continuum, the delivery of coordinated care remains inconsistent, and SCPs are still not routinely integrated into the standard practice (989)Stal J, et al. (2024) JAMA Netw Open, 7: e2418736.. To address these gaps, NCI, in collaboration with the Department of Veterans Affairs and other stakeholders, recently established national standards for cancer survivorship care (1006)Mollica MA, et al. (2024) J Cancer Surviv, 18: 1190.. These national standards are intended to guide the development of comprehensive survivorship programs across diverse settings and ensure that all survivors have access to high-quality, coordinated services.
However, meeting these standards will require addressing key workforce challenges. In addition to persistent shortages of oncologists and primary care providers, there are currently no accredited training programs in cancer survivorship, limiting efforts to standardize care and prepare the next generation of providers (1007)Manne S, et al. (2024) J Cancer Surviv, 18: 1.. Expanding access to survivorship services will require greater investment in training and supporting multidisciplinary care teams, including patient navigators, clinical care coordinators, and other professionals who are essential to delivering high-quality survivorship care.
Leveraging Patient Reported Outcomes
Patient reported outcomes (PROs), which are direct reports from patients about their health and daily functioning, are increasingly recognized as essential tools in clinical trials as well as routine practice (see Sidebar 53). PROs provide critical insights into symptoms, functional status, and quality of life, enabling a more comprehensive understanding of treatment tolerability and patient well-being (1013)Basch E, et al. (2024) JAMA, 332: 1979.(1014)Colbert JA, et al. (2025) JAMA Oncol, 11: 233..
PROs are collected through questionnaires, which alert clinicians to the status of the patient regarding quality of life, symptoms, and health-related behaviors (e.g., smoking, diet, and physical activity). When integrated into clinical care with automated alerts, these systems can prompt timely interventions by health care providers (1015)Rocque GB, et al. (2025) JAMA Netw Open, 8: e259852.. Evidence from large-scale trials shows that patients engaged in regular symptom monitoring experience better clinical outcomes, including improved symptom control, better quality of life, and fewer emergency department visits and hospitalizations (1016)Basch E, et al. (2025) Nat Med, 31: 1225.(1017)Dupuis LL, et al. (2025) JAMA Pediatr, 179: 11..
The integration of PROs with EHRs and real-time alert systems has proven both feasible and effective across diverse clinical settings. In a recent clinical trial, EHR-integrated PRO systems not only supported more responsive care but also improved communication between patients and providers (1016)Basch E, et al. (2025) Nat Med, 31: 1225..
Despite the clear benefits, barriers to widespread adoption of PROs remain, including clinician skepticism, technological limitations, workflow integration challenges, and disparities in digital access and literacy. Overcoming these barriers will require coordinated efforts to invest in user-friendly technology, provide training for clinicians and patients, streamline integration into clinical workflows, and ensure equitable access to digital tools across diverse patient populations (1014)Colbert JA, et al. (2025) JAMA Oncol, 11: 233..
Incorporating PROs into standard cancer care represents a meaningful step toward more patient-centered, responsive, and effective cancer care. As the evidence grows, particularly in pediatric populations, the integration of PROs should be prioritized to ensure that the patient voice is central to care delivery.
Supporting Caregivers
Caregivers comprise family members and/or friends who help patients with long-term chronic illness and manage any and all aspects of their care. In 2020, over 53 million US adults provided care for another person (1018)National Partnership for Women and Families. Paid Leave Could Keep More Than 6 Million Caregivers Connected to the Labor Force by 2030. Accessed: March 26, 2025.. Among them, an estimated four million were caring for an adult with cancer.
Caregivers are vulnerable to a range of adverse health outcomes. One study found that first-degree relatives and spouses of patients with genitourinary cancers had a 10 percent increased risk of developing a psychological illness and a 28 percent increased risk of cardiovascular disease (1019)Choudry MM, et al. (2024) Cancer, 130: 4061.. Other studies indicate that between 15 percent and 40 percent of cancer caregivers meet criteria for clinically significant traumatic stress or depression (1020)Klekovkina E, et al. (2025) Archives of Gerontology and Geriatrics Plus, 2: 100141. The emotional demands of caregiving are especially challenging for spouses of cancer patients, who face elevated risks of both suicide attempt and suicide death, especially within the first year after diagnosis (1021)Liu Q, et al. (2024) JAMA Oncol, 10: 1323..
Cancer survivors who also serve as caregivers face additional burdens. A national survey found that nearly one in five cancer survivors reported having caregiving responsibilities. These survivors were more than twice as likely to experience moderate to severe psychological distress as those without caregiving duties (1022)Mahmood A, et al. (2025) Support Care Cancer, 33: 75..
Emerging research highlights the interdependence of patient and caregiver experiences. In a study of breast cancer patients and their primary caregivers, nearly one-third of caregivers reported symptoms of depression, and financial toxicity was strongly linked to both the caregiver depression and the patient’s fear of cancer recurrence (1023)Yang T, et al. (2025) BMC Psychiatry, 25: 97.. Notably, the patient’s fear of recurrence also affected the caregiver’s emotional well-being, underscoring the shared and interconnected nature of distress within caregiving relationships.
Moreover, caregivers often face compounding social and financial challenges that exacerbate financial and emotional strain. These include housing and food insecurity, transportation barriers, job and/or academic disruptions, and unmet psychosocial needs. For example, employment disruptions, such as unpaid leave, job loss, or reduced hours, are common among caregivers, often resulting in loss of income and health insurance (1024)Anant S, et al. (2025) JCO Oncol Pract, 21: 41.. Recognizing the reciprocal nature of the patient– caregiver relationship is essential for delivering equitable, comprehensive, and person-centered oncology services.
Addressing caregiver needs through proactive screening for unmet needs, tailored psychosocial interventions, and financial support is critical to improving outcomes for both caregivers and the patients they support.
Enacted in more than 40 states, the Caregiver Advise, Record, and Enable (CARE) Act of 2016 requires hospitals to identify a caregiver for every patient and provide them with resources and training prior to releasing the loved one from the hospital. In 2022, the US Department of Health and Human Services released the National Strategy to Support Family Caregivers.
Developed through a multi-agency collaboration with private-sector partners, the strategy outlines more than 500 actions to strengthen caregiver support across five key areas: recognition and inclusion, access to services, financial and workplace protections, caregiver engagement, and data-driven policy development (1025)Administration for Community Living. 2022 National Strategy to Support Family Caregivers. Accessed: June 21, 2025.. Efforts to increase support for cancer caregivers are urgently needed because nearly a quarter of CoC-accredited US cancer centers do not have a family caregiver program (1026)Odom JN, et al. (2023) JAMA Netw Open, 6: e2337250..
Next Section: Envisioning the Future of Cancer Science and Medicine Previous Section: Transformative Advances in Blood Cancer