- Research: Driving Progress Against Cancer
- Cancer: An Ongoing Public Health Challenge
- Variable Progress among Cancer Types, Subtypes, and Stages of Diagnosis
- Disparities in Progress for Certain Population Groups
- The Growing Population Burden of Cancer
- Cancer: A Costly Disease. Research: A Vital Investment
Cancer in 2020
In this section, you will learn:
- In the United States, the overall cancer death rate has been steadily decreasing since the 1990s, with the reductions from 1991 to 2017 translating into more than 2.9 million cancer deaths avoided.
- The decline in the overall cancer death rate is being fueled in large part by a dramatic decrease in the lung cancer death rate predominantly as a result of reduced smoking rates.
- Since the 1990s, the age-adjusted overall cancer death rate has decreased more rapidly among African Americans than among whites; however, the African American population still disproportionately shoulders the burden of overall cancer mortality.
- The economic burden of cancer is enormous, both in the United States and globally.
Research: Driving Progress against Cancer
Research continues to be our best defense against cancer because it is the driving force behind all clinical and policy advances that improve cancer prevention, detection, diagnosis, treatment, and, increasingly, cures for individuals around the world.
Each advance that spurs progress against cancer is the result of many years of collaboration between different stakeholders dedicated to fundamentally changing the face of this devastating disease (see sidebar on Driving Progress against Cancer Together).
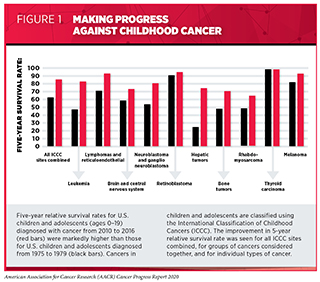
In the United States, the remarkable progress being made against cancer is illustrated by the fact that more children, adolescents, and adults are surviving longer after a cancer diagnosis. The U.S. 5-year relative survival rate for all cancers combined rose from 49 percent for people diagnosed in the mid-1970s to 70 percent for those diagnosed from 2010 to 2016 (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD [Internet]. [cited 2020 Jun 29].. The 5-year relative survival rate for all cancers diagnosed among U.S. children and adolescents (ages 0–19) from 2010 to 2016 was 85 percent, up from 63 percent for those diagnosed in the mid-1970s (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2 [Internet]. [cited 2020 Jun 29].(3)American Cancer Society. Cancer Facts and Figures 2014. (see Figure 1).
Another sign of the extraordinary progress being made against cancer in the United States is that the age-adjusted overall cancer death rate has been declining since 1991 (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;. The largest reduction in the U.S. age-adjusted overall cancer death rate ever seen in a single year, 2.2 percent, occurred from 2016 to 2017, which is the last year for which these data are available. Overall, since its peak in 1991, the rate has declined by 29 percent, a reduction that translates into more than 2.9 million cancer deaths avoided.
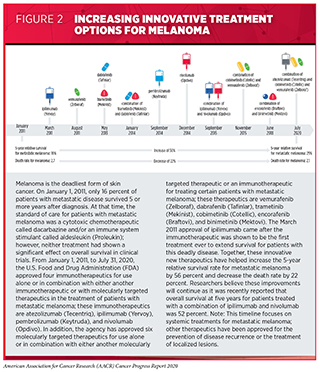
The decline in the U.S. age-adjusted overall cancer death rate has been fueled in large part by a dramatic decline in the lung cancer death rate predominantly as a result of reduced smoking rates (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;. The decline in the lung cancer death rate has accelerated in recent years, falling 2.4 percent each year from 2008 to 2013 and then falling 4.3 percent each year from 2013 to 2017. During the 2013 to 2017 period, the death rate for melanoma, which is the deadliest type of skin cancer, also fell at a remarkable rate of 6.4 percent each year (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;. This striking reduction has been attributed in large part to the innovative new therapeutics approved by the U.S. Food and Drug Administration (FDA) for treating certain patients with the disease since 2011 (see Figure 2)
As more and more new anticancer therapeutics are approved by the FDA and we continue to make scientific, clinical, and policy advances in cancer prevention, etiology, detection, diagnosis, treatment, and survivorship, we will accelerate the pace of progress against cancer. In this report, we focus on advances made during the 12 months from August 1, 2019, to July 31, 2020. Among the advances in cancer treatment that occurred during this period are the 20 new anticancer therapeutics approved by the FDA for introduction into the clinic. In addition, during this period, the FDA expanded the uses of 15 previously approved anticancer therapeutics to include additional types of cancer (see Progress across the Spectrum of Cancer Treatment.
Cancer: An Ongoing Public Health Challenge
Although we have made incredible progress against cancer, this disease continues to be an enormous public health challenge around the world (see sidebar on Cancer: A Global Public Health Challenge). In 2020, making further inroads against cancer has been further complicated by the Coronavirus Disease 2019 (COVID-19) pandemic, as discussed in COVID-19 and Cancer). As one example, it is estimated that there will be at least 10,000 additional deaths from breast cancer and colorectal cancer over the next decade in the United States as a result of the adverse effect of the COVID-19 pandemic on screening and treatment for these two types of cancer (10)Sharpless NE. COVID-19 and cancer. Science [Internet]. American Association for the Advancement of Science; 2020 [cited 2020 Jun 29];368:1290..
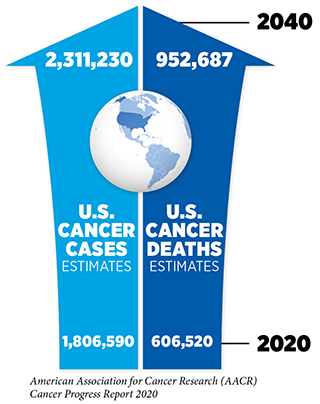
The public health challenge posed by cancer in the United States is illustrated by the fact that researchers project that there will be 1,806,590 new cases of cancer diagnosed in 2020 and that there will be 606,520 deaths from the disease (8) (see Table 1). These numbers translate into 206 new cancer cases and 69 cancer deaths every hour of every day.
Variable Progress among Types of Cancer, Subtypes of Cancer, and Stages of Diagnosis
Among the challenges we face is that progress against cancer has not been uniform for all types of cancer (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2 [Internet]. [cited 2020 Jun 29].. Nor has it been uniform for all subtypes and stages of a given type of cancer (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2 [Internet]. [cited 2020 Jun 29]..
These challenges are illustrated by the fact that the 5-year relative survival rates for U.S. patients vary widely depending on the type of cancer diagnosed, the subtype of the cancer diagnosed, and the stage at diagnosis (2)Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2 [Internet]. [cited 2020 Jun 29].. For example, the overall 5-year relative survival rates of 98 percent for men with prostate cancer and 85 percent for adults with chronic lymphocytic leukemia (CLL) stand in stark contrast to the overall 5-year relative survival rates of 18 percent for people with liver cancer and 25 percent for those with acute myeloid leukemia (AML). Among women with breast cancer, those diagnosed with the triple-negative subtype have a 5-year relative survival rate of 77 percent, while those with the hormone receptor-positive subtype have a 5-year relative survival rate of greater than 90 percent. Substantial variation in the 5-year relative survival rate is also seen for the two main subtypes of lung cancer; it is 24 percent among patients with non-small cell lung cancer (NSCLC) and 6 percent among those with small cell lung cancer. In addition, among women with endometrial cancer and adults with colorectal cancer, those whose cancer is confined to the uterus, or to the colon or rectum, have 5-year relative survival rates of 95 percent and 90 percent, respectively, while those whose cancer has metastasized have 5-year relative survival rates of 17 percent and 14 percent, respectively.
Developing new and effective tests for the early detection of more types of cancer could help address the challenge of variable progress between types of cancer because patients diagnosed when cancer is at an early stage, before it has spread to other parts of the body, have a much higher likelihood of long-term survival than those diagnosed when the disease has spread to distant sites, an occurrence known as metastasis.
Disparities in Progress for Certain Population Groups
Cancer health disparities are another pressing challenge posed by cancer, as highlighted in the AACR Cancer Disparities Progress Report 2020(14).
The National Cancer Institute (NCI) defines cancer health disparities as adverse differences in cancer measures such as number of new cases, number of deaths, cancer-related health complications, survivorship and quality of life after cancer treatment, screening rates, and stage at diagnosis that exist among certain population groups (15)Cancer Health Disparities Definitions – National Cancer Institute [Internet]. [cited 2019 Jun 19](see sidebar on U.S. Cancer Health Disparities).
Cancer health disparities are experienced by many segments of the U.S. population (see sidebar on Which U.S. Population Groups Experience Cancer Health Disparities?). The African American population is one group that has long shouldered a disproportionate burden of cancer (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;(18)(20)DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African Americans, 2019. CA Cancer J Clin [Internet]. 2019 [cited 2019 Feb 15];. For example, in 1993, the overall cancer death rate for African American adults was 33 percent higher than it was for white adults. Encouragingly, this disparity had narrowed to 17 percent by 2017, the last year for which these data are available, because the overall cancer death rate decreased more rapidly among African American adults than it did among white adults from 1993 to 2017. Another sign of progress toward eliminating disparities in outcomes between African Americans and whites is that there was a greater increase in 5-year cancer survival for African Americans compared with whites from 2011 to 2014 (21). As a result, the disparity in 5-year cancer survival for African Americans compared with whites narrowed from 8.2 percent to 7.7 percent during that period. Despite the progress, the burden of overall cancer mortality is still significantly higher among African Americans compared with whites (5)Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;(18)(20)DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African Americans, 2019. CA Cancer J Clin [Internet]. 2019 [cited 2019 Feb 15];(21).
Racial and ethnic minorities, including African Americans, not only shoulder a disproportionate burden of cancer, but also are shouldering a disproportionate burden of the ongoing COVID-19 pandemic, further highlighting stark inequities in health care. Disparities in health care are among the most significant forms of racial inequality and injustice, and it is imperative that everyone play a role in eradicating the social injustices that are barriers to health equity, which is one of our most basic human rights.
Identifying, quantifying, and understanding the causes of health disparities, including cancer health disparities, is a vital step toward developing and implementing strategies to eliminate these disparities. Current knowledge of the complex and interrelated factors that contribute to cancer health disparities is discussed in detail in the AACR Cancer Disparities Progress Report 2020 (14) (see sidebar on Why Do U.S. Cancer Health Disparities Exist?). For racial and ethnic minorities, adverse differences in many, if not all, of these factors are directly influenced by structural and systemic racism. New insights obtained through research, including basic research using samples from all U.S. population groups, through the participation of individuals from all these groups in clinical trials, and through increased collaboration among all stakeholders will allow us to make major strides toward eliminating cancer for all.
The Growing Population Burden of Cancer
The public health challenge posed by cancer will grow considerably in the United States and around the world in the coming decades unless we develop and effectively implement improved strategies for cancer prevention, early detection, and treatment (12)Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Tomorrow. Lyon, France: International Agency for Research on Cancer [Internet] [cited 2019 Jul 29]. (see sidebar on Cancer: A Global Public Health Challenge).
In the United States, it is predicted that the number of new cancer cases and the number of cancer deaths will rise to more than 2.3 million and almost 1 million, respectively, in 2040 (12)Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F (2018). Global Cancer Observatory: Cancer Tomorrow. Lyon, France: International Agency for Research on Cancer [Internet] [cited 2019 Jul 29].. These sharp increases over the current numbers are anticipated largely because of overall population growth and because the segment of the U.S. population that accounts for most cancer diagnoses—those age 65 and older (2)—is expected to grow from 56 million in 2020 to 81 million in 2040 (22)Bureau UC. 2017 National Population Projections Tables: Main Series. [cited 2020 Jun 30];.
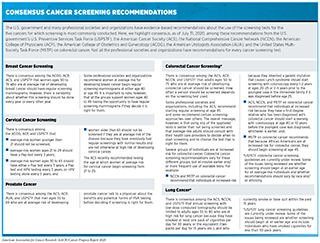
Cancer is primarily a disease of aging. In the United States, the median age at diagnosis is 66, and 54 percent of cancer cases are diagnosed in people age 65 and older (22)Bureau UC. 2017 National Population Projections Tables: Main Series. [cited 2020 Jun 30];. Progress is being made in reducing the overall U.S. cancer incidence rate, with the most recent data showing that it fell 0.6 percent each year from 2012 to 2016 (23). However, incidence rates for some types of cancer are increasing among people age 49 and younger at an alarming rate (24)Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;0:1–20.(25)A B, F S, R B. Prostate Cancer in Young Men: An Emerging Young Adult and Older Adolescent Challenge. Cancer [Internet]. Cancer; 2020 [cited 2020 Jun 30];126.. For example, the colorectal cancer incidence rate among people age 49 and younger increased 2.2 percent each year from 2012 to 2016 (24)Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin [Internet]. 2020;0:1–20.. This rise in early-onset colorectal cancer was driven largely by an increase in the colorectal cancer incidence rate among non-Hispanic whites. During the same period, the colorectal cancer incidence rate among those age 65 and older fell 3.3 percent each year. Similar trends have been seen for prostate cancer (25)A B, F S, R B. Prostate Cancer in Young Men: An Emerging Young Adult and Older Adolescent Challenge. Cancer [Internet]. Cancer; 2020 [cited 2020 Jun 30];126.. For both examples, younger people were more likely to be diagnosed when the cancer had spread to distant sites, data that are being considered as colorectal cancer screening guidelines are reviewed (see sidebar on Consensus Cancer Screening Recommendations for Average-risk Individuals).
Cancer: A Costly Disease
Research: A Vital Investment
The enormous toll of cancer is felt not only through the number of lives it affects each year, but also through its immense economic impact.
In the United States, it is estimated that cancer health care spending was $161.2 billion in 2017, the last year for which these data are available (26). This does not include the indirect costs of lost productivity due to cancer-related morbidity and death, which were $30.3 billion and $150.7 billion, respectively. Overall, these numbers translate to about 1.8 percent of the country’s gross domestic product.
The economic burden of cancer stands in stark contrast to the amount of money the federal government invests across all areas of medical research. In 2017, the same year that cancer health care spending was $161.2 billion, the budget for the National Institutes of Health (NIH), which is the largest medical research agency in the world, was just $34.15 billion, of which $5.64 billion went to the NCI.
If the number of cancer cases diagnosed each year in the United States increases in the coming decades as anticipated, the direct and indirect costs will also escalate (27)Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical Care Costs Associated with Cancer Survivorship in the United States. Cancer Epidemiol Biomarkers Prev [Internet]. American Association for Cancer Research; 2020 [cited 2020 Jun 30];.
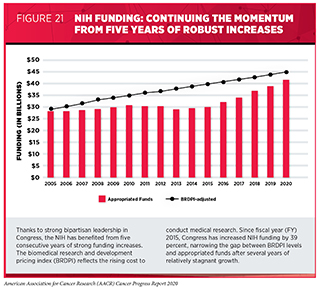
The increasing personal and economic burden of cancer highlights the vital need for more transformative research to accelerate the pace of progress. Recent advances, some of which are highlighted in this report, were made as a result of the cumulative efforts of researchers from a diverse array of specialties. Their work is supported in large part by funds from the federal government that are administered through the NIH. The consecutive multibillion dollar increases for the NIH budget from fiscal year (FY) 2016 to FY2020 have helped researchers keep up with the pace of scientific innovation (see Figure 21). It is imperative, however, that Congress continue to provide sustained, robust, and predictable increases in investments in the NIH and the NCI, as well as other federal agencies that are vital for fueling progress against cancer such as the FDA and the Centers for Disease Control and Prevention (CDC), in the years ahead (see The AACR Call to Action.)